What do we know about this problem?
Fascial plane blocks are efficient interventions for postoperative pain control. However, the block of choice needs to be identified for optimal postoperative pain management after ovarian cancer surgery.
What does this study contribute?
The study confirmed the analgesic superiority of erector spinae block over transversus abdominis block in patients undergoing major ovarian cancer surgeries.
INTRODUCTION
Post-surgical pain is a significant patient concern. Ovarian cancer surgeries are accompanied by a considerable visceral disruption. These surgeries are frequently performed under general anesthesia (GA), which provides inadequate postoperative pain control 1.
The use of ultrasound-guided fascial plane blocks, such as transversus abdominis plane (TAP) and erector spinae plane (ESP) blocks, target the dorsal, lateral and anterior cutaneous nerves - chest and abdomen - in a simple, efficient way with little complications 2.
TAPB provided a reliable reduction of incisional pain and opioid usage in several studies. However, its deficient visceral pain relief may necessitate adding other modes of analgesia 3,4.
Many studies recommend ESPB as it showed a reliable perioperative pain control 5,6.
Despite the success of ESP and TAP blocks in reducing postoperative opioid consumption in previous studies, no study had ever compared their analgesic control of postoperative pain in adult patients undergoing major ovarian cancer surgery. The purpose of this randomized comparative research was to explore the analgesic superiority of either block in these patients.
METHODS
This prospective randomized double-blind comparative trial was conducted in the obstetric operating theater of Cairo University Hospitals, between July and December 2020. The intent of the study was to compare the analgesia of the US-guided ESP and TAP blocks in adult patients undergoing ovarian cancer surgery.
Sixty patients were recruited after acceptance by the ethics committee of the School of Medicine, Cairo University (ID: MS-104-2020) and upon registering at clinicaltrials.gov (ID: NCT04434339 on July 2020). Patients' approval to participate was documented by written informed consents.
Inclusion criteria: 18-65 year old patients, ASA class I - II (American Society of Anaesthesiologists), undergoing debulking surgery under G.A., with a vertical midline infraumbilical incision.
Exclusion criteria: ASA III-IV, patient's refusal, uncooperative patients, block site infection, failed block, pregnant patients, patients receiving vasoactive drugs, patients with the New York Heart Association (NYHA) class II-IV, BMI (kg/m2) of 18.5-30, psychiatric disorders, INR>1.5 coagulopathy, platelet count < 80000/ microL, hepatic insufficiency with ALT and AST > twice normal, and hypersensitivity to the study drugs.
Randomization: On arrival to the operating room, cases were allocated in a 1:1 ratio into ESPB group (no.=30) and TAPB group (no.=30), based on computer-generated randomization codes kept in sealed envelopes (EPIDAT 4.1). These envelopes were provided to the anesthetist in charge of performing the block by an investigator that was not involved in patient care.
In the ESPB group, cases had a preoperative ultrasound (US) guided ESPB on both sides. In the TAPB group, cases had a preoperative bilateral US guided lower TAPB. The anaesthesiologist who collected the data was blinded for which block was given.
Preoperative management: The participants were ordered to fast before the operation according to the standard guidelines. On the day of surgery, patients arrived at the preparation room 1 hour before the operation, to allow time to perform the block and to allow for a minimum of thirty minutes after the block, before induction of general anesthesia to ensure block success or failure by pinprick testing. A18G cannula was inserted to start intravenous fluids infusion and to administer a premedication of 0.02-0.03 mg/kg intravenous midazolam. All basic monitors were in place and the baseline readings of HR, SPO2, SBP, DBP and MAP were documented.
In the ESPB group, a mark was made on the required level (T10). It was identified by locating T7 spinous process as a middle of a line passing between the lower tips of the scapulae then going 3 spinous processes caudal to reach T10. The injection points are about 3 cm on either side of the midline. While the patient was sitting, the ultrasound transducer was positioned in a longitudinal parasagittal alignment using the HFL38X linear multi-frequency 6-13 MHz probe of SonoSite M-Turbo (Brothell, WA, USA) of a portable ultrasound system. The anatomical landmarks were identified, which consisted of the transverse process at the level of T10, the trapezius posteriorly, and the erector spinae anteriorly. 3 ml of Lidocaine 2% were injected subcutaneously, then, a 22-G spinal needle was advanced in-plane, targeting the transverse process tip under ultrasound guidance. After the needle tip reached the transverse process, twenty ml of 0.25% bupivacaine were injected on each side 7. This volume targeted to cover dermatomal levels from T10-T12 as a minimum.
