Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO -
 Access statistics
Access statistics
Related links
-
 Cited by Google
Cited by Google -
 Similars in
SciELO
Similars in
SciELO -
 Similars in Google
Similars in Google
Share
Revista colombiana de Gastroenterología
Print version ISSN 0120-9957
Rev Col Gastroenterol vol.30 no.1 Bogotá Jan./Mar. 2015
Experience with Liver Transplantation in patients over 65 years of Age at the Hospital Pablo Tobón Uribe in Medellin, Colombia from 2004 to 2010
Octavio Muñoz MD. (1), Laura Ovadía MD. (2), Yesid Saavedra MD. (2), Juan Carlos Restrepo MD. MSc. PhD. (1), Carlos Yepes MD. MSc. PhD. (3), Óscar Santos MD. (1), Juan Ignacio Marín MD. (1), Sergio Hoyos MD. MSc. (1), Carlos Guzmán MD. (3), Álvaro Mena MD. (3), Gonzalo Correa MD. (1)
(1) Gastro Group of the Faculty of Medicine at the Universidad de Antioquia and Hospital Pablo Tobón Uribe in Medellin, Colombia.
(2) Gastrohepatology Group of the Faculty of Medicine at the Universidad de Antioquia in Medellin, Colombia.
(3) Faculty of Medicine at the Universidad de Antioquia and Hospital Pablo Tobón Uribe in Medellin, Colombia.
Received: 29-05-14 Accepted: 02-02-15
Abstract
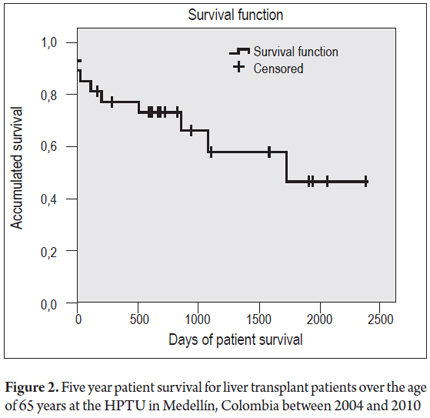
Liver transplantation protocols have been extended to people over 65 years of age who had previously been excluded from protocols due to the increased morbidity and mortality rates associated with age. This study aims to identify survival rates and complications in patients over 65 years who have undergone liver transplantation. Medical records of patients older than 65 who underwent liver transplantation in the period between September 2004 and November 2010 at the Hospital Pablo Tobón Uribe in Medellin, Colombia were analyzed. We studied 27 patients with an average age of 67 years. The 30 day post-transplant survival rate was 85.2%, at one year the survival rate was 70.4%, and at five years it was 63%. An evaluation of post-transplant complications found that the most frequent complications were massive bleeding and nosocomial infections. The main causes of death were cardiovascular events. Conclusion: Proper patient selection allows those over 65 years of age to become candidates for liver transplantation with a good actuarial 5-year survival rate and better quality of life.
Keywords
Hepatic transplantation, liver transplantation, liver grafting, old age, 65 years and over.
INTRODUCTION
Orthotropic liver transplantation (OLT) is the accepted as treatment of choice for patients with advanced liver disease with have poor prognoses whose disease manifests as chronic liver disease with uncontrollable complications such as acute liver failure and selected tumors. With the development of new surgical techniques, anesthesia, intensive care immunosuppression regimens, survival rates have improved to 83% at one year following transplantation and to 75% after five years. The success of this therapy is responsible for the high demand for the procedure: over six thousand transplants are performed every year in the European Registry and a similar number are performed in the American registry (1, 2).
Until the beginning of the 1980's, only a few centers anywhere in the world transplanted patients who were over 50 years old. Now, the evolution of technique and technology has made it possible to include more people on the waiting list who were previously ineligible because of age or comorbidities. This can be explained by two reasons. First, there has been a progressive increase in the percentage of the population that is over 65 years. In the United States the average life expectancy has increased by 17 additional years. It is estimated that by 2030 the proportion of the population over 75 years old will increase from 6% to 9%, and it will reach 12% by 2050. Second, the prevalence of liver disease, especially chronic hepatitis C and hepatocellular carcinoma, that requires OLT has increased among these groups (3, 4).
Reports from individual medical centers have shown good results among older patients including complication and survival rates similar to those of younger organ recipients. Nevertheless, the results reported in the registries do not confirm this (5, 6). In addition, other medical centers have shown prolonged hospital stays and increased mortality. With these results, age restrictions on OLT vary from center to center, and some consider that more importance should be given to chronological age and physiological age in addition to the strict focus on the diagnosis of comorbidities, especially cardiovascular, pulmonary and neoplastic ones (7, 8).
