Introduction
The syndemics theory posits that a “constellation of two or more afflictions can amplify the negative impact of one or more other health problems”1. The most frequent underlying psychosocial conditions that increase the risk of acquiring HIV and other sexually transmitted infections (STI) are drug and alcohol abuse, any experience of violence, and mental health problems 2. Epidemiologic studies have found that the risk of HIV infection 3 and the prevalence of STIs 4,5 increase as the number of those psychosocial conditions also increases. Some studies have also reported the synergistic effects of such psychosocial conditions. For instance, Tomori et al. 5 reported that the combination of alcohol dependence and illicit drug use increases the risk of active syphilis beyond their independent effects. Chakrapani et al. 6 found synergistic effects of violence and alcohol use as well as violence and depression on unprotected anal sex acts.
Colombia offers an interesting setting to examine the associations and interactions of syndemic conditions in the context of STIs. The HIV prevalence in Colombian groups at risk is high and comparable to that of other Latin-American countries 7: men who have sex with men (MSM), 5.6% to 24% 8,9; female sex workers (FSW), 0.6% to 3.5% 10; and transgender women (TW), 10% to 19% 11. HIV positivity in these groups has been associated with social adversities 12, previous experience of violence, serial forced displacement, early sexual initiation 9, substance abuse 8, and history of STIs 9. Additionally, there is a high prevalence of HIV and risky behaviors in heterosexual groups of low socioeconomic status 13,14. In these groups, the role of drug and alcohol use, and early sexual initiation on promoting the practice of unprotected sex has also been reported 13,15. Thus, it is essential to understand the accumulative and synergistic effects of the psychosocial factors to devise and plan the best possible HIV/STIs prevention strategies for these Colombian subpopulations.
The objective of this study is to examine the effect of alcohol misuse, poly-drug use, the experience of sexual violence, and early initiation of sexual activity (as a proxy of sexual abuse during childhood) on HIV positivity and self-reported STI history. We used data from an HIV testing and counseling campaign to reach a diverse population of TW, MSM, heterosexual men (HM), FSW and heterosexual women (HW) as access to HIV testing remains low in Colombia 16,17. We explored the following subjects: 1) the association of the accumulation of psychosocial factors with HIV positivity and history of STIs, and whether or not it was consistent with previous studies; 2) the synergistic effects (on an additive and multiplicative scale) of the presence of two syndemic conditions on both outcomes (HIV positivity and history of STIs), and; 3) the variation of these two outcomes with gender/sexuality, that is if the associations and interactions found are consistent in all groups. We were expecting a higher prevalence of syndemics in the MSM and TW groups versus the HM group, and in the FSW versus the HW groups. However, we hypothesized similar negative effects of the psychosocial factors on HIV positivity and STIs history in both highrisk and heterosexual groups.
Materials and Methods
Study Design: We used data from a crosssectional study conducted with a non-random sample of participants in Cali between 2013-2015, the largest city in South Western Colombia. Cali has a population of 2.3 millions, approximately 3.5% live in extreme poverty and 15% in poverty; by 2016, 11.8% were unemployed 18. The sample was recruited from among people who participated in an HIV testing and counseling campaign (HTC) rolled out by the Corporación de Lucha Contra el SIDA (CLS). CLS periodically runs such campaigns to identify subpopulations unaware of their HIV serostatus who may need medical attention 19. Briefly, the HCT campaign started by reaching out to community leaders who belong to the groups of interest included in this study: TW, MSM, and FSW. These leaders were instructed to invite individuals who could require health services. The invitees were referred to a local center where participants could access HIV counseling and point-of-care HIV tests. Study activities were conducted at 22 community centers, three sex work venues, and at the CLS clinic. At each site, research and clinical CLS personnel approached participants to complete a paper-based survey that was adapted from a previously published HIV behavioral surveillance instrument 20. The only exclusion criterion was being younger than 18 years old. This study was reviewed and approved by the Institutional Review Board of the CLS (IRB 00005732 of the U.S. DHHS; approval letter N° 022).
