Introduction
Empyema necessitatis or empyema necessitans is a complication of pleural empyemas in which the infection extends out of the pleural cavity, involving the soft tissues of the thoracic wall or other body segments. 1,2 It is mainly caused by Mycobacterium tuberculosis infection, followed by Actinomyces spp.3 This paper reports the case of a patient with empyema necessitatis secondary to Citrobacter freundii infection, which is the first of its kind reported so far in the literature, as seen after a search in PubMed, BIREME and SciELO databases is made.
Case presentation
A 26-year-old Caucasian patient, from a rural area, with a history of severe cognitive deficit secondary to cerebral palsy, was taken by his father to the emergency department due to a clinical picture of 15 days of evolution consisting of neurological deterioration evidenced by decreased contact with his environment, and greater difficulty to perform the basic activities of daily living (eating and dressing). These symptoms appeared along with asthenia, adynamia, fever and cough with greenish phlegm.
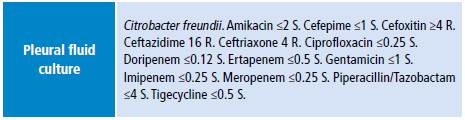
Physical examination showed a patient with blood pressure of 100/68mmHg, heart rate of 76 beats per minute, respiratory rate of 17 breaths per minute and oxygen saturation of 94% to the environment. He also had multiple caries and gingivitis, drowsiness, hypoprosexia and diminished lung sounds in the right base. Hypochromic microcytic anemia, leukocytosis with neutrophilia, elevated C-reactive protein and normal renal and hepatic function were found in the paraclinical tests taken to the patient on admission (Table 1).
Table 1 Paraclinical tests on admission.
PMN: polymorphonuclear leukocyte; MCV: mean corpuscular volume; MCH: mean corpuscular hemoglobin; AST: aspartate aminotransferase; ALT: alanine aminotransferase; BUN: blood urea nitrogen.
Source: Own elaboration.
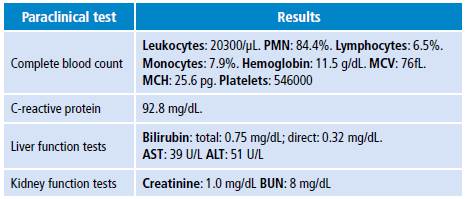
Sputum smears were taken, which were negative for acid-fast bacilli. The chest x-ray showed consolidation in the middle lobe associated with pleural effusion, leading to a diagnosis of community-acquired pneumonia. Empiric management with ampicillin/sulbactam and clarithromycin was initiated. Despite having received a 5-day course of antibiotics and the improvement of respiratory and neurological symptoms, febrile peaks persisted, so new laboratory tests were taken, revealing persistence of leukocytosis and neutrophilia, and elevated C-reactive protein (Table 2). Ultrasonography of the right pleural cavity showed free-flowing pleural effusion (339.4cm3).
Table 2 Control paraclinical tests on day 6.
PMN: polymorphonuclear neutrophils; MCV: mean corpuscular volume; MCH: mean corpuscular hemoglobin.
Source: Own elaboration.
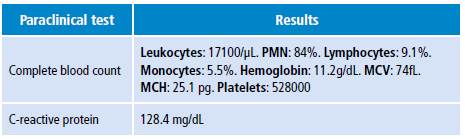
A diagnostic thoracentesis was performed, which allowed obtaining clear fluid with characteristics of simple parapneumonic effusion (Table 3). Culture of this sample was taken for common germs, which was negative.
Table 3 Cytochemical and cytological study of pleural fluid and paired blood samples.
Source: Own elaboration.
Given the persistence of systemic inflammatory response signs, the antibiotic treatment was changed to piperacillin/tazobactam and acquired immunodeficiency was ruled out as a causal factor of poor response to treatment by negative HIV ELISA test. During the following 4 days of therapy, the patient developed a mass on the anterior right thorax, of about 4 cm in diameter, without local inflammatory changes.
Computed tomography of the thorax was performed, revealing consolidation of the middle lobe and ipsilateral pleural effusion, along with hypodense mass projected on the pectoral muscular plane (Figure 1) and extension from the fourth to the seventh intercostal space, leading to diagnose empyema neccesitatis.