This study reports results for OLT patients over 65 years of age at the Hospital Pablo Tobón Uribe (HPTU) in order to evaluate survival and complication rates in this population group which can lead to better plans for strategies to improve outcomes.
MATERIALS AND METHODS
Information about patients who were recipients of cadaveric liver transplants at the HPTU from September 2004 to November 2010 was obtained retrospectively from the database of the Gastrohepatology Group of the University of Antioquia. From among these patients, men and women who were older than 65 were selected and evaluated according to the protocol established by the hospital. The protocol includes pretransplant studies to assess cardiovascular risks and screening for malignancies. Tests include EKGs, resting echocardiography, dobutamine stress echocardiography, and colonoscopies. Mammography and Pap smears are performed for women, and the prostate-specific antigen test is done for men. In addition, pulmonary function tests are performed if patients have hypoxemia or histories of lung disease. Patients' right heart chambers are catheterized if there is evidence from echocardiography or coronary angiography of pulmonary hypertension or if a pharmacological stress test is positive for myocardial ischemia. Patients are excluded if they have severe cardiopulmonary disease, pulmonary hypertension, systemic infections, advanced AIDS, extrahepatic neoplasia, drug or alcohol addiction, uncontrolled psychiatric disease, and thrombosis of the hepatic portal system- Patients with acute liver failure that had developed irreversible brain damage were also excluded.
The immunosuppression protocol used by the Gastrohepatology Group for liver transplant patients includes intraoperative administration of 1 g of intravenous methylprednisolone followed by decreasing doses until the sixth day when daily administration of 20 mg of prednisolone begins for a three month period. In the immediate postoperative period, patients are classified into two groups: those with renal impairment or with high risks of developing it, and those without current or potential kidney problems. The former group receives 1000 mg Mycophenolate every 12 hours while the second group is given 1-2 mg/kg of Azathioprine. In patients with renal impairment or at high risk of developing it, calcineurin inhibitor is administered from the third day after the procedure or when renal functioning permits. In patients without kidney problems, administration of calcineurin begins six to eighteen hours after transplantation and continues at gradually increasing doses. The first-line drug is Cyclosporine until it reaches the objective of the C2 level in the first quarter which is between 800 and 1200 ng/mL. For patients who have adverse effects and acute cellular rejection, a change is made to Tacrolimus. All patients are strictly monitored through periodic outpatient check-ups to assess graft functioning, adverse effects of immunosuppression, transplant complications, metabolic complications, neoplastic complications, etc.
The statistical analysis was based on descriptions of various sociodemographic and clinical variables of the patients under study. Variables included pretransplant conditions, comorbidities, etiology of liver disease severity classified by Child-Pugh and MELD, laboratory test results, intraoperative and postoperative variables such as complications, days in the ICU, hospital stays, graft survival and overall survival. Initially, the type of distribution of variables was verified and bivariate analysis was performed using the Chi2 test for categorical variables and the nonparametric Mann-Whitney test to compare ranges between independent groups. For all cases, the Kaplan Meier curve was used to analyze graft survival, graft loss and patient death at 30 days, one year and 5 years. Multivariate logistic regression was used to try to explain possible associations between the most relevant variables with dichotomous outcomes of graft loss and death.
RESULTS
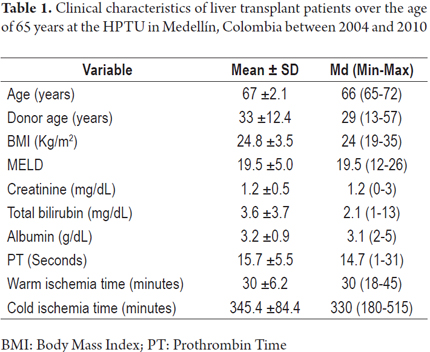
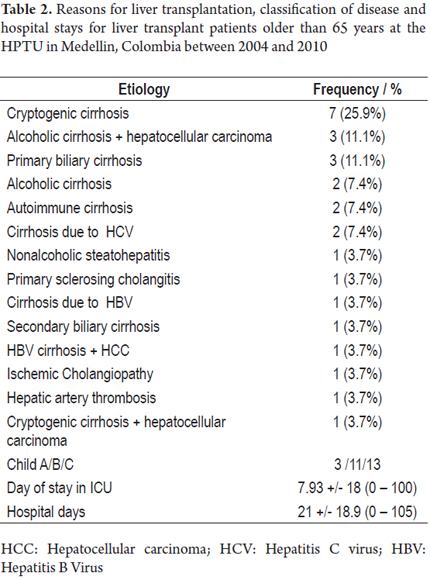
From 2004 to 2010 at the HPTU, 305 orthotropic liver transplants were performed with cadaveric donor in adults and children. Twenty-seven of these patients were over 65 years of age. Of these 59.3% were female, and the average age was 67 years (65-72 years). Thirteen patients were Child C, and the mean MELD score was 19 points (12-26 points). Eight patients (29%) had a diagnosis of cryptogenic cirrhosis, five patients (18%) had alcohol-related cirrhosis, and 6 patients (22%) had hepatocellular carcinoma. Demographic characteristics and etiologies of liver dysfunction are shown in Tables 1 and 2.
