Cervical cancer is a condition that affects women. 1 An overall estimate of the incidence of this disease for the year 2012 2 shows that, during that year, nearly 528 000 new cases were reported, of which 266 000 resulted in death. These figures demonstrate that this malignant neoplasm is the fourth most common type of cancer in women -after breast, colorectal, and lung cancers- and that it is the fourth leading cause of cancer-related deaths worldwide 1,3. In developing countries, this cancer is the second most common type of cancer and the third cause of cancer deaths, reaching higher incidence and mortality rates in less developed countries, particularly, in Sub-Saharan Africa, Melanesia, Latin America and the Caribbean 2.
From an epidemiological point of view, cervical cancer behaves as a sexually transmitted disease because it has the same risk factors. It is more frequently observed in black women, women with low level of education, those who had early sexual initiation, multiple sexual partners and those who live in urban areas of developing countries 4. The natural history of cervical cancer clearly shows its close relationship to persistent infection by human papillomavirus (HPV) with high oncogenic potential, since viral genome sequences can be found in the tumor cells of virtually all cases 5.
Despite its high prevalence, cervical cancer has the greatest potential for prevention and cure among all malignant neoplasms due its infectious nature and slow evolution, as it goes through several stages of precancerous lesions 6,7. Consequently, it can be prevented by HPV vaccination 8 and by performing a Pap smear to detect and treat precursor lesions as early as possible, prior to progression to the malignant form 9.
A study conducted in England showed that regular Pap smear screening in women from 35 to 64 years reduced the incidence of stage I cervical cancer by 67% and stage III cervical cancer by 95%, being even more effective for preventing death from this type of cancer than as a preventive measure 10.
The wide variation of the incidence and mortality rates, when considering different geographic regions in the world, reflect economic, social and cultural differences 11, as well as the availability and the quality of cytology tests. This is also evident in HPV infection incidence rates in populations of different regions of the world 12,13.
In Brazil, a historic series covering the period from 1979 through 2005 showed that mortality rates, standardized by age range, reach 5.29/100 000 women, with an increase of 6.4% over that 26-year period. The distribution of these rates exposes differences among the regions of the country according to a historic series of the period 1980-2009, with rate of 10.0/100 000 women in the North region; 5.9 in Midwest; 5.9 in the Northeast; 4.2 in the South and 3.6 in the Southeast 14. Some studies present a temporary decrease in the trend, standardized by age range in Brazil over the past few years. However, this does not occur in the same proportion across the country, as there are regional differences and, sometimes, differences within the same state when the capital is compared to the other towns 15-17.
This study aimed to determine the mortality rates from cervical cancer, analyze temporal and spatial distribution of average rates by neighborhood between 2000 and 2012, and analyze the correlation of those rates with family income in the neighborhoods of the city of Natal, capital of Rio Grande do Norte (RN), Northeast Brazil.
MATERIALS AND METHODS
An observational, retrospective and descriptive study was conducted, considering the data pertaining to mortality from cervical cancer obtained from the data base of the Sub-coordenadoria de Vigilancia Epidemiologica (Epidemiological Surveillance Subcoordinator Office) of the Secretaria de Saude do Estado do Rio Grande do Norte, Brazil (Health Department of the State of Rio Grande do Norte) for the period 2000-2012. The study sought causes and ICD C53.9 diagnosis (10th Edition - ICD-10).
The municipality of Natal is located in the Northeastern region of Brazil; it extends throughout 167 263 km2 and has 803 739 inhabitants, according to the Brazilian National Institute for Statistics and Geography (IBGE) (http://www.ibge.gov.br/cidadesat/topwindow.htm). The city of Natal has 36 neighborhoods divided into 4 administrative regions (North, South, East and West) (Prefeitura Municipal do Natal. Available in: http://www.natal.rn.gov.br/semurb/paginas/ctd-102.html).
Most neighborhoods are located in the northern and western regions, where the lowest quality of life indicators can be found, in other words, the population in these neighborhoods has lower income averages and education levels, and resides in domiciles with the lowest basic sanitation conditions. The neighborhoods in the eastern and southern regions have higher quality of life indicators 18.
Adjusted mortality rates were calculated based on the standard world population to enable comparison with international data, which is measured per 100 000 women (ASW/100 000 women); these rates were obtained considering the overall total of deaths. Furthermore, for some age ranges, the non-standardized mortality rate was the one obtained by dividing the number of deaths by the estimated mid-year population and, then, multiplying that number by 105.
