Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO -
 Access statistics
Access statistics
Related links
-
 Cited by Google
Cited by Google -
 Similars in
SciELO
Similars in
SciELO -
 Similars in Google
Similars in Google
Share
Revista colombiana de Gastroenterología
Print version ISSN 0120-9957On-line version ISSN 2500-7440
Rev Col Gastroenterol vol.24 no.3 Bogotá July/Sept. 2009
Transverse colon tuberculosis. A case presentation and clinical review
Luz Mireya Cala MD(1), Edgardo Yaspe Costa MD(2), Carlos Serrano Mora MD(3)
(1) Clinical gastroenterologist, Caja de Compensación Familiar CAFAM. Bogota, Colombia.
(2) Clinical pathologist, Hospital Universitario de La Samaritana LABOPAT. Bogota, Colombia
(3) Clinical gastroenterologist. Institute of Gastroenterology, Clinica de Mary. Bogota, Colombia. serranomora50@hotmail.com
Received: 02-02-09 Accepted: 12-08-09
Summary
We describe the clinical case of a 90 year old female patient presenting weight loss and anemia. Physical examination detected an abdominal mass in the epigastrium. An abdominal scan revealed wall thickening at the transverse colon. When a colonoscopy was performed an infiltrating mass discovered. Biopsies diagnosed colonic tuberculosis. We present a literature review of digestive TBC, emphasizing colonic tuberculosis.
Key words
Tuberculosis, Colon, Digestive TBC.
PRESENTATION
The following is about a 90 year-old patient referred for gastroenterological examination because of anorexia, asthenia and weight loss. She did not present dysphagia, post-prandial plenitude, obvious abdominal pain, diarrhea, fever or digestive bleeding.
Her background revealed a prior ascariasis for which she had received treatment in 2007. She had also been treated for two urinary infections (E. Coli > 100000 col.). She had occasionally presented episodes of coughing which had been interpreted as bronchial hyperactivity. Her cough had improved with symptomatic medical treatment.
She was receiving treatment for arterial hypertension, lipid lowering medications, and occasionally took non-steroid anti -inflammatory drugs for osteoarthritis.
The physical examination found a weak and senile, but conscious patient with apparent nutritional deterioration. TA 120x90 FC: 72 x min. Weight 39.5 kg (1 year before she weighed 46.5 kg). Cardiopulmonary auscultation revealed only a discrete decrease in vesicular murmur. Abdominal palpation found a depressible soft abdomen and a hard, mobile, painless, intra-abdominal mass located between the epigastrium and the mesogastrium. It was approximately 5 cm. in diameter.
A check of results of routine lab tests performed periodically during the previous 18 months revealed a CBC with mild progressive anemia (initial 01/07: Hcto 38 - Hb 12.8 gr. up to Hcto. 32 Hb 11.0 gr. in 06/08), and normal leucocytes and platelets. However, the VSG was repeatedly elevated (45mm/hour). Glycemia, ALT, AST, DHL and TSH were normal. Creatine oscillated between 1.2 1.8 mg%. Proteinemia was 6.5 g., and albumen was 4.3 g. Protein electrophoresis and alkaline phosphatase were normal. An abdominal ultrasound showed colelithiasis.
An abdominal TAC was requested (figures 1 and 2) which showed a thickening of the transverse colon walls with extensive colonic diverticulosis. It suggested the possibility of diverticulosis in the resolution phase. No other intestinal or extra-digestive lesions were found.
Figure 1. Transverse colon thickening.
Figure 2. Transverse colon thickening.
She was referred for a colonoscopy which was performed under sedation. An ulcerated lesion, 50% infiltrated with stenosis, was found in the transverse colon towards the splenic angle (figures 4 and 5). It extended for approximately 5 cm. blocking the path of the endoscope toward the right hemicolon. Near and immediately next to the discrete lesion was a pedicure polyp of 15 mm. in diameter with an adenoma appearance (figure 3). The procedure had to be suspended immediately after obtaining a sample for biopsy because the patient experienced cardiac arrhythmia and hypotension. Nonetheless, the patient recovered completely in the post-procedure observation room.