Psychosocial Conditions: We examined four psychosocial conditions: early sexual initiation as an indicator of child sexual abuse, the experience of forced sex with a partner in the past year, alcohol misuse, and poly-drug use. Participants were asked to report the age of their first sexual encounter; early sexual initiation was defined as ≤ 13 years old, which corresponds to the minimum age for legal sexual consent under Colombian law 21. Forced sex was defined as a positive answer to the following question: “During the last year, did any of your sexual partners force you to have sex with him (her), even though you did not want to do it?”. We evaluated alcohol misuse by asking participants about the frequency of alcoholic drinks in the last month and the number of drinks per day. Individuals were then classified into two categories: those who did not misuse alcohol (non drinkers, frequency ≤ 1 time per month) and those who did (binge and heavy drinkers). We assessed drug use by asking participants about the frequency of injectable and non-injectable drug use per week in the last six months. We inquired about marijuana, cocaine, crack, hallucinogens, heroin, amphetamines, and stimulants. We counted those drugs that were used at least once and classified individuals as non-users, users of one drug and poly-drug users if they used ≥ 2 drugs.
Covariates: The covariates included were age, educational level (the highest level reached), health insurance (i.e., affiliation to any health-care system), personal income (no income, < 1, 1-2, 3-5, and ≥ 5 minimum wages per month, which was USD$ 308 at the time of the survey), incarceration history, homelessness (i.e., living in the streets), and self-report of race/ethnicity (including white, afro Colombian, mestizo, and indigenous).
Dependent variable: 1) Assessment of HIV positivity serostatus. Half of the respondents were tested with the rapid qualitative immunoassay AKON® HIV 1/2/0 Tri-line (ACON Biotech (Hangzhou) Co. Ltd) and the other half with the DoubleCheckGold™ HIV 1&2 (Orgenics Ltd., Yavne, Israel) due to discontinuation of one of the former HIV test 22. A certified nurse technician collected the blood samples from the participants. In HIV-positive patients, a fourth-generation ELISA was performed (UMELISA- HIV, indirect enzymatic immunoassay that detects antibodies against HIV-1 and HIV-2 in human serum, plasma or dry blood spots. Centro de Análisis Molecular, Bogotá, Colombia). If the ELISA was not reactive, the screening test result was considered a false positive. Only one such a case was found. Those cases in which the ELISA was also reactive were then confirmed by a Western blot assay. 2) History of sexually transmitted infections. Self-reported STIs as “ever been told by a doctor or a nurse to have a sexually transmitted disease” were recorded.
Statistical Analysis: For comparison with previous publications, we examined the data in five steps, as previously described 23. First, we compared the social and psychosocial conditions across the gender/sexuality groups. Second, we applied bivariate and multivariate models to test the effect of each psychosocial condition and their co-occurrence on both outcomes. A syndemic index was created by summing the presence of the studied psychosocial conditions, with an overall score ranging from 0 to 4. The highest category was re-defined as ≥ 3 because of the conditions’ low frequency. A summative or cumulative effect of those conditions would be present if a gradient was observed across the categories of the index. Then, Poisson regression was used to examine the univariate and multivariate associations and to calculate the prevalence ratio (PR). Finally, we tested the additive and multiplicative interactions between six combinations of exposures on each outcome as follows: 1) forced sex and early sexual initiation; 2) forced sex and alcohol misuse; 3) forced sex and drug use; 4) early sexual initiation and alcohol misuse; 5) early sexual initiation and drug use, and; 6) alcohol misuse and illicit drug use. For the additive interactions, we calculated the relative excess risk due to interaction (RERI); a positive RERI suggests that the co-occurring conditions confer a higher risk of HIV/STIs than expected, beyond the independent effects of the conditions 24. The interaction module ICP was used to obtain the significance of RERI at the 95% level. Data were recorded using Microsoft Access software 2010 with consistency checks and the STATA/IC 12.1 (Stata Corp LP, Texas, USA) was used for all analyses.
Results
In this study, 812 and 525 were male and female at birth, respectively. Among those with male sex at birth, 54.7%, 7.3%, and 38% self-identified as MSM, TW, and HM, respectively. Among those with female sex at birth, 19% and 81% self-identified as FSW and HW, respectively. TW, MSM and HM groups differed on several social characteristics, being social adversities more frequent among transgenders (Table 1). Additionally, we observed a high prevalence of psychosocial conditions in the sample studied: 298 (22.5%), 510 (38.2%), and 312 (23.5%), 62 (4.6%), participants reported early sexual initiation, alcohol misuse, polydrug use, and forced sex, respectively. Specifically, the TW and FSW groups showed the highest frequency of psychosocial conditions across men and women, respectively.