Source: Document obtained during the study
Figure 1 Computed tomography of the thorax. Axial section.
Figure 1 shows consolidation of the middle lobe and ipsilateral pleural effusion, along with hypodense mass projected on the pectoral muscular section. The arrow indicates the point where pleural collection passes through the muscular section of the chest wall into the subcutaneous cellular tissue of the right pectoral region.
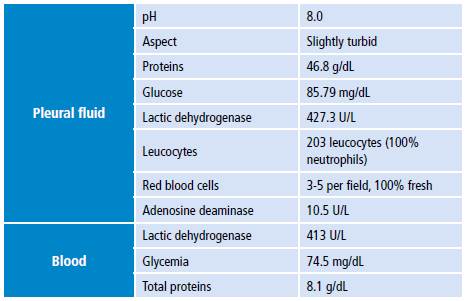
Percutaneous drainage was established for treating and diagnosing the collection. ADA (adenosine deaminase) and culture were performed for mycobacteria, which were negative, as well as a culture for common germs with C. freundii isolate with hyperproduction of class C chromosomal beta-lactamase and sensitive to aminoglycosides and fluoroquinolones (Table 4). Cefepime was administered for four weeks and the scheme was completed with oral ciprofloxacin for four weeks more. Respiratory and neurological symptoms completely resolved, and the thoracic mass disappeared.
Discussion
First described in 1640 by Guillan de Baillon 2,4, empyema necessitans or empyema necessitatis is a pleural empyema complication, in which infection extends towards the pleural cavity and involves the soft tissues of the chest wall 1 or other body segments. This occurs more frequently through the less resistant area, which is usually located between the second and sixth intercostal space and between the midclavicular line and the anterior axillary line. In less frequent cases, the abdominal wall, paravertebral space, vertebrae, esophagus, bronchi, mediastinum, diaphragm, pericardium, flank, breast and retroperitoneum may be involved. 1,2,4 Another manifestation may include the formation of pleurocutaneous or bronchopleurocutaneous fistulas. 3
Empyema necessitans is more common in adults. Chronic alcoholism, cachexia, chronic obstructive pulmonary disease, tuberculosis, poor oral hygiene and bronchiectasis have been found to be risk factors. 5
In this case, the extension of pleural empyema occurred through the fourth to seventh intercostal space with involvement of the soft tissues of the thoracic wall; the risk factor of this adult patient was having poor oral hygiene.
To establish a diagnosis, it is necessary to confirm the continuity of the pleural collection with the thoracic wall or the affected body segment. 5
The most frequent etiological agents and mortality rates have changed with the advent of antibiotics. In 1940, Sindel 6 published a review of cases in which he found that the most frequent cause was M. tuberculosis (73% of cases), followed by Streptococcus pneumoniae, and a total mortality rate of 66%, of which 87% were related to tuberculosis.
After the development of antibiotics, Freeman et al.4 conducted a case review from 1966 to 2004 and found that 50% of these infections were secondary to tuberculosis and 24% to actinomycosis. Then, Llamas et al.5, in a review of cases published between 2004 and 2010, found that M. tuberculosis and actinomycosis (mainly Actinomyces israelii and Actinomyces odontolyticus) remained the main causes (35% and 20%, respectively). In both studies, the reported mortality was 0%. Following these publications, case reports were reviewed, finding only one case of mortality related to infectious empyema. 7
In addition to the microorganisms described, cases have been reported involving Klebsiella corrodens, Streptococcus milleri, Burkholderia cepacia, Fusobacterium nucleatum, Mycobacterium avium intracellulare, Aspergillus fumigatus, Zygomycetes, Blastomyces spp, Peptostreptococcus, Bacteroides, Propionibacterium, Coccidiodes immitis, Streptococcus agalactiae, Nocardia asteroides and Corynebacterium jeikeium.2,3,8-10
Differential diagnoses should consider traumatic causes (pulmonary herniation), neoplasms (mesothelioma, lymphoma, malignant fibrous histiocytoma, among others) and inflammatory processes in the chest wall. 3 In the case described here, the patient did not report a traumatic history, so pulmonary herniation was not considered as a possibility. On the other hand, the clinical picture and the paraclinical symptoms suggested an infectious pulmonary process, which, added to the neutrophilic exudate within pleural fluid, which is more frequently associated with parapneumonic effusion 11-13, led to consider a neoplasm as unlikely. Furthermore, the most common finding in a neoplastic exudate is the presence of lymphocytes >50%. 13
Treatment consists of broad-spectrum antibiotic therapy until a culture-directed therapy can be administered and, in most cases, the collection is drained. 2
Regarding surgical approach to drainage, Akgül et al.7 conducted a study in seven patients with empyema necessitatis of various etiologies. These authors concluded that surgical techniques may include chest tube, decortication or open drainage of the collection, and that they should be chosen taking into account the physical condition, age, the duration of symptoms, the etiology and the existence of a parenchymal pathology in each patient. 7 In this case, the management of the collection was limited to percutaneous drainage because the patient's caregivers refused more invasive surgical procedures.