Figure 3. Transverse colon polyp.
Figure 4. Ulceration and stenosis.
Figure 5. Infiltrating ulceration.
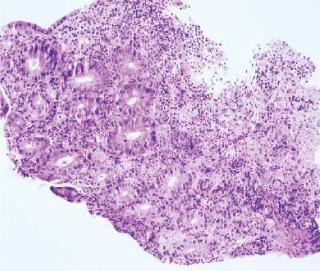
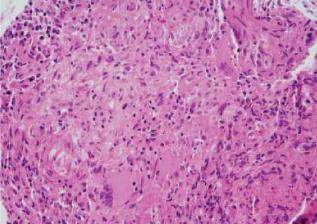
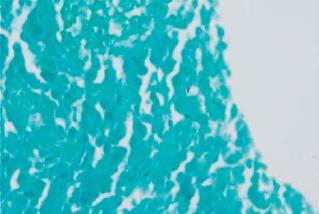
The pathological anatomy study of the colon biopsies showed an inflammatory process with ulceration and neovascularization (figure 6), the presence of monocytes, and PMN and granuloma formations without necrosis (figure 7). There was no malignancy. The special stainings were positive for BAAR (figure 8).
Figure 6. Inflammation and colonic mucosal ulceration.
Figure 7. Granulomas with giant multinucleated cells.
Figure 8. ZN (+) Staining for BAAR.
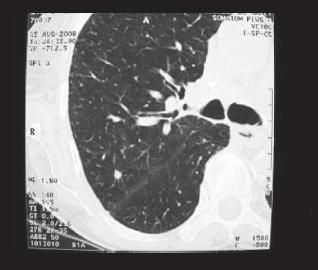
Afterwards, serial bacilloscopy and tuberculin studies were performed. The results were negative. A spiral CT showed apical fibrotic changes, a granuloma on the LSD and mediastinal ganglionic calcifications in the right hilum indicating that these findings were consequences of granulomatosis (figure 9).
Figure 9. Apical fibrosis and granuloma.
The patient is currently receiving medical treatment under the supervision of her health service. She has evolved satisfactorily in the sense that she has regained her appetite and has gained weight.
DISCUSSION
Since the nineties, TBC has reemerged as a very significant health problem for both developing countries and developed. It is frequently associated with HIV infection. It has been estimated that there are 7 to 8 million new cases in the world each year, while 2 to 3 million deaths are annually attributed to the infection (1).
Clinical studies show that even though TBC can affect any age group, it is more frequent in children and the elderly, especially those who are immunocompromised (HIV, chronic steroids use, other inmunosuppressors infliximab- and other systemic diseases associated with immunological dysfunction). It especially affects some racial and ethnic minorities, constituting a significant health problem in different geographical regions of the world (2).
Before effective treatments for TBC existed, 55% to 90% of the patients with fatal tuberculosis had their digestive apparatus compromised, particularly at the gastrointestinal level. It is estimated that today 20-25% of the patients with ileum and/ or colonic tuberculosis have pulmonary TBC.
The paths of gastrointestinal infection include dissemination through the intake of infected sputum, hematogenous dissemination of tuberculosis foci at the pulmonary level or in the submucosal lymphatic nodes, and local dissemination from the primarily infected neighboring organs (renal tuberculosis with fistulas).
Gastrointestinal TBC is pathologically characterized by inflammation and fibrosis of the intestinal wall and the regional lymphatic ganglions. These changes that can compromise the servos and create nodular masses are similar to those of Crohns disease.
From the macroscopic perspective, intestinal TBC can be classified into three categories: an ulcerative form which must be differentiated from Crohns disease, observed in 60% of patients; a hypertrophic form present in 10% of patients, and an ulcero-proliferative variation (pseudotumoral) observed in 30% of infected patients. The last two present a differential diagnosis with malignant neoplasms (cancer, lymphoma) or other infections (amebomas).
Intestinal TBC is most frequently located in the ileocecal region of the digestive tract. 80-90% of infected patients show only non-specific symptoms, such as anorexia and weight loss. Up to 30% of the patients have constipation. CPC may show anemia, while the leukocyte count can be normal. The tuberculin count is frequently negative.
