Introduction
Cancer is one of the leading causes of mortality in the world due to chronic non-communicable diseases, with approximately 10 million deaths annually. Among these, gastrointestinal cancers occupy the first places in incidence and mortality rates1. In Colombia, by 2022, gastrointestinal cancers, including liver, gallbladder and pancreatic cancer, were responsible for 33.1% of cancer deaths2, highlighting their clinical, economic and social impact.
In the United States, colorectal cancer deaths have steadily declined since 1980, thanks to dietary changes, screening programs, and better access to treatment3. In contrast, this type of cancer remains a major cause of mortality in Colombia4. In 2023, according to data from the National Administrative Department of Statistics (DANE), stomach cancer was the tenth leading cause of death in the country, with 5309 deaths. Meanwhile, esophageal and colorectal cancers accounted for a total of 5540 deaths. In the department of Boyacá, stomach cancer was the fifth leading cause of death, with 156 deaths, followed by esophageal and colorectal cancers, with 152 deaths5. Esophageal cancer has a high incidence and prevalence worldwide and was responsible for 4.3% of deaths from gastrointestinal neoplasms in 20221, with dismal survival rates (15% to 25% at 5 years) due to its aggressive nature6,7. In Colombia, colon cancer is more concentrated in urban centers such as Bogotá, Quindío and Risaralda8.
These gastrointestinal neoplasms have a multifactorial origin and are associated with Helicobacter pylori infection9,10, living at altitudes above 2000 meters above sea level11,12, and behavioral factors such as obesity, smoking, and alcohol consumption13,14, all of which may influence survival15. Boyacá is a mountainous department located in central Colombia, which has been identified in previous studies as a high-risk area for the development of gastrointestinal cancer16. This situation, combined with the high consumption of tobacco and alcohol in the region17, motivated the present analysis of the survival of patients with a histopathological diagnosis at a departmental referral center.
Materials and methods
A retrospective cross-sectional study was conducted in a high complexity center in the department of Boyacá, with the objective of characterizing patients over 18 years of age with positive histopathological findings for neoplasms. Between 2018 and 2020, a total of 5935 endoscopies and 1982 colonoscopies were performed, and biopsy results positive for neoplasia were identified. The patients included in the study presented with gastrointestinal symptoms such as abdominal pain, bleeding, anemia or weight loss and, during the endoscopic procedure, macroscopic lesions of malignant appearance. Additional variables, such as TNM classification or surgical specimen analysis, were not included.
Sociodemographic information was obtained from electronic medical records (Servinte Clinical Suite), and histopathological information was collected from pathology reports. Data were stored in a database in Excel 365 and analyzed with IBM SPSS software18.
Sociodemographic variables included age, sex, origin, social security system affiliation, date of diagnosis and date of death. Other variables included the degree of differentiation, location of the lesion and presence of H. pylori (for cases of stomach cancer), and the history of exposure to cigarettes and alcohol intake. The categorization of gastric lesions followed the classification of Lauren and Jarvi19,20, grouping them into intestinal or diffuse types. Staging was not considered because it included outpatients who did not receive follow-up at the institution.
For the calculation of survival, the time in days that elapsed between the histological diagnosis and the date of death was recorded, which was obtained from the records of the Administrator of the Healthcare Social Security Resources (ADRES). The distribution of quantitative variables in gastric neoplasms was verified using the Kolmogorov-Smirnov test due to the large sample size, while for esophageal and colorectal neoplasms, the Shapiro-Wilk test was used. The medians and their confidence intervals were estimated using the Mann-Whitney U test. For nominal variables, frequency and position measures were calculated, applying the chi-square test or the Fisher’s test to assess statistical significance, with a 95% confidence interval (CI).
Survival analysis was performed using the Kaplan-Meier method and curves were compared using the Log-Rank statistical test. The study followed the principles of the Declaration of Helsinki, was approved by the ethics committee of the Hospital Universitario San Rafael de Tunja (Act 0011-2021) and was considered a risk-free investigation, complying with the standards of good clinical practice21.
Results
During the study period, 133 malignant neoplasms of the gastrointestinal tract were reported. Of these, 18 patients received surgical management during the same hospitalization. In cases of esophageal cancer, no patient underwent surgical resection with curative intent. A total of 64.2% (n = 9) received palliative care through stent insertion, while the remaining patients were either undergoing additional studies or had such an advanced disease that no palliative care could be provided.
