Introduction
The World Health Organization (WHO) estimates that about 25% of the world’s population is infected with Mycobacterium tuberculosis. Generally, extrapulmonary tuberculosis occurs in approximately 12% of tuberculosis (TB) patients1, and the most commonly affected sites are the mediastinal, retroperitoneal, and cervical lymph nodes, vertebral bodies, adrenal glands, meninges, and the digestive system2. Regarding the latter, the intra-abdominal manifestation only occurs in 3.5% of extrapulmonary TB. Notably, liver involvement occurs in up to 80% of the above cases3. Nonetheless, the manifestation of TB as a primary site in the liver represents less than 1% of the patients currently registered4. The authors Levine and Reed(5) agree on the first three forms of manifestation of hepatic TB as described below: granulomatous hepatitis accompanied by miliary TB, primary hepatic TB, focal tuberculoma, and tuberculous cholangitis or TB in the bile ducts. The most common symptoms for these scenarios are usually right upper quadrant pain, anorexia, weight loss, and fever. However, the literature describes the difficulty in diagnosing due to the similarity of the clinical and imaging pictures to other well-described and more common pathologies, such as cholangitis, hepatocellular carcinoma, and cholangiocarcinoma6.
Case presentation
This is the case of a 54-year-old female patient with a known morbid history of arterial hypertension on regular treatment with atenolol 50 mg once daily and cholecystectomy (cholelithiasis) surgery. Her medical record includes multiple hospital visits in the last five years due to a recurrent clinical picture of diffuse abdominal pain predominantly in the epigastrium and radiating to the right hypochondrium, which was sometimes accompanied by non-thermometered fever, with no predominance of time, and fluctuating jaundice.
In the last five years, she was evaluated in different health centers, reporting laboratory studies, digestive screening (universal erythematous gastropathy, with Helicobacter pylori +), and colonoscopy without pathological findings. In addition, an abdominal resonance was performed, obtaining axial and coronal planes in T2, T1, T2FAT-SAT, FASE, and FS images, with and without contrast medium. They showed an enlarged liver and preserved morphology, with multiple cystic lesions randomly distributed in both liver lobes and an annular enhancement of the contrast medium (Figure 1). Magnetic resonance cholangiography was also performed, which revealed significant dilation of the intrahepatic bile duct, specifically the left one, and a well-defined cystic lesion with regular borders, which caused dilation of the extrahepatic bile duct (Figure 2). After injection of the contrast medium, a filling defect was observed, suggesting choledocholithiasis in the left hepatic duct. A biopsy was performed that did not report findings suggestive of malignancy, so we decided to manage the acute clinical picture with antibiotic therapy (carbapenems) only and periodic follow-up of the lesion.
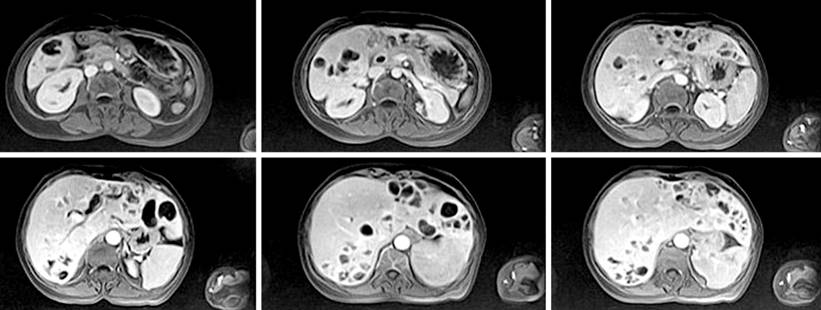
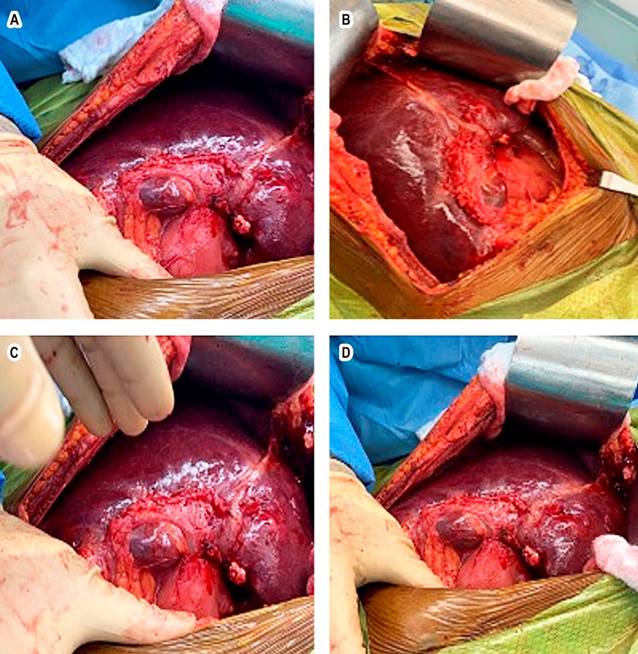
Figure 1 Abdominal resonance of axial and coronal planes. Liver measuring 22 cm in the longitudinal axis, regular borders, having multiple cystic lesions in both liver lobes with annular contrast enhancement. Source: Patient’s medical record.