The analysis of mortality rate trends was done by applying the simple linear regression model. In this model, the response variable is the mortality rate and the explanatory variable is time (measured in years). In order to determine the existence of a trend in a series, a statistical test was performed considering that the null and alternative hypotheses are a coefficient for the explanatory variable, which is either equal to or different from zero. This means that the series is considered as stable when the null hypothesis is not rejected (p-value higher than 0.05). If the null hypothesis is rejected (p-value less than 0.05), the series is classified as increasing or decreasing trend according to the positive or negative sign of the estimate obtained for the coefficient of the explanatory variable.
A residual analysis was conducted for each adjustment in order to evaluate, mainly, the stable variance hypothesis in the error distribution of the adjusted models. A Durbin-Watson test was used to confirm the correlation between the errors mentioned above, while the Shapiro-Wilk test was used to evaluate the normality of such distributions.
The average household income data for each neighborhood in the city of Natal was obtained from the Demographic Census conducted in 2010 by the IBGE. Moreover, the rough rates for each year in the 2000-2012 interval and the averages, in sequence, of those rates were calculated for the period based on the number of deaths from cervical cancer in those neighborhoods. The Empirical Bayes estimation was used to soften the aforementioned averages and, in order to evaluate spatial correlation between them, the Global Moran's index was calculated and used to verify spatial independence. The linear correlation test was used to evaluate the correlation between the softened average rates and the average household income per neighborhood. Finally, the spatial distribution and Global Moran's index analysis were conducted using the Terra View software, version 4.2.2. The R software was used for the remaining statistical analysis.
RESULTS
Between 2000 and 2012, the city of Natal reported 309 deaths from cervical cancer. The mortality rate for this type of cancer, standardized by age, was 5.5 per 100 000 inhabitants. The coefficients of mortality by age range are summarized in Table 1.
Table 1 Distribution of the number and percentage of deaths and mortality coefficients for cervical cancer in Natal, from 2000 to 2012
| Age range | No. | Reported deaths % | Non-standardized mortality coefficient /100 000 women |
| 20 - 39 years | 39 | 12.6 | 1.1 |
| 40 - 49 years | 59 | 19.1 | 8.6 |
| 50 - 59 years | 63 | 20.4 | 13.8 |
| 60 - 69 years | 65 | 21.0 | 23.1 |
| ≥ 70 years | 83 | 26.9 | 32.6 |
The distribution of the number of deaths reported over the study period, divided into three periods and from the age range point of view, showed that the number of deaths was rather similar for the periods 2000-2004 and 2009-2012, while the period 2005-2008 had fewer cases. A similar behavior was also observed in regards to mortality coefficients (Table 2).
Table 2 Deaths from cervical cancer in Natal: number of deaths per period, age range and adjusted mortality rate based on world standard population (ASW100 000 women)
| Age range | Period studied | ||
| 2000 - 2004 | 2005 - 2008 | 2009 - 2012 | |
| 20 - 39 years | 21 | 18 | 10 |
| 40 - 49 years 20 13 26 | |||
| 50 - 59 years | 29 | 13 | 21 |
| 60 - 69 years | 21 | 16 | 28 |
| ≥ 70 years | 27 | 24 | 32 |
| Total | 118 | 74 | 117 |
| ASW | 6.4 | 4.2 | 5.8 |
Analysis of trends in the historical series of the mortality coefficients, standardized and non-standardized, was conducted by age range, and is detailed in Table 3. All series were classified as stable once the p-values of the respective tests of the explanatory variable coefficients were larger than 0.05. Figure 1 details the behavior of those series over time.
