Introduction
Airway management in patients with esophageal atresia represents an additional challenge for the administration of anesthesia and directly impacts perioperative out-comes.1 The most common esophageal atresia is type C (86% of the cases) presenting a closed esophageal proximal end and a distal end generating an abnormal communication between the trachea and the gastrointestinal (GI) tract through the fistula. The localization of the fistula is variable and should be assessed with perioperative bronchoscopy to ensure distal intubation and avoid overdistension of the stomach and subsequent ventilatory restriction.1
The use of perioperative ultrasonography for pulmonary evaluation has been rising in the last few years and, more recently, for perioperative airway evaluation.2,3 On the basis of its superior clinical value, it is now considered a skill that must be part of any anesthesiologist training.4-6 Selective ultrasound-guided intubation reports in the adult patient, have been published recently, but there are few publications in the literature regarding its use in the pediatric population.7 A novel application of perioperative ultrasound to confirm selective intubation in this clinical setting is herein discussed.
Case report
We present the case of a male 35-week preterm, 3-day-old patient with a postnatal clinical diagnosis of esophageal atresia, scheduled for repair after performing rigid bronchoscopy. There is a high suspicion of VACTERL association (vertebral defects, anal atresia, cardiac defects, tracheo-esophageal fistula, renal anomalies, and limb abnormalities) since, in addition to the esophageal atresia, the baby presents with polydactyly of the left hand. The echocardiogram shows a structurally healthy heart, the spine x-ray shows no abnormalities, but there is a double bubble sign in the abdominal films that heightens the suspicion of duodenal atresia. The blood work, renal function, electrolytes, and clotting times are normal for patient age. The physical examination shows considerable sialorrhea through the esophageal tube, stable vital signs, weight 1830 g, spontaneous ventilation with no signs of respiratory distress, oxygen saturation above 90% with oxygen at 1/16 l/min. Venous access was obtained via an epicutaneous catheter and 24-gauge peripheral venous catheter.
The patient was transferred to the operating room under basic monitoring, inhalation induction was performed with 2% sevoflurane, fentanyl 1 mg/kg, and propofol 1 mg/kg, and spontaneous ventilation was preserved. The presence of a tracheoesophageal fistula at the level of the carina was confirmed with the use of rigid bronchoscopy. On the basis of these indings, a joint decision with Pediatric Surgery was made to simultaneously perform the duodenal atresia and type C esophageal atresia repairs. In view of the localization of the istula, right selective intubation was performed to ensure isolation of the istula. Using rapid induction sequence (propofol 1 mg/kg, fentanyl 1 mg/kg, rocuronium 1.2mg/Kg), the patient was intubated at the first attempt using a Miller 1 blade and 3.0 tube that was advanced under auscultation guidance and held at a distance of 11cm to the right labial commissure, when respiration bruits in the left chest and epigastrial bruits were no longer audible.
Using a 12 MHz high-frequency lineal transducer, LOGIQ e Ultrasound (GE Healthcare, Chicago, IL)®, a bilateral, 6-quadrant systematic lung scan was performed, images on the right hemithorax were consistent with a normally ventilated lung, with pleural sliding at each respiratory movement and the M-mode "seashore" sign (Figs. 1 and 2).
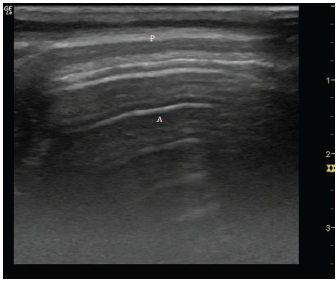
Source: Authors.
Figure 1 Hyperechoic pleural line (P=of the right lung and its reverberation phenomenon (lines A). (A) Indicative of normal, ventilated pulmonary parenchyma.
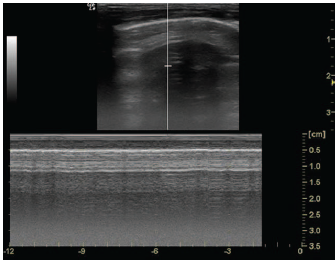
Source: Authors.
Figure 2 M-mode right lung with “seashore” sign indicative of ventilated normal lung.
In contrast, the left hemithorax showed images consistent with absence of ventilation, with no pleural sliding, pulmonary parenchymal consolidation due to lack of ventilation (also known as pulmonary hepatization), allowing for easy visualization of the cardiac chambers (Fig. 3).
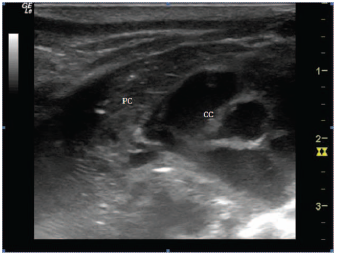
Source: Authors.
Figure 3 Left hemithorax with collapsed/consolidated (CL) left lung scanner image: visualization of cardiac chambers. (CC).
