Introduction
Peritoneal tuberculosis was described for the first time in 1843 in a New York hospital, 39 years after the introduction of the concept of extrapulmonary tuberculosis by Laennec1. It represents 4.9% of all extrapulmonary causes of tuberculosis, surpassed in frequency by lymphatic, pleural, osteoarticular, genitourinary, and meningeal manifestations2. Surveillance systems have sought an earlier diagnosis; nonetheless, confirmation can be achieved once the disease progresses significantly due to nutritional, gastrointestinal, infectious, and systemic complications3.
Peritoneal tuberculosis is caused by the Mycobacterium tuberculosis complex (M. tuberculosis, M. africanum, M. bovis, M. caprae, M. microti, M. pinnipedi), which reaches the peritoneum by hematogenous dissemination, by lymphatic route, by contaminated foods, especially unpasteurized milk (M. bovis), or by direct extension of adjacent infectious foci such as the intestine or fallopian tubes. Chronic liver disease (alcoholic etiology), human immunodeficiency virus (HIV) infection, peritoneal dialysis in chronic kidney disease, neoplastic processes, and anti-tumor necrosis factor alpha (TNF-α) treatment represent the main risk factors for the development of peritoneal tuberculosis4.
It is a form of abdominal tuberculosis that frequently presents with non-specific abdominal pain of variable intensity, insidious progression in 50%-100% of cases, and subsequent obstruction of lymphatic drainage that results in blockage of peritoneal fluid reabsorption and ascites between 40% and 73% of patients. Constitutional symptoms such as weight loss, fever, and nocturnal diaphoresis may also be present5. Spontaneous bacterial peritonitis is the primary diagnosis to consider in the presence of ascites, abdominal pain, and fever. However, the persistence of ascites and signs of an inflammatory response in the cytological evaluation of the peritoneal fluid after treatment with conventional antibiotics points to a search for secondary causes of peritonitis, such as gastrointestinal perforation, therapeutic failure due to multidrug-resistant pathogens, and two very similar diseases regarding clinical manifestation and the findings in diagnostic imaging: peritoneal tuberculosis and peritoneal carcinomatosis6.
Case presentation
We present the case of a 61-year-old male patient of mixed race, of medium socioeconomic level, from an urban area, with a history of an ischemic cerebrovascular event of the left posterosuperior cerebral artery 5 years ago, treated with 100 mg of acetylsalicylic acid per day. He consulted the emergency department of a high-complexity clinic due to 15 days of lower limb edema, grade 3 ascites, hyporexia, involuntary weight loss of 10 kg, and dry cough. On physical examination, he was normotensive, without tachycardia, tachypnea, or desaturation, but cachectic (body mass index [BMI] of 17.3 kg/m²) with hepatomegaly and lower limb edema with grade II Godet’s sign.
His initial laboratory tests showed moderate thrombocytopenia (70,000/mL), mild liver injury (aspartate aminotransferase [AST]: 67 U/L, alanine aminotransferase [ALT]: 47 U/L, total serum bilirubin: 2.7 μmol/ L, indirect: 1.9 μmol/L). The unintentional weight loss syndrome study included antibodies to hepatitis C virus and HIV, which were negative, negative hepatitis B surface antigen, and non-reactive rapid plasma reagin.
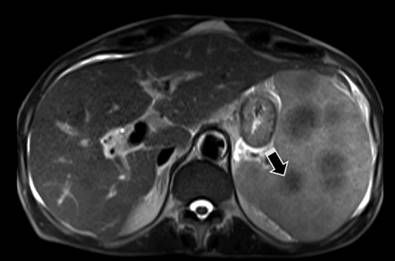
Abdominal computed axial tomography (CT) revealed splenomegaly with multiple nodular images in its parenchyma, focal alteration in the contour of the right hepatic lobe due to an isodense nodule, in addition to nodular involvement of the fat of the greater omentum and adenomegaly in the hepatic hilum and retroperitoneum, with ascitic fluid. Chest CT identified multiple nodular images in the lung parenchyma with granulomatous lesions in the middle lobe without other alterations. Similar findings were confirmed on contrast-enhanced abdominal magnetic resonance imaging (MRI), raising the possibility of neoplastic disease (Figure 1).