Table 3 Analysis of mortality rate coefficient trends for deaths from cervical cancer according to age range, and for all standardized coefficients in Natal/RN, from 2000 to 2012
| Age range | Projected Model | p-value | Trend |
| 20 - 39 | 1.47 - 0.06t | 0.387 | Stable |
| 40 - 49 | 8.83 - 0.03t | 0.912 | Stable |
| 50 - 59 | 21.45 - 1.03t | 0.143 | Stable |
| 60 - 69 | 22.21 + 0.15t | 0.882 | Stable |
| ≥ 70 | 32.41 + 0.05t | 0.962 | Stable |
| Total | 6.51 - 0.14t | 0.243 | Stable* |
* Trends of standardized coefficient series (ASW)
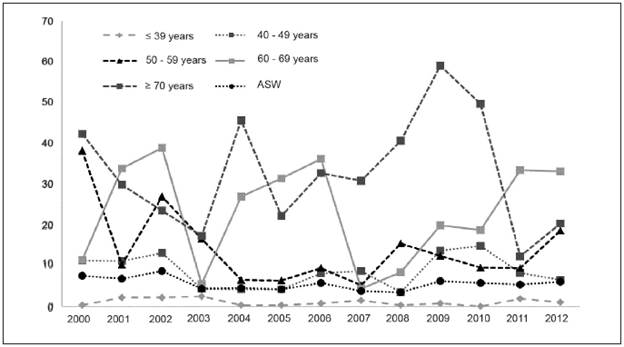
Figure 1 Mortality rates from cervical cancer in the city of Natal/RN, adjusted based on world standard population (ASW) for all women, non-standardized, by age range, from 2000 to 2012
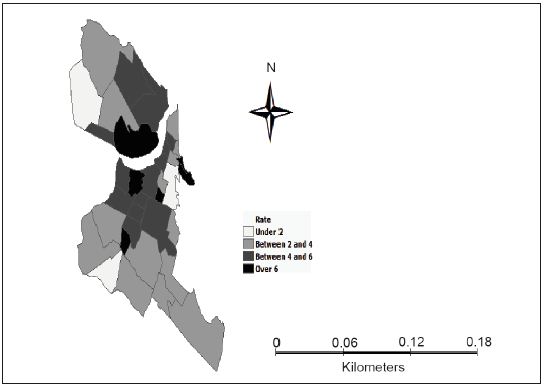
For the distribution of average death rates from cervical cancer in the neighborhoods of Natal between 2000 and 2012, the final average obtained was 4.82, with a 95% confidence interval equal to [3.74-5.90]. As a result, the Global Moran's index for those mortality rates was -0.048, with a p-value for the corresponding spatial correlation test of 0.300, which means that there is a spatial independence of the deaths from cervical cancer in Natal/ RN. Figure 2 illustrates the distribution of said rates per neighborhood. On the other hand, the average household income distribution over the neighborhoods was R$ 3,347.35, with an interval equal to [2,476.17-4,218.54] and a 95% confidence interval. The p-value obtained was p=0.648 for the linear correlation test between the mentioned incomes and average death rates from cervical cancer, which means that there is no significant linear dependency between these variables.
DISCUSSION
The death and incidence rates of cervical cancer are strongly associated with the socioeconomic status of a region, as well as with the life conditions of the studied populatiom. It is widely known that, in less developed regions, there are difficulties for using data to analyze temporal mortality trends for this type of cancer, since confirming diagnosis and providing death records is still challenging, which may result in underreporting 19.
In Brazil, the latest data available on mortality due to cervical cancer shows that there were 4 430 deaths from this type of cancer during 2013. Data also shows that five-year survival rates for patients with cervical cancer worldwide has improved throughout the years, with indexes varying from below 50% to well over 70%. In Brazil, from 2005 to 2009, five-year survival was around 61% of cases 20.
A global coverage study on cervical cancer mortality, including countries from five continents and conducted since 1973 until 1997, showed an estimated coefficient of 9.0 per 100 000 women, with rates varying from 4.0 in more developed regions to 11.2 per 100 000 women in less developed regions. Distribution across continents presented rates varying from 23.1 per 100 000 women in Africa, to 15.7 in America -2.3 in North America and 13.4 in Central and South America-, 8.4 in Asia, 5.0 in Europe and 2.0 in Oceania 21.
Another study in 29 countries of the European Union (EU), conducted from 2000 to 2004, reported that the mortality coefficients for cervical cancer, corrected by age range, varied from 1.1 per 100 000 women in Finland to 11.4 per 100 000 women in Romania 22.
Another wide coverage study conducted in 2000 and involving 20 Latin American countries, 7 in Central America and 4 in the Caribbean, found indexes varying from 4.3 per 100 000 women estimated in Puerto Rico to 53.5 estimated in Haiti. This study showed mortality coefficients for cervical cancer, corrected by age and by region, of 7.6 to 22.2 per 100 000 women in South America, 12.1 to 26.1 per 100 000 women in Central America, and 4.3 to 53.5 in the Caribbean. The same study included Brazil with a figure of 11.6 per 100 000 women, which is above the estimated coefficients of Argentina, Uruguay and Chile 23.