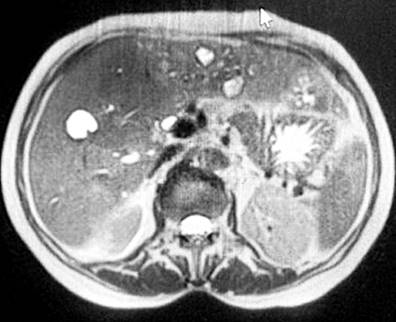
Figure 2 Magnetic resonance cholangiography showing dilation of the intrahepatic bile duct and a cystic lesion with regular borders. Source: Patient’s medical record.
On her last visit, the patient went to the emergency room with the symptoms described above, leukocytosis, increased bilirubin, cholestasis enzymes (Table 1), and jaundice in the sclera and mucous membranes. The diagnosis of cholangitis was assessed, for which an MRE cholangiography was performed, showing new findings in favor of multiple intrahepatic cystic lesions with an annular enhancement of the contrast medium and dilation of the intrahepatic and extrahepatic bile ducts. These findings were consistent with Caroli’s disease. An intervention with endoscopic retrograde cholangiopancreatography (ERCP) was made, in which a sphincterotomy was performed before cannulation. The discharge of choledocholithiasis and seropurulent content consistent with cholangitis was observed, later placing a 10 Fr/9 cm plastic prosthesis (Figure 3).
Table 1 Hematic biometrics
| Test | Result |
|---|---|
| WBC | ↑ 47.87 |
| RBC | ↓ 2.32 |
| Hb | ↓ 6.00 |
| Ht | ↓ 17.70 |
| MCV | ↓ 76.30 |
| MCH | 25.90 |
| MCHC | 33.90 |
| PLT | ↑ 484 |
| Erythrocyte sedimentation rate (RSV) | ↑ 140 |
| Differential | |
| Neutrophils % | ↑ 91.50 |
| Lymphocytes % | 1.00 |
| Lymphocytes # | 0.78 |
| Monocytes # | 1.57 |
| Neutrophils # | ↑ 43.77 |
| Chemistry | |
| Amylase | 62.0 |
| Lipase | 42.8 |
| ALT | 19.5 |
| AST | 21.3 |
| Albumin | ↓ 2.3 |
| Direct bilirubin | ↑ 1.4 |
| Indirect bilirubin | ↑ 1.1 |
| Total bilirubin | ↑ 5.0 |
| Chemistry | |
| GGT | ↑ 318.7 |
| Alkaline phosphatase | 327 |
| BUN (urea) | ↑ 47.9 |
| Creatinine | ↑ 3.2 |
| Fasting glucose | ↑ 113.0 |
| Potassium | 4.8 |
| Sodium | ↓ 124.4 |
| Calcium | 9.1 |
| Phosphorus | ↑ 6.1 |
| AFP | 5.1 |
| CEA | 1.7 |
| AC 19-9 | 15.6 |
| HIV, HBV, HCV | Negative |
| Autoimmune panel | |
| Complement, IgG, IgG4, and anti-LKM-1 | Within normal limits |
| QuantiFERON-TB-GOLD | Negative |
| Bacilloscopy | Negative |
| Miscellaneous tests | |
| Procalcitonin | ↑ 44.5 |
| D-dimer | ↑ 1500 |
| Lactate | 1.0 |
| C-reactive protein | ↑ 248.9 |
AFP: alpha-fetoprotein; ALT: alanine aminotransferase; anti-LKM-1: type 1 liver and kidney microsomal antibodies; AST: aspartate aminotransferase; BUN: blood urea nitrogen; CA 19-9: carbohydrate antigen 19-9; CEA: carcinoembryonic antigen; WBC: white blood cells; GGT: γ-glutamyl transferase; RBC: red blood cells; Hb: hemoglobin; Ht: hematocrit; IgG: immunoglobulin G; MCH: mean corpuscular hemoglobin; MCHC: mean corpuscular hemoglobin concentration; MCV: mean corpuscular volume; PLT: platelet count; HBV: hepatitis B virus; HCV: hepatitis C virus; HIV: human immunodeficiency virus; RSV: respiratory syncytial virus. Taken from the laboratory of Centro de Salud Clínica Corominas.

Figure 3 ERCP showing seropurulent content consistent with cholangitis. Source: Patient’s medical record.
We decided to take her to the operating room for left hepatectomy, with intraoperative findings of multiple cystic lesions (Figure 4). Hepatectomy was not performed, and a sample of the lesions described was taken for histopathological study purposes.