Most cases of colonic TBC are located near the cecum and proximal ascendant colon. They are associated with ileal TBC. Only a few cases have been described at the level of the transverse colon in isolation. In fact, some authors believe that these are two different varieties, one ileocecal and the other colonic and rectal (3, 4).
Clinical manifestations, including anorexia, asthenia, and weight loss are generally vague indicators, but on occasion are primarily due to the degree of obstruction that the disease has generated. The finding of a palpable mass detected during the physical examination is a clear indicator, although they will in exceptional cases manifest as digestive hemorrhage (5).
Paraclinical studies include a colon Rx with contrast enema, an abdominal TAC and colonoscopy with biopsies for culture, PST and histological study. The last two are probably, the most specific methods for confirming the diagnosis.
In view of the risk factors and clinical evolution involved, a differential diagnosis must be performed to determine whether the symptoms indicate colonic TBC, Crohns disease, colon cancer, colonic non-Hodgkins lymphoma, or other infectious diseases such as ameboma and yersiniosis. The coexistence of colon cancer and colonic tuberculosis, although very rare, has been reported.
In all cases, medical treatment should ideally be performed by an interdisciplinary TBC treatment team. Patients with clinically manifest, low-risk intestinal obstruction must be taken into surgery. However, some authors accept the possibility of anti-TBC medical treatment in sick patients with a high clinical probability of colonic TBC, even when it has not been possible to conclusively demonstrate the disease at the histopathological level.
REFERENCES
1. Raviglione MC. The TB epidemic from 1992 to 2002. Tuberculosis (Edinburgo) 2003; 83: 4-14.
2. WHO. Global tuberculosis control report. Fact sheet No. 104, 2007.
3. Nélida Huamán-López. Tuberculosis intestinal y peritoneal. Revista de la Sociedad Peruana de Medicina Interna 2002; 15.
4. Misra SP, Misra V, Dwivedi M, Gupta SC. Colonic tuberculosis: clinical features, endoscopic appearance and management. J Gastroenterol Hepatol 1999; 14: 723-9.
5. T Namisaki, H Yoshiji, M Fujimoto, et al. Two cases of colonic tuberculosis presenting with massive melena. Int Journal of Clinical Practice 2004; 58: 1162-1164.
6. JF Álvarez, H Devarbhavi, P Makhija, S Rao, R Kottoor. Clinical Colonoscopic and Histological Profile of Colonic Tuberculosis in a Tertiary Hospital. Endoscopy 2005; 37: 351-356.
7. R Kaushik, R Sharma, AK Attri. Coexisting tuberculosis and carcinoma of the colon: a report of two cases and a review of the literature. Trop Gastroenterol 2003; 24(3): 137-9.
1. Raviglione MC. The TB epidemic from 1992 to 2002. Tuberculosis (Edinburgo) 2003; 83: 4-14. [ Links ]
2. WHO. Global tuberculosis control report. Fact sheet No. 104, 2007. [ Links ]
3. Nélida Huamán-López. Tuberculosis intestinal y peritoneal. Revista de la Sociedad Peruana de Medicina Interna 2002; 15. [ Links ]
4. Misra SP, Misra V, Dwivedi M, Gupta SC. Colonic tuberculosis: clinical features, endoscopic appearance and management. J Gastroenterol Hepatol 1999; 14: 723-9. [ Links ]
5. T Namisaki, H Yoshiji, M Fujimoto, et al. Two cases of colonic tuberculosis presenting with massive melena. Int Journal of Clinical Practice 2004; 58: 1162-1164. [ Links ]
6. JF Álvarez, H Devarbhavi, P Makhija, S Rao, R Kottoor. Clinical Colonoscopic and Histological Profile of Colonic Tuberculosis in a Tertiary Hospital. Endoscopy 2005; 37: 351-356. [ Links ]
7. R Kaushik, R Sharma, AK Attri. Coexisting tuberculosis and carcinoma of the colon: a report of two cases and a review of the literature. Trop Gastroenterol 2003; 24(3): 137-9. [ Links ]











 text in
text in