Following this ultrasound confirmation, the endotracheal tube was fixed 11cm from the right labial commissure, 2 cm beyond the usual depth for conventional intubation in this age group.
Both surgical repairs were completed, starting with supine decubitus transverse laparotomy in the supine position to repair the duodenal atresia, after which the patient was thoracotomy to repair the type C esophageal atresia. Throughout the procedure, the patient was under single-lung controlled ventilation, with permissive hypercapnia of up to 67 mm Hg, 70% FiO2 maintaining SpO2 above 90%. During direct exploration there was no evidence of stomach distension, confirming adequate endotracheal tube positioning during the procedure. The patient required hemodynamic support with epinephrine up to 0.15 mg/kg/min. After completing both procedures, the patient is repositioned in supine decubitus and a ultrasound imaging as described above is repeatedly obtained. With real-time visualization of the left hemithorax, the endotracheal tube is removed to a distance of 9 cm from the right labial commissure. Then, during lung recruitment, the line and pleural sliding was progressively observed, with gradual reduction of the collapsed lung image. Finally, A lines (Fig. 4) and the Mode M seashore sign were observed, confirming adequate left lung ventilation and the ultrasound window that enabled the visualization of the cardiac cavities due to air interposition, gradually disappeared.
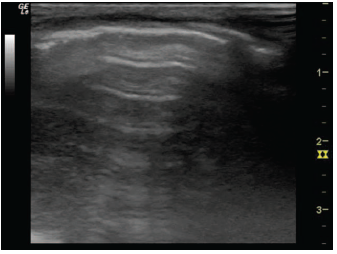
Source: Authors.
Figure 4 Right lung expansion following removal of the endotracheal tube - Pleural sliding.
The patient is transferred back to the neonatal intensive care unit (ICU) for postoperative management. The patient evolved satisfactorily, with progressive decrease of the ventilation parameters and hypercapnia; the patient was weaned from hemodynamic support and extubated 36 hours after surgery.
Discussion
The approach to airway management in patients with tracheoesophageal fistula-associated esophageal atresia is one of the major challenges in pediatric anesthesia, due to the need to ensure intubation distal to the fistula.1 Traditionally, selective intubation has been evaluated via auscultation, chest wall observation, radiography, and bronchoscopy. These clinical maneuvers are easy to evaluate, but their reliability is poor. Conventional radiology is highly reliable but requires transporting the equipment and exposes the patient to significant radiation. Bronchoscopy is the current gold standard for selective intubation, but in pediatric patients, this technique is complex and bronchial anatomy is difficult to identify, with the additional hurdle of patient desaturation and potential apnea.1,6 The above technical difficulties are even more significant in the premature neonate, making selective intubation a most challenging approach in this patient population. A suitable fiberscope was not available to evaluate such a small gauge tube position (3.0), therefore the initial case planning included the use of ultrasound to confirm selective intubation. However, a second check of the selective intubation was performed under direct vision during the initial rigid bronchoscopy.
Consequently, a new "point of care" scenario is considered, bringing the technology to the patient's bedside, for clinically relevant decision-making. In this particular case, pulmonary ultrasonography confirms selective ventilation and allows for postsurgical alveolar recruitment follow-up. Similar to other scenarios using ultrasound, pulmonary ultrasound evaluation is being used as a tool in airway management and for early diagnosis of pulmonary disease.2,3
The following findings are particularly relevant:
Pleural sliding
This is the image generated by the physiological friction between the the parietal and visceral pleural layers, which are hyperechogenic and confirms a healthy pleural cavity.2,3,6
Seashore sign
Visualization obtained in M mode that shows the static thoracic wall, followed by a hyperechoic pleural line, and then a granulated pattern representing the healthy lung parenchyma, with a cyclic pattern compatible with pulmonary pulse.3
Identifying these ultrasound pulmonary signs helps guide selective intubation and subsequent pulmonary expansion.
The increasing availability of ultrasound, its portable and reproducible nature, the low risk of radiation, and the possibility to do it at the patient's bedside make it a promising tool for clinical application in the management of selective intubation. Nevertheless, the difficulties that were mentioned must be considered when evaluating a preterm neonate as a candidate for this technique.
There is a gap in our knowledge that requires further studies to standardize the technique in pediatric patients and decide whether it can be adopted as a standard of care.
This report was approved by the Ethics and Research Committee of San Ignacio University Hospital. The parents signed the informed consent to use the patient's clinical information and images.
Ethical disclosures
Protection of human and animal subjects. The authors declare that the procedures followed were in accordance with the regulations of the relevant clinical research ethics committee and with those of the Code of Ethics of the World Medical Association (Declaration of Helsinki).
Confidentiality of data. The authors declare having followed the protocols of their centre of work regarding patient data disclosure.
Right to privacy and informed consent. The authors obtained the informed consent of the patient and/or subject reported in the article; the form is kept by the corresponding author.











 text in
text in 