Diagnostic evaluation
Hepatic TB lacks pathognomonic clinical features or unique patterns in its manifestation; therefore, it is difficult to differentiate it from other more frequent pathologies that present with symptoms and imaging findings similar to hepatocellular carcinoma, intrahepatic cholangiocarcinoma, Klatskin tumor, and secondary liver abscesses4. Other approaches, such as fine needle aspiration cytology, have been used but are inconclusive. When evaluating the findings of ultrasound and computed tomography (CT), the usual results direct the presumptive diagnosis to malignancies or possible metastasis foci5. All of the above indicates the need for histopathological methods and GeneXpert as the reference test for definitive diagnosis. In this case report, the patient underwent different assessments (upper endoscopy, colonoscopy, magnetic resonance cholangiography, exploratory surgery, and liver biopsies) over the past five years due to the ambiguity of her clinical picture.
Three greyish-brown elastic fragments with whitish nodules, of which the largest measures 1.6 x 1 x 0.5 cm and the smallest 0.8 x 0.3 cm, were sent to the laboratory. The specimen was fully processed, and histochemical stains (reticulin, periodic acid Schiff [PAS], and Masson’s trichrome) were performed for microscopic evaluation.
In the microscopic evaluation, hepatic tissue with alterations of the standard architecture was seen due to an extensive area of caseation necrosis. Outside, epithelioid cells, Langerhans-type giant cells, and fibrosis were found. In addition, a remnant of hepatocytes with distorted architecture and portal spaces having a fibrous expansion, hydropic degeneration, and sinusoidal congestion was detected. In some areas, there was ductal proliferation. The conclusion of the liver biopsy indicated a granulomatous inflammatory process with caseation necrosis compatible with M. tuberculosis. Figure 5 shows a representation of the histological section. As a result, the pathology department suggested correlating the histopathological findings with the patient’s symptoms.
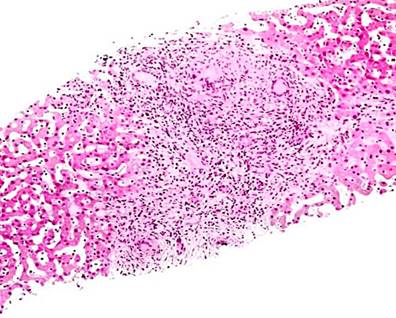
Figure 5 Histological section of liver tissue with giant cell granuloma. Source: Themes U. Mycobacterium tuberculosis11.
Considering the pathological and clinical imaging reports, extrapulmonary TB was diagnosed, and antituberculosis treatment was started.
Therapeutic intervention
In other case studies, the conventional antituberculosis regimen (isoniazid [INH], rifampicin [RIF], ethambutol [EMB], and pyrazinamide [PZA]) for six months has been the therapy of choice. Sometimes, it has been modified with micronutrient supplementation such as vitamin B67. For this patient, the standard treatment of two months of quadruple therapy with INH, RIF, EMB, and PZA was considered, followed directly by another four months of dual administration of RMP and INH. However, extrapulmonary and disseminated forms of TB may sometimes require more extended treatment, as is the case of bone manifestation (nine months), lymphoid manifestation (six months), or involvement of the central nervous system (one year)8. After three months of therapy, the patient showed improvement and decreased symptoms. The reserved prognosis remains.
Discussion
It is estimated that 6% to 38% of patients with intra-abdominal TB have evidence of pulmonary TB at diagnosis3. The pathogenesis pathway includes a hematogenous bacillus spread from a pulmonary focus. In 2017, Schininà et al.9 mentioned that of the 14 participants with hepatic TB included in their study, all had a liver lesion as a disseminated form of TB. However, hepatic TB as the primary infection focus is a manifestation with a particularly low incidence (less than 1% of TB cases worldwide)4. A systematic review published in 2015 by Hickey et al.10 showed that, among the reported cases of hepatic TB, 79% corresponded to miliary TB, while only 21% to local hepatic TB. Regarding the pathogenesis proposed for disseminating TB to the liver in the case of primary hepatic TB, the migration of the bacillus M. tuberculosis from a focus in the gastrointestinal tract is described. It travels through the intestine towards the portal vein and from there to the liver, where, even under unfavorable conditions such as low oxygenation of the liver tissue, this bacillus grows in 1% of the cases4.
Moreover, the manifestation of hepatic TB in the absence of miliary TB makes timely diagnosis and treatment difficult for health personnel by perfectly simulating other more frequent hepatic-biliary conditions5. Schininà et al.9 reported that the most common symptoms in their study sample were right upper quadrant abdominal pain, night sweats, weight loss, fatigue, high fever, upper abdominal tenderness, and hepatomegaly on physical examination. This picture is similar to that of the patient under study but is non-specific for the disease. Hickey et al.10 pointed out that in countries with endemic TB, TB was the leading cause of liver granulomas, and the presence of the latter is highly suggestive of infection by the bacillus in endemic countries.











 text in
text in