In the TAPB group, while the patient was lying supine, the probe was positioned between the iliac crest and subcostal border at the level of the umbilicus, perpendicular to the mid-axillary line. The muscle layers of the anterior abdominal wall were identified and the plane was spotted between the internal oblique and transversus abdominis muscles. Following subcutaneous lidocaine 2% injection, a spinal 22-gauge needle was inserted in-plane under ultrasound guidance. A 20 mL 0.25% bupivacaine injection was administered 8. The block had the same steps repeated on the other side.
Intraoperative management: After transferring the patients to the operating room (OR), all basic monitors (ECG/ HR/SpO2/NIBP) were placed. G.A. was administered with 2 mg/kg propofol, 1ug/ kg fentanyl and 0.5 mg/kg atracurium. Following intubation, ETCO2 monitoring was initiated, and the patient was mechanically ventilated to maintain the ETCO2 at 35-40 mmHg. The HR, SPO2, SBP, DBP and MAP values were recorded every 20 minutes till the end of the surgery.
Anaesthesia was maintained with an end-tidal concentration of isoflurane 1-2%. Atracurium top-up doses of 0.1 mg/ kg were administered every 30 minutes. An additional fentanyl dose of 0.5 Hg/kg IV, for a maximum of 3 Hg/kg, was administered if HR ± BP increased > 20 % from the baseline in response to surgical stimulation, and the total fentanyl dose was recorded.
Postoperative management: Pain was evaluated at rest and documented using the visual analogue scale (VAS) after 30 minutes and then after 2, 4, 6, 8, 10, 12, 18 and 24 hours. Point zero was the time of recovery from the effect of general anesthesia. The time to 1st analgesic request was documented (the duration from "zero" point till 4 or more in the VAS). One-gram paracetamol IV was given every 6 hours regardless of the VAS value. Fifty mg tramadol IV were administered as rescue medication when the VAS score was 4 or more with 1 mg /kg every six hours as a maximum dose. A fentanyl PCA with a background infusion of 20 mic/hr , bolus of 10 mic and lockout interval of 10 minutes, was allowed if the maximum dose of tramadol failed to control pain to less than 4 (VAS) within 1 hour, and the patients were excluded from the study. The total consumption of tramadol was recorded.
The HR and MAP values were recorded after 30 minutes, and 2, 4, 6, 8, 10, 12, 18 and 24 hours. Complications in the form of local anaesthetic toxicity, nausea and vomiting (PONV), failed block, and injury to surrounding structures were documented
Outcomes
The main outcome was opioid consumption during the first 24 hours after surgery. Secondary aims were intra- and postoperative changes of HR and BP postoperative VAS, the time to first analgesic demand and postoperative complications. The time points for postoperative data were 0,30 minutes and 2, 4, 6, 8, 10, 12, 18 and 24 hours.
Sample size
The total sample size needed was a minimum of 60 cases (30 patients in each group) and 10 cases were added to offset any dropouts. This estimate was based on the results of a pilot study conducted with 10 patients in each group of the targeted patients in this study. The power analysis used the G power software 3.1.9.4 on tramadol consumption within the first 24 hours after the operation as the primary outcome. The pilot study showed a tramadol consumption of 31.8 ± 26.8 mg in patients who received ESP and 57.2 ± 25.2 mg in patients with the TAP block. Sample size calculation was done with the two-tailed unpaired T test for the difference between 2 independent means and accepting the cut-off for significance (a) of 0.05 and a power of 0.96, we considered the effect size as 0.976.