A diagnostic laparoscopy was performed with a biopsy, which macroscopically revealed multiple nodules in the parietal peritoneum smaller than 5 mm in all quadrants, with no other findings. Through a BLAKE drain, 500 mL of peritoneal fluid was obtained, which was cloudy and bloody in appearance, with lymphocytic pleocytosis (1,955 leukocytes/mm3, lymphocytes in 80% and neutrophils in 19.8%), hemoperitoneum (16,000 red blood cells/mm3), serum albumin-ascites gradient (SAAG): 1.1 g/dL, glucose: 81 mg/dL, protein: 2.4 mg/dL, albumin: 1.1 g/dL, lactate dehydrogenase (LDH): 115 U/L, without identifying microorganisms in the Gram stain or the Gomory stain or in the culture. A SAAG of 1.1 g/dL or greater suggests portal hypertension, and etiologies such as cirrhosis, alcoholic hepatitis, cardiac ascites, portal vein thrombosis, Budd-Chiari syndrome, and liver metastases must be considered, with no compatible findings in the images. Besides, his albumin level of less than 2.5 mg/dL was not related to renal losses but rather to global sarcopenia and his severe protein-calorie malnutrition. Therefore, despite the SAAG score, carcinomatosis versus peritoneal tuberculosis was proposed as a differential diagnosis, in which smear microscopy and Gene Xpert were negative for acid-fast bacilli (AFB). However, the adenosine deaminase (ADA) test reported a value of 178 IU/L, highly suggestive of peritoneal tuberculosis.
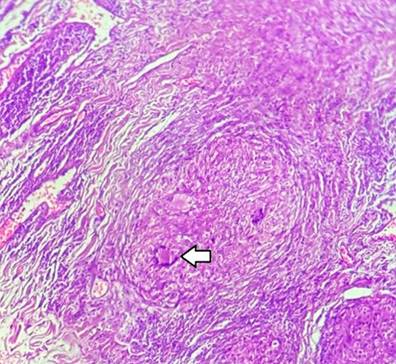
Histopathology of the peritoneum showed chronic non-necrotizing granulomatous inflammation consistent with peritoneal tuberculosis (Figure 2).
Given this result, infectious diseases began anti-tuberculosis management with isoniazid 75 mg, rifampicin 150 mg, pyrazinamide 400 mg, and ethambutol 275 mg, 4 tablets a day from Monday to Saturday, plus pyridoxine one 50 mg tablet/day. Two days after starting the tetraconjugate, the patient presented with altered alertness and dissociation of blood urea nitrogen (BUN)/creatinine associated with prerenal acute kidney injury and a hydroelectrolytic disorder due to severe hyperkalemia without electrocardiographic changes. They were treated with intravenous fluids, polarizing solution, calcium gluconate, and exchange resins. As a potential cause, he received a parenteral nutritional supplement for the management of severe malnutrition, so refeeding syndrome was likely. In addition, an alteration was detected in the liver biochemical profile with elevated transaminases, R index: 4.6, with direct hyperbilirubinemia and increased alkaline phosphatase, which led to the conclusion that the mixed hepatocellular and cholestatic pattern was due to drug-induced liver injury (DILI). Suspending management with anti-tuberculosis drugs was indicated, which produced a progressive decrease in transaminase levels.
While in the hospital, before returning to treatment with tetraconjugate could be contemplated, he presented with fever, tachycardia, hypotension, tachypnea, desaturation, and elevation of inflammatory markers, which required intubation and transfer to the intensive care unit (ICU) and initiation of a vasopressor regimen for the management of septic shock. Given the high suspicion of immunosuppression, infectious diseases indicated a broad-spectrum antibiotic regimen with vancomycin, meropenem, and caspofungin. Extensive consolidation in the left lung and bilateral pleural effusion were detected in the chest X-ray, while the fiberoptic bronchoscopy showed chronic endobronchitis without recent bleeding. Enterobacter cloacae was seen in blood cultures. General surgery performed percutaneous drainage of 1,500 mL of pleural fluid on the left side, 400 mL on the right and left a pigtail catheter. After 7 days of infectious hit therapy, the patient died due to multisystem failure resulting from sepsis of pulmonary origin.