The following rates of complications of liver disease were found: 66% of the patients had ascites, 52% had encephalopathy, 33% had histories of bleeding varices, 22% had spontaneous bacterial peritonitis, and 22% had pre-transplant renal dysfunction. 18.5% of the patients were hospitalized prior to procedures. Comorbidities were found in 66.7% of the patients. They included diabetes mellitus, hypertension, coronary heart disease, chronic renal failure and/or chronic obstructive pulmonary disease. The most frequently used immunosuppression scheme, cyclosporine, azathioprine and prednisolone, was used in 33% of the transplants. A combination of cyclosporine, mycophenolate and prednisolone was used for 22% of the transplants. Two of the patients underwent retransplantation. One of them had suffered acute thrombosis of the hepatic artery, and the other had ischemic cholangiopathy.
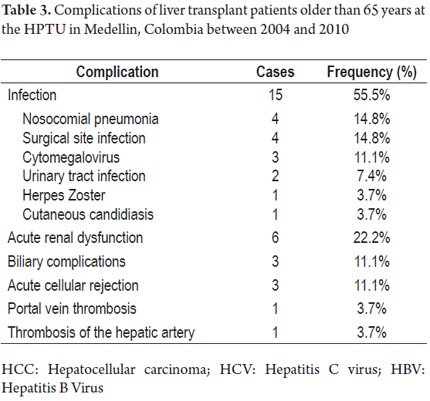
Immediate postoperative complications included massive bleeding in 8 patients (29%). Two of these required packing and five (18%) were reoperated. We also evaluate complications during the first 3 months after transplantation and found fifteen cases of infectious complications. These occurred more frequently than nosocomial pneumonia and urinary tract infections. Six patients (14%) suffered acute renal failure, and four patients required renal replacement. Three patients had biliary complications. There were three cases of acute cellular rejection demonstrated by biopsy, one case of thrombosis of the hepatic artery, and one case of portal thrombosis (Table 3).
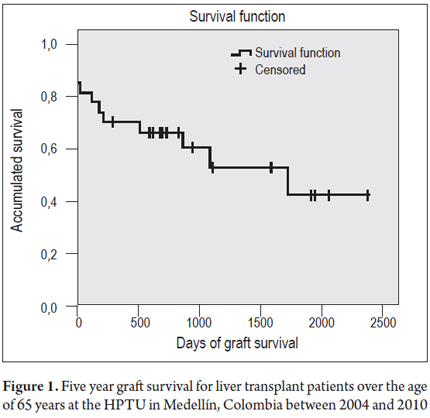
The median survival time for both the graft and patient survival at 5 years was 1,727 days (95% CI 494 to 2,959.9). Figure 1 shows graft survival at 30 days of 81.5%, graft survival at one year of 63%, and graft survival at 5 years of 55.6%. Figure 2 shows patient survival rates for the same periods of time: 85.2% at 30 days, 70.4% at one year, and 63% at 5 years. Ten patients died during the follow-up period. Cardiopulmonary disease, which accounted for three of the deaths, was the single most important cause. There were two deaths due to septic shock, two cases of massive intraoperative bleeding, one case of primary graft dysfunction, and one patient died of neoplasia of gastric origin. The multivariate analysis showed no associations of these variables with the outcomes of graft loss or death.
DISCUSSION
Because liver transplantation in patients over 65 is still under discussion at transplant centers around the world, the results of this series should provide valuable information for making the decision about transplantation for patients in this age group. Proper patient selection permits good actuarial survival in the medium and long term that is comparable to those reported for other age groups.
At present, patients over 60 constitute 20% of the patients transplanted in the European registry. Before older patients undergo liver transplantation risks and benefits should be assessed. Patients should be undergo careful analyses to exclude cardiopulmonary disease, malignancies and other conditions of the elderly.
The survival rates described in this paper are similar to those reported in other studies with patients of the same age. Cross and colleagues at the Institute for the Study of Liver of King`s College Hospital found that survival rates in a sample of 77 patients who were over 65 years when they received transplants between 1988 and 2003 were 99% at 30 days, 82% at one year, and 73% at five years. A study conducted at Baylor University in 2001 found a survival rate at three years of 62%, and a survival rate at five years of 60% (10, 11).