Table 1 Sociodemographic characteristics, syndemic conditions and frequency of HIV and STIs, overall and specific group descriptions. Cali-Colombia 2013-2015.
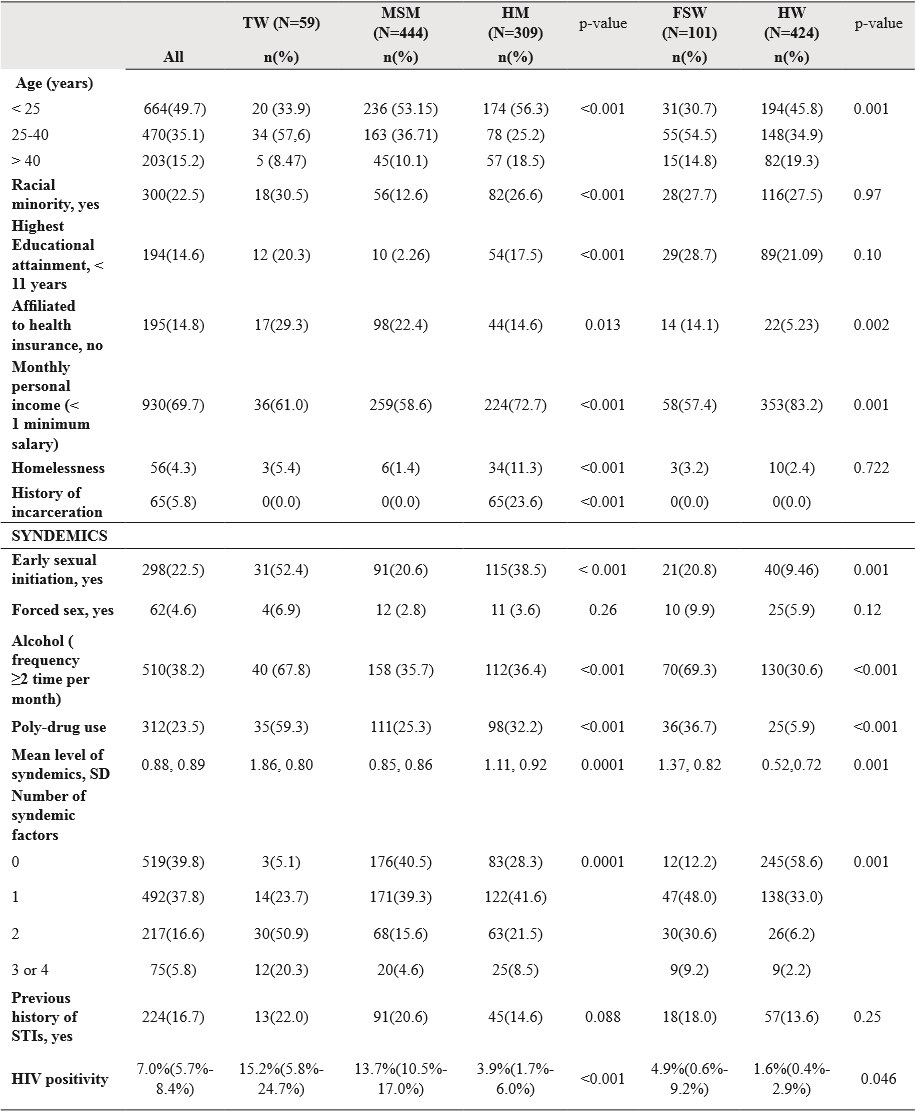
SD: standard deviation.
Source: Author elaboration.