Discussion
The diagnostic approach to peritoneal tuberculosis encounters three significant barriers: insidious clinical evolution, non-specific symptoms, and limited available diagnostic tests3. Additionally, the absence of specific clinical signs and the paucibacillary nature of the disease means that the diagnosis is based on histopathological studies of peritoneal biopsies obtained laparoscopically. Therefore, it is necessary to use a four-step model comprising conventional laboratory tests, imaging (ultrasound, CT, and MRI), microbiological laboratory, and histopathological study. Within traditional laboratory tests in the initial approach, the blood count can reveal a mild anemia of standard volumes and thrombocytosis, with elevation of the erythrocyte sedimentation rate and C-reactive protein and hypoalbuminemia7. Ascitic fluid, in macroscopic terms, tends to be described as sallow in 77% of cases, although it can also be cloudy, chylous, or bloody8. Within the cytochemical profile, a pleocytosis tends to be seen between 500 and 1,500 leukocytes, with lymphocytic predominance (>60% of the total cell count), the protein in the fluid is invariably 25 g/L, and the SAAG is lower than or equal to 1.1.
Ultrasound and CT reveal free or loculated ascites, lymphadenopathy, and peritoneal, mesenteric, and omental thickening. CT classically identifies high-density ascites, between 25 and 40 Hounsfield units9. Direct microbiological studies on peritoneal tuberculosis remain a challenge due to the suboptimal sensitivity of the available tools, the paucibacillary nature, and the dilutional effect of ascites10. The Ziehl-Neelsen stain in the ascitic fluid is positive in less than 6% of cases, and the culture yield is less than 58%. However, this performance can be improved by using a larger volume of peritoneal fluid (>1 liter) with centrifugation of the sample11. One study evaluated the sensitivity of Xpert MTB/RI in the ascitic fluid, which ranged between 8% and 50%, and better results were obtained when combined with staining, culture, histology, and the adenosine deaminase (ADA) test12. It must be considered that an ascitic fluid with a positive ADA test is highly suggestive of peritoneal tuberculosis, with an established cut-off point of 30 IU/L, which reaches a sensitivity of 93% and specificity of 96%13. The last step in the approach is the histopathological study, ideally of samples of nodular lesions of the peritoneum obtained by laparoscopy. It represents the gold standard for diagnosing peritoneal tuberculosis, whose typical description consists of granulomatous lesions made up of multinucleated Langerhans-type giant cells associated with areas of caseous central necrosis.
In the reported case, the clinical picture of abdominal pain of insidious evolution, ascites, weight loss, and fever, in addition to the diagnostic studies (conventional laboratory tests, diagnostic imaging, microbiological laboratory, and histopathology), allowed us to conclude the diagnosis of disseminated tuberculosis, both peritoneal/nodal and hepatosplenic. However, the diagnosis and the beginning of management with antitubercular tetraconjugate were late, taking into account that in the search for risk factors for an invasive infection, there was no apparent epidemiological contact initially, and a state of immunosuppression was very likely, but potential causes were not found. Pre-existing liver disease was suspected, although the images were not compatible with liver cirrhosis or portal hypertension. The delay in starting treatment influenced a progressive evolution of the natural history of tuberculosis infection in close relation to his precarious nutritional status, which facilitated the invasion of the peritoneum and, in turn, further aggravated malnutrition. All this resulted in the patient’s death from an infectious complication despite antibiotic management.
Conclusion
While peritoneal tuberculosis continues to represent an essential diagnostic challenge, it should be suspected in all patients with inflammatory ascites refractory to therapeutic paracentesis and antibiotic treatment, particularly in countries where tuberculosis is endemic, such as Colombia. No laboratory, histopathological, or imaging test is diagnostic in isolation, so a combined approach of ultrasound and abdominal CT, ADA testing, Xpert TBC/RIF, Ziehl-Neelsen staining, cultures in solid and liquid media, and biopsy of nodular peritoneum lesions is required. Therefore, the therapeutic approach to diagnose these patients must be adopted by a multidisciplinary team with the contribution of internal medicine, surgery, infectious diseases, and intensive care, as in the case concerned.











 text in
text in