Statistical Analysis
Data analysis was done by Statistical Package for Social Science (SPSS) version 21.0. Chicago, Illinois, USA. The mean ± standard deviation and 95% confidence interval represented the quantitative data. Qualitative data were shown as the number and percentage of patients. The means were compared using the unpaired Student's t-test. Skewed numerical data were shown as median (range). Medians were compared using the independent samples median test. The proportions between two qualitative parameters were compared using the chi-square test. General linear model repeated measures ANOVA was used for comparison of serial measurements within each patient as within subject effect and group as between subjects' effect. The 2 tailed P-value < 0.05 was considered statistically significant.
RESULTS
Seventy patients were enrolled and 60 completed the study upon the exclusion of 10 patients. Four patients were excluded because they developed local skin infection and 6 patients experienced changes in the surgical plan. Table 1 illustrates the characteristics of patients and surgery.
Table 1 Characteristics of patients and surgery.
| Variable | ESPB (n =30) | TAPB (n =30) | |
|---|---|---|---|
| Age (years) | Mean (SD) | 52.4 (7.6) | 56 (5.5) |
| 95% CI | 47.5 to 57.3 | 52.2 to 59.8 | |
| BMI (Kg/M2) | Mean (SD) | 27.3 (2.3) | 27.7 (1.9) |
| 95% CI | 26.2 to 28.3 | 26.8 to 28.6 | |
| ASA I/II | 20/10 | 18/12 | |
| Duration of surgery (min) | Mean (SD) | 156.5 (31.6) | 163 (24.4) |
| Median | 155: 140-180 | 165: 140-180 | |
* Values are means (standard deviation (SD)), median: first-third quartiles, 95% confidence interval (95% CI) and numbers.
Source: Authors.
As regards the primary outcome (total tramadol use in both groups) a highly statistically significant difference was noted between the two groups (P < 0.001). (Table 2) 8 patients in the TAPB group and 2 patients in the ESPB group required the use of fentanyl PCA.
Table 2 Analgesia and PONV performance in the ESPB and TAPB groups.
| Variables | ESPB (n =30) | TAPB (n =30) | P value | |
|---|---|---|---|---|
| Total fentanyl consumption (mic) | Mean (SD) | 124.3 (24.1) | 154.7 (25.3) | 0.01 |
| 95% CI | 113 to 135.6 | 141.8 to 167.6 | ||
| Total tramadol consumption (mg) | Mean (SD) | 33.3 (30.6) | 77.3 (32.6) | < 0.001 |
| 95% CI | 16.2 to 50.4 | 59.2 to 95.4 | ||
| Time to first analgesic request in hours | Mean (SD) | 10.4 (9.6) | 1,2 (0.9) | < 0.001 |
| 95% CI | 5.5 to 15.3 | 0.7 to 1.7 | ||
| Median | 6:4-24 | 2:0.5-2 | ||
| Number of patients requested analgesia | 18 (60 %) | 30 (100%) | 0.008 | |
| PONV | 12 (40%) | 20 (67%) | 0.044 | |
Data are presented as means (standard deviation (SD)), median: first-third quartiles, 95% confidence interval (95% CI), percent (%)
Source: Authors.
All patients in the TAPB group demanded rescue tramadol, in contrast to only 60% in the ESPB group. The time to first analgesic request showed a highly significant difference between groups (P =< 0.001) (Table 2). The statistical difference in the intra-operative total fentanyl consumption between ESPB and TAPB groups was significant (P =0.01). The consumption in the TAPB group was significantly higher (Table 2).