A total of 94 out of 1337 (7%) participants were HIV positive by the rapid test, and 224 out of 1337 (16.7%) reported being diagnosed with an STI at least once in their life. Regarding HIV positivity, no differences were observed between the MSM and TW groups (PR=0.90 CI 95%:0.47-1.72), but both showed a higher risk than the HM group (TW, PR=3.93, CI 95%: 1.73-8.90; MSM, PR=3.53, CI 95%: 1.94-6.46). Additionally, FSW were more likely to be HIV positive than the HW (PR=2.99, CI 95%: 0.97-9.26). Compared to HM, MSM (PR=1.41, CI 95%: 1.02-1.95) and TW (PR=1.51, CI 95%: 0.87-2.62) were also more likely to report previous STIs, but the FSW and HW groups showed similar STI prevalence (PR=1.33, CI 95%: 0.82-2.15) (data not shown).
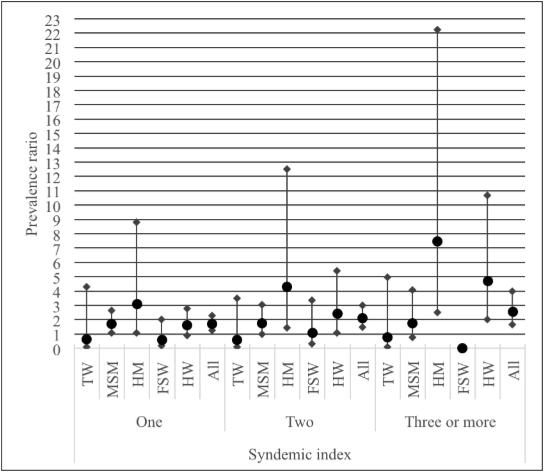
In the univariate and multivariate analyses, poly-drug use was the only psychosocial factor related to HIV positivity (Table 2). Neither in the whole sample nor in the subgroup analysis, was the syndemic index related to HIV positivity. In contrast, each of the psychosocial conditions independently and the syndemics index was related to a higher likelihood of a history of STIs (Table 2); the linearity test was significant (p<0.001). While the syndemic index was not related to the STI history in the TW and FSW groups, it was related in the other three groups: MSM, HM, and HW (Figure 1).
Table 2 Poisson regression of syndemics on HIV and STIs. Cali-Colombia 2013-2015.
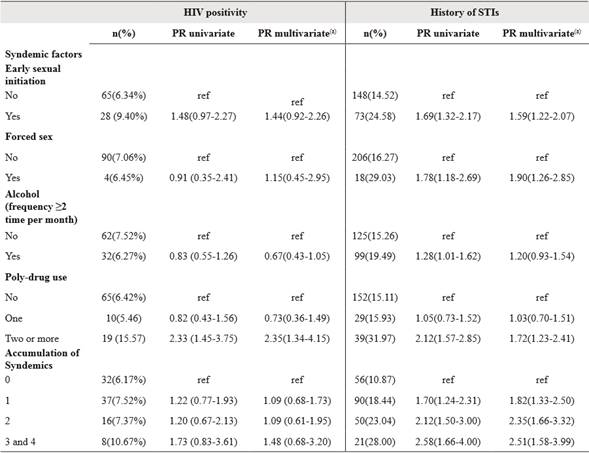
Adjusted by age, income, education, homelessness, ethnicity. Ref: category of reference. PR: prevalence ratio.
Source: Compiled by author.
Source: Compiled by author.
Figure 1 Syndemic index by groups according to Previous STIs (PR and IC95%). Cali-Colombia 2013-2015.
In the case of HIV positivity, positive RERIs were found for forced sex and poly-drug use, and polydrug use and alcohol misuse (Table 3), but none of the RERI or multiplicative interactions was significant. In the case of STI history, positive RERIs were found for forced sex and early sexual initiation, and for forced sex and poly-drug use.
Table 3 Poisson regression analysis and Additive interactions. Analysis unadjusted for other covariates. Cali-Colombia 2013-2015.