The median age was 66.7 years (interquartile range [IQR]: 59-79), with a range between 24 and 92 years. All age groups were represented; however, the highest incidence was observed in the 60-69 age group (25.5%), followed by the 70-79 age group (24.8%). According to sex, a male predominance was observed, with 73 cases (55.3%) (Table 1). It is noteworthy that between the ages of 20 and 39 years there were more cases of malignant neoplasms in women. The youngest patient and the oldest patient had gastric adenocarcinomas.
Table 1 Sociodemographic Characteristics of the Population Under Study
| Variable | n | % | |
|---|---|---|---|
| Sex | Female | 60 | 45% |
| Male | 73 | 55% | |
| Health Insurance System Regime | Subsidized | 104 | 78% |
| Contributory | 21 | 16% | |
| Special | 8 | 6% | |
| Origin | Tunja | 55 | 42% |
| Other cities in Boyacá | 74 | 55% | |
| Other departments | 4 | 3% | |
Table created by the authors.
In the distribution of neoplasms of the gastrointestinal tract, the highest proportion corresponds to gastric cancer, with 66.2% (n = 88), followed by colorectal carcinoma, with 23.4% (n = 31), and esophageal cancer, with 10% (n = 14) (Figure 1).
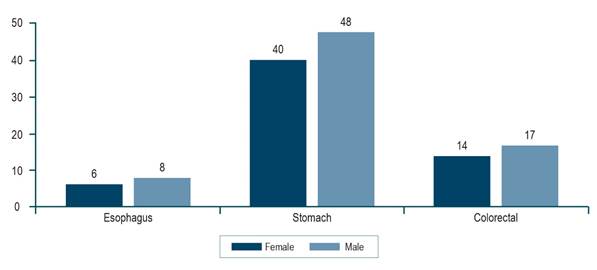
Figure 1 Anatomical Distribution of Gastrointestinal Neoplasms According to Sex. The image is the property of the authors.
The most frequent histologic type was adenocarcinoma (n = 114, 85%), with a predominance of the intestinal subtype, which manifested more frequently in patients older than 60 years (Table 2).
Table 2 Distribution of Gastrointestinal Neoplasms According to Age, Sex, Type and Anatomical Localization
| Variable n (%) | ≤29 years n (%) | 30 to 59 years n (%) | ≥60 years | p* n (%) | Total | |
|---|---|---|---|---|---|---|
| Sex | Female | 3 (75) | 11 (37) | 46 (46) | 0.30 | 60 (45) |
| Male | 1 (25) | 19 (63) | 53 (54) | 73 (55) | ||
| Neoplasm | Adenocarcinoma | 4 (100) | 27 (90) | 84 (83) | 0.93 | 115 (85) |
| Carcinoma | 0 (0) | 0 (0) | 9 (9) | 9 (7) | ||
| Lymphoma | 0 (0) | 2 (6) | 4 (5) | 6 (5) | ||
| Mesenchymal | 0 (0) | 1 (4) | 3 (3) | 4 (3) | ||
| Localization | Esophagus | 0 (0) | 3 (10) | 11 (11) | 0.63 | 14 (10) |
| Stomach | 4 (100) | 21 (70) | 63 (63) | 88 (66) | ||
| Colorectal | 0 (0) | 6 (20) | 25 (26) | 31 (24) | ||
Table created by the authors.
Upon classification, according to the histological type of neoplasm found, it was determined that adenocarcinoma of the intestinal type was the most frequent, followed by the diffuse type (Table 3).
Table 3 Histological Classification of Neoplasms According to the World Health Organization22
| Type of neoplasm | Frequency | Percentage |
|---|---|---|
| Adenocarcinoma | 2 | 1.5% |
| Tubular-pattern adenocarcinoma | 7 | 5.3% |
| Diffuse-type adenocarcinoma | 14 | 10.5% |
| Intestinal-type adenocarcinoma | 84 | 63.2% |
| Mucinous adenocarcinoma | 1 | 0.8% |
| Adenocarcinoma in situ | 3 | 2.3% |
| Metastatic adenocarcinoma | 1 | 0.8% |
| Mixed adenocarcinoma (intestinal pattern) | 2 | 1.5% |
| Mixed adenocarcinoma (tubular and diffuse pattern) | 1 | 0.8% |
| Squamous cell carcinoma | 7 | 5.3% |
| Neuroendocrine carcinoma | 1 | 0.8% |
| Carcinoma or lymphoma | 1 | 0.8% |
| Lymphoma | 1 | 0.8% |
| Diffuse large B-cell lymphoma | 1 | 0.8% |
| B-cell lymphoma | 3 | 2.3% |
| Mantle B-cell lymphoma | 1 | 0.8% |
| MALT-type B-cell lymphoma | 2 | 1.5% |
| Mesenchymal neoplasm (GIST or mucinous origin) | 1 | 0.8% |
| Total | 133 | 100 |
GIST: gastrointestinal stromal tumor; MALT: mucosa-associated lymphoid tissue. Adapted from: Bosman F, et al. 4th edition. World Health Organization; 2010.