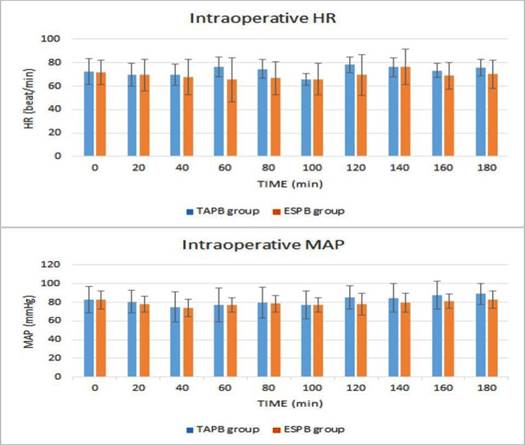
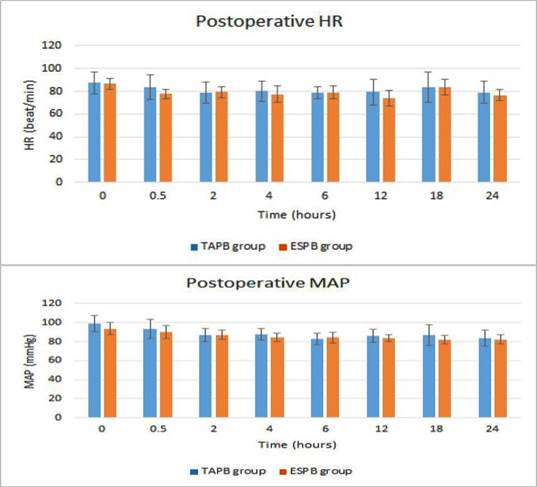
A statistically significant difference between the groups was reported in the intraoperative time points for HR F(1)=5.91, P=0.026. A statistically significant between-group difference was shown in the intraoperative time points for MAP F(1)=3.06, P=0.047 (Figure 1). Postoperative HR showed a significant difference between the 2 groups across the 8 time points F(1)= 5.1, P=0.02. Postoperative MAP showed a significant between-group difference across the time points F(1)=9.1, P=0.0002 with higher values in the TAPB group for HR and MAP (Figure 2).
Source: Authors.
Figure 1 Trends of the intraoperative HR and MAP in ESPB and TAPB groups. The vertical axis in each graph is for the estimated marginal means while error bars are for the standard deviation.
Source: Authors.
Figure 2 Trends of the postoperative HR and MAP in the ESPB and TAPB groups. The vertical axis in each graph is for the estimated marginal means while error bars are for the standard deviation.
The postoperative VAS variations in both groups showed a statistically significant difference (P =0.007) and (P < 0.001) for group ESPB and TAPB, respectively. VAS had a median of 2 1-3 and 4 2-6 for ESPB and TAPB groups, respectively. The VAS of both groups showed a statistically significant difference throughout the 24 hours postoperatively F(1)=18.15, P=0.001. The TAPB group had significantly higher VAS scores except at the postoperative 12 and 24 hours' time points. (Table 3).
Table 3 Comparison of the postoperative VAS between the ESPB and TAPB groups.
| VAS | TAPB (n =30) | ESPB (n =30) | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Mean | SD | 95% CI | MeanS | SD | 95% CI | ||||
| Lower Bound | Upper Bound | Lower Bound | Upper Bound | ||||||
| 0 h | 3.73 | 0.96 | 3.25 | 4.21 | 2.13 | 1.55 | 1.32 | 2.95 | < 0.006 |
| 30 min | 4.4 | 0.98 | 3.9 | 4.9 | 2.80 | 1.37 | 2.18 | 3.42 | |
| 2 h | 5.66 | 0.73 | 5.30 | 6.10 | 3.53 | 1.85 | 2.57 | 4.49 | < 0.003 |
| 4 h | 5.53 | 1.13 | 4.88 | 6.19 | 1.67 | 1.35 | 1.01 | 2.32 | |
| 6 h | 5.67 | 1.11 | 5.13 | 6.21 | 1.87 | 0.92 | 1.33 | 2.41 | < 0.001 |
| 12 h | 2.40 | 1.35 | 1.70 | 3.10 | 1.73 | 1.33 | 1.05 | 2.42 | 0.3 |
| 18 h | 4.20 | 1.26 | 2.94 | 5.46 | 2.27 | 1.03 | 1.73 | 2.80 | < 0.001 |
| 24 h | 3.73 | 0.79 | 3.33 | 4.13 | 2.73 | 1.62 | 1.92 | 3.54 | 0.05 |
*Data are presented as means [standard deviation (SD)], 95% confidence interval (95% CI), percent (%), h is for hours.
Source: Authors.
There were no reported complications except for PONV that showed a statistically significant between-group difference in the prevalence at the postoperative time points F(1)= 4.46, P=0.044. (Table 2).