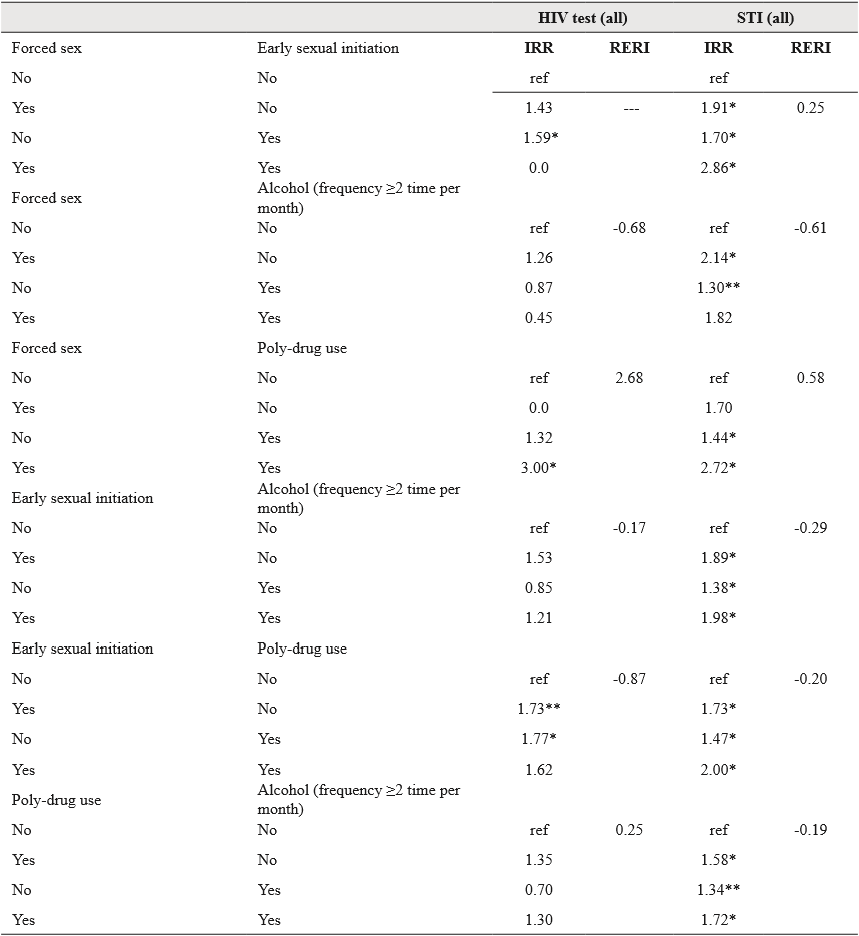
A RERI = 0 means no interaction; RERI > 0 means positive interaction or more than additivity; RERI < 0 means negative interaction or less than additivity; *p-value<0.05; **0.05<p-value<0.10. Ref: category of reference.
Source: Compiled by author.
In the HM and HW groups, there were significant combination effects of psychosocial conditions on STIs (data not shown), but again the RERIs were not significant. The multiplicative interactions tested (n=6) were also not significant for HIV positivity or STI history (data not shown).
Discussion
Main findings
In this study, we explored in HIV high-risk subpopulations in Colombia, the effect of four psychosocial factors (early sexual initiation, forced sex, alcohol misuse, and illicit drug use) on HIV positivity and history of STIs. The exposure to psychosocial conditions was higher in the TW group compared to the other groups, which is consistent with high life-course exposure of TW to structural and interpersonal adversities 25. Our results further indicate that the frequency of psychosocial conditions is not negligible in the heterosexual populations, especially in those living with social deprivations associated with homelessness and lack of health insurance.
In this sample, poly-drug use, rather than the accumulation of syndemics, drives HIV infection. This is consistent with other Colombian studies which also have found that the risk of HIV is associated with drug use 8,9. According to the minority stress theory, drug abuse may represent a way to cope with lifetime interpersonal stressors, sexual violence, and discrimination, leading to unprotected sex practice and consequent higher HIV risk 26. We could also hypothesize that poly-drug use is a mediator between early sexual initiation and both the risky behaviors and HIV 27.
The lack of association between the accumulation of syndemic conditions and HIV was also described in a longitudinal analysis of youth MSM 28 but showed significant associations with drug use. However, other studies conducted only in MSM reported the co-occurrence of psychosocial conditions and HIV incidence, HIV positivity, and self-reported cases 29,30. To our knowledge, there is no other study on the syndemic effects on HIV or STIs acquisition among TW or FSW; most of the studies involving TW groups analyzed the effect of syndemic factors on high-risk sexual behaviors, showing an accumulative effect 31. Further analysis of Colombian samples with a larger proportion of HIV positive participants could further clarify our results.