This case is important given that, after conducting a search, it is the first report of this pathology by C. freundii, which broadens the spectrum of clinical pictures that can occur due to this microorganism. This bacterium is part of the genus Citrobacter (member of the Enterobacteriaceae family), which are facultative, mobile and oxidase-negative anaerobic gram-negative bacilli that use citrate as the sole source of carbon. In the environment, citrobacteria are commonly found in water, soil and food; they are also occasional colonizers of the gastrointestinal tract in humans and, although the strains involved are considered to be of low virulence, they can be the origin of multiple types of infections (urinary, respiratory, intra-abdominal, surgical site, bone, central nervous system and bacteremia), representing 3-6% of all infectious diseases due to enterobacteria. They can cause community-acquired infections and infections associated with health care, affecting, especially, neonates (meningitis and brain abscesses), elderly and immunocompromised patients.
Along with Citrobacter koseri, C. freundii is one of the species most associated with infections. 14-15 Regarding its susceptibility profile, C. freundii has natural resistance to amoxicillin, amoxicillin/ clavulanate, ampicillin, ampicillin/sulbactam, cephamycins and first and second generation cephalosporins. Its acquired resistance to other β-lactams is given by the presence of ampC, extended spectrum β-lactamases and carbapenemases; resistance to fluoroquinolones and aminoglycosides has also been reported. 15
In this case, the infection occurred in a patient in whom acquired immunodeficiency was ruled out and who is outside the common age groups. For this reason, the possibility of developing the infection due to an episode of bronchoaspiration secondary to severe cognitive deficit that facilitated the passage of this germ from the gastrointestinal tract to the respiratory tract was considered. Regarding antibiotic therapy, empirical intra-hospital treatment with ampicillin/sulbactam and clarithromycin was initiated, following the recommendations of the Colombian guidelines for the treatment of community-acquired pneumonia in immunocompetent adults 16, in the context of a patient with a CURB-65 Severity Score of 1, with distant housing as a socioeconomic risk factor and with risk factors for gram-negative bacteria. Using ampicillin/sulbactam may explain the therapeutic failure of the first scheme due to the inherent resistance of C. freundii to this antibiotic. On the other hand, with the isolate of an ampC-producing and fluoroquinolone-sensitive strain, intra-hospital treatment with cefepime and outpatient scheme with ciprofloxacin was decided.
Conclusion
This is a clinically relevant case, since it is one of the few reported in Colombia of this entity 17 and the first one described by C. freundii. The absence of reports of cases of empyema necessitans in the country is noteworthy, given that, a higher incidence would be expected since this is an endemic area for tuberculosis. This observation could be explained by underreporting in the country or could be an indicator of a good effectiveness of the diagnosis and treatment of infections due to M. tuberculosis. Finally, this case is useful to illustrate the importance of considering this pathology in patients with pneumonia and parapneumonic effusions with poor response to treatment or with the appearance of associated pectoral mass, since this implies a change in the diagnostic and therapeutic approach, which may significantly affect the prognosis of patients.