DISCUSSION
The purpose of this double-blind, randomized comparative research trial was to investigate the preference of the analgesic properties of ultrasound-guided erector spinae block versus transversus abdominis block in patients undergoing ovarian cancer debulking surgery under general anesthesia. Although the comparison between ESPB and TAPB for analgesia after gynecological surgeries was a matter of interest among researchers, there are practically no studies comparing their analgesic efficacy in major ovarian cancer surgery as an example of extensive gynecological surgeries. This study suggests that ESPB analgesia is more efficient than TAPB under such conditions. This hypothesis was supported by our results, in which the ESPB group had a significantly lower intraoperative fentanyl and 24 hours postoperative tramadol consumption, lower 24-hour postoperative VAS, HR, MAP, longer time to 1st analgesic demand and a lower prevalence of PONV than the TAPB group.
The superiority of analgesia provided by ESPB over TAPB in our study can be explained based on their anatomy and how these blocks work.
In TAPB, local anaesthetic injection targets the nerve group running in the plane between the internal oblique and transversus abdominis muscles. This nerve group comprises the lateral and anterior cutaneous branches of the anterior rami of spinal nerves of the lower 6 thoracic nerves, intercostal, subcostal, first lumbar, iliohypogastric and ilioinguinal nerves 9. These nerves connect immediately above the transversus abdominis, therefore, the fascial distribution of local anaesthetic in TAP can offer somatic analgesia for the anterior and lateral abdominal wall 10.
Cadaver studies and contrast examinations assumed that ESPB works at the origin of spinal nerve. This was explained by the discontinuity of the muscles, allowing the injection to spread into the ventral and dorsal rami of the spinal nerves, then over the connective tissues between transverse processes to the paravertebral and epidural spaces. This would also block the rami communicants transmitting sympathetic nerves, allowing relief of somatic and visceral pain 2,11.
Several studies investigated the analgesia provided by TAP and ESP blocks in ovarian surgery. TAPB had a comparable analgesia to that of dexmedetomidine 12 and superior to that of local anesthetic infiltration. 13 Bisch S.P. et al. 14 reported a mean reduction of postoperative opioid use of 62% with continuous TAPB at time points from 24 for 48 hours. Bang S., et al 15. performed ESPB in a case of a large ovarian tumour, showing no pain levels above 4 at rest, or any rescue opioids requested during the first five days after surgery.
Other studies on gynaecological and obstetric surgeries found that ESPB provided more reliable pain control and less opioid usage than TAPB within the first 24 hours postoperatively 16-18.
The findings of a study on non-gynecological surgeries conducted by Altiparmak B., et al. 19 on laparoscopic cholecystectomy patients were consistent with our findings. However, they differed from the findings of a retrospective research trial by Tulgar, et al. on the same procedure which reported an insignificant difference between the groups 7.
The authors in this study targeted a procedure with more significant visceral manipulation and they did not use tramadol PCA which gives better control of pain in contrast to Tuglar's study. Additionally, Tuglar, et al. reported ESPB at T9 level, while the study of Altiparmak B, et al. which was consistent with our results, performed the block at T7, delivering better analgesic coverage during laparoscopic cholecystectomy.
Study limitations
The main limitations of this investigation were the use of tramadol on-demand instead of patient-controlled-analgesia (PCA) that could provide better quality analgesia. Yet, this did not affect the results. The time frame was only for 24 hours, but it was enough to make the results of the study statistically significant. VAS was reported only at rest, but, this did not affect the significance of the results. Therefore, further studies are essential to determine the best-individualized analgesic strategies for patients undergoing major gynaecological procedures.
CONCLUSION
Our results revealed that the ESPB provided a lower opioid consumption, more delayed time to first analgesic request, a lower VAS, HR and MAP within 24 hours postoperatively. It may then be concluded that the ESPB analgesic performance is superior to TAPB in major ovarian cancer surgeries.
ETHICAL DISCLOSURES
Ethics committee approval
This study was approved by the ethics committee of the School of Medicine, Cairo University (ID: MS-104-2020) and was registered at clinicaltrials.gov (ID: NCT04434339 on July 2020).
Protection of human and animal subjects
The authors declare that no experiments were performed on humans or animals for this study. The authors declare that the procedures followed were in accordance with the regulations of the relevant clinical research ethics committee and with those of the Code of Ethics of the World Medical Association (Declaration of Helsinki).











 text in
text in 