Our findings added to current evidence of psychological conditions, and concurrence of psychosocial factors on the risk of STIs acquisition in heterosexual populations in Latin America 32, in South African women 33, and in Hispanic populations in the US (34). This suggests the importance of continuing to apply the syndemic framework in populations that traditionally are not seen as priorities for HIV prevention. Studies in the heterosexual populations of Peru and Colombia, and among clients of FSW in Mexico have demonstrated the importance of prevention strategies focused on the HM and HW residing in low-income neighborhoods 12,32,35. These latter groups should also be of high priority for HIV prevention interventions in Colombia.
We did not find statistically significant additive or multiplicative interactions between the psychosocial conditions and any of the dependent variables. We found that only poly-drug use and its combination with forced sex were related to a higher likelihood of HIV positivity with the highest RERI (2.68). Yet this interaction was not statistically significant. A synergistic effect means that the effect of two conditions taken together is greater than the sum of their separate effects 6. This type of test has been reported in two studies among MSM in India 5,6, which found some synergistic effects of psychosocial factors. The possibility of a synergistic effect of violence and drug use in this study suggests that focalizing HIV and STI screening in people with such exposures could be advantageous. This could be the case of selecting individuals in whom HIV PreExposure prophylaxis- PrEP could render substantial benefit.
Strengths and limitations: This study’s sample was obtained through an HIV testing campaign, which is an effective way to identify subpopulations at risk of HIV in Colombia 19. However, it is still possible that our sample is composed of individuals with more favorable social profiles compared to samples from other studies 9. For instance, the FSW were selected from regulated sexual worksites and thus, the results obtained cannot be generalized to those working on the streets. The social vulnerability of street sex workers is likely greater than that of the group in this study. Studies conducted in Colombia indicate a higher prevalence of HIV among the FSW working on the streets 36. The higher health affiliation frequency and household income of the FSW compared to those of the HW suggest a more advantageous social profile of the FSW group in our study.
We have assessed the history of STIs by selfreport which may have introduced a memory bias. Similarly, we inquired about the previous diagnosis of STI by a doctor or nurse while in Colombia consultation to health professionals for STIs remains low 37. Therefore, the prevalence of STI might have been underestimated in this study. Additionally, the associations analyzed might have been biased, as a doctor or nurse may have not previously diagnosed those participants considered more at risk. Further studies should consider testing for STIs rather than simply relying on self-report. In this study, the questions assessing syndemics were based on behavioral surveys; questions about mental health were not included 20. Also, syndemic conditions were analyzed as dichotomous exposures, which could have limited the interpretation of findings, latent analysis, and identification of the clustering of effects. Furthermore, our analyses were based on cross-sectional data. Some associations must be interpreted cautiously as the effects of the social conditions might be inverse. For example, the education effect on early sexual initiation could be rather the case of early sexual initiation leading to low education. Longitudinal studies and intervention trials are needed to test the effects of psychosocial factors and their interactions in populations at high risks of HIV.
Finally, the lack of association may also be related to the low number of cases of HIV. Future research including larger samples of Colombian TW and MSM would contribute to verify our results.
Conclusions
Due to unfavorable social and psychosocial conditions, HIV remains increasing in Colombia.
This study demonstrates relationships between psychosocial conditions and HIV/STIs acquisition that can inform public health interventions. We hypothesize that drug use is at the core of the HIV epidemic in Colombia: First, because it correlates with the other psychosocial conditions, and; second, because it is associated with a higher HIV positivity and history of STI, a finding consistent with previous studies 8. Future studies should explore the role of psychosocial conditions on HIV-risky behaviors in larger samples of MSM, TW, and FSW while evaluating the syndemics of adverse conditions.
Current Colombian law supports the repression of drug abuse but fails to promote mental health programs dealing with violence and drug abuse from a social perspective. A life course social perspective that incorporates an understanding of early exposures on sexual health and the implementation of gender inclusion programs at all social levels could represent a way to reduce the risk of HIV infection effectively in Colombian subpopulations. The reduction of stigma, discrimination, and structural barriers at the health care level are also important measures to address the problems of violence and drug abuse in Colombia 38.