Another study that analyzed the survival of patients over 60 years of age was done by Filliponi in 2001. It had a sample of 23 patients were underwent transplantation between 1996 and 2000. The number of participants was a little less than in our study. That study found a one year survival rate of 87.5%, and a three year survival rate of 83.3%. Although our study did not analyze survival at three years, the results found by this author for the one year survival rate are similar to those obtained at our center (12).
The difference between patient survival and graft survival rate reported is due to the two cases that required retransplantation. Although this situation is unusual among patients over 65 years of age, there were complications of vascular origin that could not be foreseen during the pretransplant evaluations or in the postoperative period.
Transplant complications such as infections, vascular and bile duct complications occurred in the same proportions as traditionally reported, despite the short-term analysis.
Long-term survival within this group of patients may be affected by increased incidence of complications such as tumors and heart disease, the latter being the main cause of death in our study. It has also been suggested that senescence of the immune system in the elderly, may reduce the need for immunosuppressive drugs and result in a lower rate of graft rejection (9). This is reflected in our rejection rate of only 11% which is much lower than those reported in series from the general population of patients who have undergone liver transplantation.
Although not assessed with appropriate instruments, patients who survived managed to join their families and engage in social activities which substantially improved their quality of personal and family lives.
Numerous factors have been associated with adverse outcomes. A review of studies of liver transplantation in patients over 60 years of age shows that the variables with the greatest negative impacts on survival are serum bilirubin> 10 mg/dl, albumin <3 mg/dl, prothrombin time > 20 seconds, a MELD score higher than 25, Child C, inadequate pretransplant nutritional status, complications of chronic liver disease and encephalopathy, ascites, and hospitalization prior to transplantation (5, 11).
Multivariate analysis in this study failed to show a clear influence of any of the variables mentioned on patients or graft survival. This result can be explained by the small number of patients analyzed which may have been too small to find statistically significant associations.
The major limitation of this study was the small number of patients included. Although performance of liver transplantations is increasing in Colombia, they are performed less frequently in our country than in other centers around the world. It should also be noted that the proportion of transplant patients over 65 years of age remains very low in our environment.
Finally, considering that our survival figures are similar to those published internationally, this study serves provides support for liver transplantation over 65 years of age when they have been appropriately selected and when practices that allow good results for our patients to increase survival and quality of care are implemented. This report is the first such study in our country, and it opens the door for other centers where liver transplantation is performed to publish their results so that we can obtain sufficient information and generate national statistics.
Conflicts of interest
The authors declare that they have no conflicts of interest.
REFERENCES
1. European Liver Transplant Registry. Data analysis booklet. Paris 2007. Available at: http://www.eltr.org. [ Links ]
2. O'Leary JG, Lepe R, Davis GL. Indications for liver transplantation. Gastroenterology 2008;134:6. [ Links ]
3. Aduen JF, Sujay B, Dickson RC, et al. Outcomes after liver transplant in patients aged 70 years or older compared with those younger than 60 years. Mayo Clin Proc 2009;84:11. [ Links ]
4. Arias E. United States life tables, 2002. Natl Vital Stat Rep 2004;53:1-38. [ Links ]
5. Zetterman RK, Belle SH, Hoofnagle JH, et al. Age and liver transplantation: a report of the Liver Transplantation Database. Transplantation 1998;27:66(4). [ Links ]
6. Rudich S, Busuttil R. Similar outcomes, morbidity, and mortality for orthotopic liver transplantation between the very elderly and the young. Transplant Proc 1999;31(1-2). [ Links ]
7. Adam R, Hoti E. Liver transplantation: the current situation. Semin Liver Dis 2009;29:1. [ Links ]
8. Ahmed A, Keeffe EB. Current indications and contraindications for liver transplantation. Clin Liver Dis 2007;11:2. [ Links ]
9. Keswani RN, Ahmed A, Keeffe EB. Older age and liver transplantation: a review. Liver Transplantation 2004;8:10. [ Links ]
10. Cross TJ, Antoniades CG, Muiesan P, et al. Liver transplantation in patients over 60 and 65 years: an evaluation of long-term outcomes and survival. Liver Transpl 2007;13:10. [ Links ]
11. Levy MF, Somasundar PS, Jennings LW, et al. The elderly liver transplant recipient: a call for caution. Ann Surg 2001;233:1. [ Links ]
12. Filipponi F, Roncella M, Boggi U, et al. Liver transplantation in recipients over 60. Transplant Proc 2001;33:1-2. [ Links ]











 text in
text in