A review of the history according to the location of the neoplasm showed that 12.9% of the patients with colorectal cancer smoked, while 54.2% of the gastric neoplasms had the presence of H. pylori (Table 4).
Table 4 Distribution of Neoplasms by Location in Relation to the Presence of H. pylori, Alcohol and Tobacco Consumption
| Location n (%) | Esophagus n (%) | Stomach n (%) | Colorectal | |
|---|---|---|---|---|
| H. pylori | Absent | 13 (92.9) | 38 (45.8) | 0 |
| Present | 1 (7.1) | 45 (54.2) | 0 | |
| Tobacco use | Yes | 3 (21.5) | 10 (12) | 4 (12.9) |
| No | 11 (78.5) | 73 (88) | 27 (87.1) | |
| Alcohol consumption | Yes | 1 (7.1) | 17 (20) | 6 (19.3) |
| No | 13 (92.9) | 66 (80) | 25 (80.6) | |
Table created by the authors.
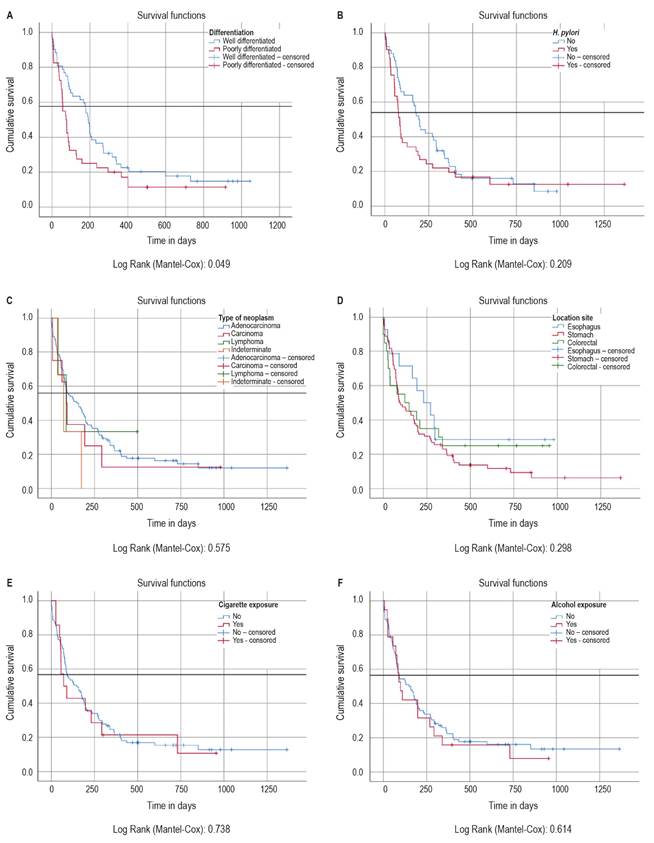
On consulting the ADRES data, it was found that, as of April 25, 2023, 87.9% (n = 117) of the patients had died. A survival analysis was conducted on these 117 subjects, who were followed for 4.8 years. Survival was evaluated according to the degree of histopathological differentiation, which showed a statistically significant difference (p = 0.049). Median survival was 22 months from diagnosis to death (95% CI: 16.2-27.8), with a median of 109 days (95% CI: 34.7-183.2) and a maximum survival time of 3.7 years (Figure 2).
A total of 87 samples from the esophagogastric junction and stomach were analyzed. In 17.2% of the cases, the presence of H. pylori could not be determined due to the lack of a report and the transfer of the slide to the family; in contrast, 32.1% of the samples tested positive for this microorganism. A survival curve was generated, in which the presence of H. pylori did not show statistical significance on survival (p = 0.45) (Figure 2B).