The relative lack of success of most Latin American countries in reducing cervical cancer incidence and mortality rates contrasts with the significant deceleration of the same rates in North America. This is clear evidence that a well-organized and well-executed preventive program not only has a protective effect but also allows for the early detection and treatment of precursor lesions and has the potential to significantly impact mortality rates 23.
According to the World Health Organization (WHO), Pap smear coverage of between 80 and 100% of the target population combined with a well-organized diagnostic network and appropriate treatment of precursor lesions can reduce cervical cancer mortality by at least 60%. Thus, high mortality coefficients from this type of cancer reflect the fragility of screening programs for early diagnosis and treatment of lesions before their progression 24.
The Brazilian screening strategy for cervical cancer is based mainly on offering the Pap smear to women aged 25 to 64, considered the most-at-risk population. Recommendations are that women with active sex life, particularly in this age group, should be tested every year or, if regular yearly testing yields two consecutive negative results, at least once every three years 20. However, the few available studies of the national screening program show a coverage averaging 70%, which is below who recommendations 25.
This study analyzed standardized and non-standardized mortality coefficients from cervical cancer for women in the city of Natal, capital of the Rio Grande do Norte (RN), Northeast Brazil, from different age groups, in the period between 2000 and 2012, their trends and spatial distribution.
The cervical cancer mortality coefficient, standardized by age, found in this study was below expectations, when compared to the world population. It could be considered better than that reported in women from less developed regions, but a little worse when compared with the women who live in the most developed regions of the world.
The non-standardized mortality coefficients for women aged 40-49, 50-59 and 60-69 were below those found for the same age groups in women from Recife (another city of northeastern Brazil) in the period 2000-2004 26. Both studies show an increase of mortality indexes as age also increases. This phenomenon can be expected since the risk of death is cumulative.
The mortality coefficient from cervical cancer, corrected by age range, found in the present study was of 5.5 deaths per 100 000 women, mildly above the estimated index for Brazil, which was 4.8 per 100 000 women 14. The latter studied a historical series for the period 19802010. It is, however, far below the mortality rate described in 27 for the Northeast region of Brazil and considers only the capital cities, which attained a coefficient of 15.3 deaths per 100 000 women in the city of Natal during the period 1996-2005. The significant difference found in these two studies could be explained by the differences in time intervals. In another study 28, a decreasing trend of the mortality coefficients for cervical cancer in the metropolitan region of Natal was found, while the present study found that trends remained stable in Natal throughout the time frame considered.
The mortality coefficient found in this study is similar to the one described for the state of Rio Grande do Norte from 2006 to 2010, which was of 5.95 per 100 000 women 28. It is also close, though slightly lower, than the coefficient found for women of Recife from 2000 to 2004: 8.2 per 100 000 women 26. Our results also show a coefficient below that reported for the state of Minas Gerais -6.8 per 100 000 women from 2004 to 2006 28. On the other hand, the coefficient obtained in the present study is higher than that found in another study conducted in Minas Gerais from 2000 to 2009, which was 2.3 per 100 000 women 15.
These results, when compared to temporal trends, differ from those described in a study that covered all Brazilian states and performed between 1980 and 2009, in which a reduction trend of the cancer mortality coefficient was detected in RN 14. It also differs when compared to the aforementioned study in relation to the results found for the Northeast Region, where a trend of increased mortality was observed 14.
The temporal stability trend for cervical cancer mortality rates standardized by age shown in the present study also differs from those found for the entirety of Brazil, or at least from the capitals of the Northeast Region in a study conducted in the period 1980-2010 16. Such study found a decrease trend of mortality rates as the years passed. The present study also differs from the trend observed for Brazil in a study conducted from 1996 to 2010, which reported a decreasing trend in cervical cancer mortality rates in the country 16, being, however, in agreement with aforementioned study regarding the Northeast Region, where a trend towards the stabilization of cervical cancer mortality rates from 2006 onwards was found 16.
These results suggest that public policies aimed at improving screening program coverage and immunization campaigns against HPV should be adjusted, so that all trends can be transformed from stable to decline.
Our results regarding the temporal trends for cervical cancer mortality rates still differ from a similar study carried out between 1980 and 2009 involving women from the Minas Gerais State, where a decreasing trend was observed in all age groups 15.
The present study did not find any correlation between spatial distribution and mortality rates from cervical cancer. Furthermore, no correlation between those rates and family income was observed. However, it is known that individuals in more vulnerable socioeconomic conditions tend to have a lower degree of knowledge about both the screening program and the main risk factor for the disease: genital HPV infection 7