Based on the findings presented in the survival curve according to the degree of differentiation, and given the clinical significance, survival by type of neoplasm and site of appearance was also verified (Figures 2C and D). These were not significant, since they obtained a p-value of 0.57 and 0.298, respectively. When evaluating the median survival according to the variables studied (Table 5), it was observed that people who use tobacco and present poorly differentiated neoplasms have a lower survival, while people under 60 years of age show a higher survival.
Table 5 Median survival by type of variable
| Variable | Estimate (days) | 95% confidence interval | ||
|---|---|---|---|---|
| Lower limit | Upper limit | |||
| Age | Under 60 years | 236 | 107.3 | 364.6 |
| Over 60 years | 92 | 32.4 | 151.5 | |
| Sex | Female | 130 | 52.8 | 207.1 |
| Male | 92 | 0.0 | 195.2 | |
| Differentiation | Well differentiated | 191 | 170.8 | 211.1 |
| Poorly differentiated | 74 | 46.7 | 101.2 | |
| Neoplasm | Adenocarcinoma | 148 | 76.2 | 219.7 |
| Carcinoma | 88 | 47.8 | 128.2 | |
| Lymphoma | 86 | 10.7 | 161.2 | |
| Poorly differentiated | 71 | 16.5 | 125.4 | |
| Localization | Esophagus | 231 | 87.9 | 374 |
| Stomach | 92 | 32.3 | 151.7 | |
| Colorectal | 123 | 0.0 | 274.2 | |
| H. pylori | Absent | 193 | 157.3 | 228.6 |
| Present | 84 | 66.4 | 101.5 | |
| Alcohol consumption | Absent | 148 | 69.9 | 226 |
| Present | 99 | 63.4 | 134.5 | |
| Tobacco use | Absent | 148 | 76.0 | 219.9 |
| Present | 71 | 10.4 | 131.5 | |
| Global | 127 | 57.9 | 196 | |
Table created by the authors.
Discussion
The present study is relevant because it provides unpublished information on the incidence and survival after histopathological diagnosis of digestive tract cancers in samples obtained endoscopically in a referral center in the department of Boyacá. In Colombia, a continuous increase in the incidence and prevalence of gastrointestinal tract neoplasms is projected, with the exception of gastric cancer16. The median age at diagnosis is slightly higher than that reported in Latin America23-26. In addition, colorectal, gastric and esophageal cancers are more frequent in men27, which is consistent with data from regional and international studies2,28-30.
When comparing the survival presented in other parts of the world and that reported in Colombia26,31,32, a lower survival was found in our population, which could be attributed to sociodemographic factors or late diagnosis. Although the type of affiliation to the social security system does not seem to be a determining factor, it is possible that this low survival rate is influenced by the fact that more than 50% of the population studied belongs to the subsidized regime and resides in the area of influence of the institution, in the department of Boyacá33.
Given the high prevalence of H. pylori infection reported in Colombia (63.4%)34, its relationship with survival was analyzed, despite the fact that more than 10% of the data on gastric cancer were not available. Thus, it was observed that, together with the degree of differentiation, the presence of H. pylori is associated with a decrease in survival.
The main strength of the study is that it was conducted in a referral center that serves people from several surrounding areas, which allowed histological confirmation of the diagnoses. However, the size of the sample, the absence of tumor staging, the assessment by oncology in the absence of this institutional service and the lack of analysis of additional comorbidities, especially due to the limitations imposed by the Covid-19 pandemic, represent important limitations35,36.
In conclusion, it highlights the importance of implementing screening to detect these neoplasms in early stages in high-risk patients, given that the cancers diagnosed in this study were in advanced stages, resulting in short survival. It is essential to increase awareness of risk factors and promote healthy lifestyles (no alcohol or smoking). Further studies involving multiple institutions and interdepartmental collaborations are also required to identify factors associated with the observed poor survival, including the role of H. pylori in this population.
Conclusion
The population treated with endoscopies at a departmental referral center for digestive tract neoplasms is primarily composed of men, who were diagnosed at advanced stages, which was reflected in limited survival. This situation could be positively impacted by the implementation of screening programs, community education on risk factors, and improvements in the quality of endoscopy at primary care levels.











 text in
text in