Introduction
Crohn’s disease (CD) is part of the inflammatory bowel disease, and its manifestation is rare in Colombia: an incidence of 0.74 per 100,000 people per year (1. Meanwhile, tuberculosis (TB) is a more frequent entity, with an incidence of 22.6 to 28.9 cases per 100,000 inhabitants2, but intestinal involvement is uncommon; it only represents 3.5% of extrapulmonary tuberculosis cases3. Intestinal TB mainly affects the terminal ileum and cecum. It may result in the formation of ulcers and fistulas4, and in histopathological studies, granulomas can be found. It is one of the primary differential diagnoses in patients with suspected CD5.
Differentiating these pathologies represents a high level of complexity not only from a diagnostic point of view but also from a therapeutic one since some treatments, such as biologicals, may increase the risk of infections6. We present the case of a patient with pulmonary TB and CD.
Clinical case
A 28-year-old man presented with a 3-month clinical picture of abdominal pain and bloody, non-fatty diarrhea, which woke him up and persisted despite fasting. In the systemic inquiry, he reported occasional cough and involuntary weight loss of 30 kilograms in the last 3 years. Personal and family history was negative. A chest X-ray and CT scan were performed, suggesting TB; this entity was confirmed by bronchoalveolar lavage samples with Ziehl-Neelsen stain, PCR, and positive cultures, with no evidence of drug resistance. Colonoscopy showed colitis and ileitis with histopathology findings of chronic nonspecific ileitis and chronic nonspecific colitis with a focal active component. Due to the clinical context of pulmonary TB and with a high index of suspicion, intestinal TB was diagnosed, so the patient was administered rifampicin, isoniazid, pyrazinamide, and ethambutol.
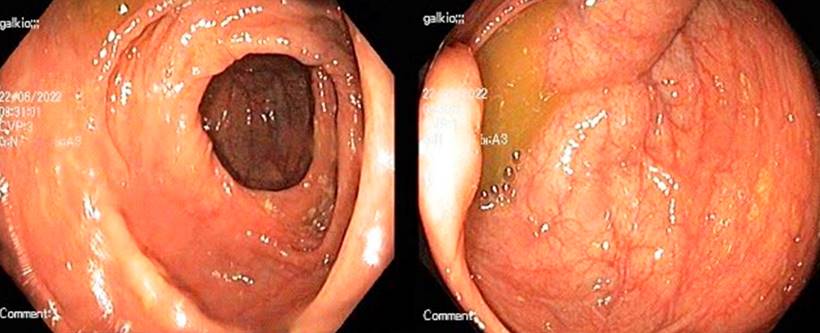
After 6 months, his respiratory and constitutional symptoms improved, but he was admitted to the hospital due to persistent abdominal pain and diarrhea. Adherence to antituberculous therapy was confirmed, and microbiological studies for TB were negative. The laboratory tests detected fecal calprotectin of 2,060 μg/g (Table 1) and the magnetic resonance enterography (MRE), intestinal sub-occlusion in the ileum (Figure 1). A new ileocolonoscopy identified cecal folds, appendiceal orifice, and ileocecal valve with severe edema covered by ulcers, easy bleeding, and edema involving the proximal ascending colon. In addition, biopsies were taken that reported inflammatory bowel disease with chronic ulceration and granulomas (Figure 2). The diagnosis of CD was made with a Crohn’s disease activity index (CDAI) of 421 points. Controversially, corticosteroids were postponed, starting treatment with azathioprine.
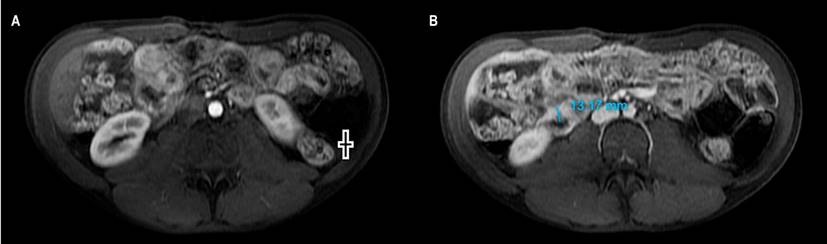
Figure 1 MRE with contrast. A. In the arterial phase: thickening of the ileus (+). B. In the portal phase: thickening of the ileum with a wall of 13 millimeters. Image owned by the authors.
Table 1 Patient laboratory findings
| Study | Result |
|---|---|
| Blood count | Leukocytes: 9.98 x 103 IU/L, neutrophils: 8 x 103 IU/L, lymphocytes: 1.2 x 103 IU/L, hemoglobin: 9.2 g/dL, MCV: 89 fL, RDW: 19.1 %, PLT: 503,000 |
| Albumin | 2.82 g/dL |
| Fecal calprotectin | 2,060 μg/g |
| HIV 1 and 2 antibodies | Negative |
PLT: absolute platelet count; RDW: red cell distribution width; MCV: mean corpuscular volume; HIV: human immunodeficiency virus. Table owned by the authors.
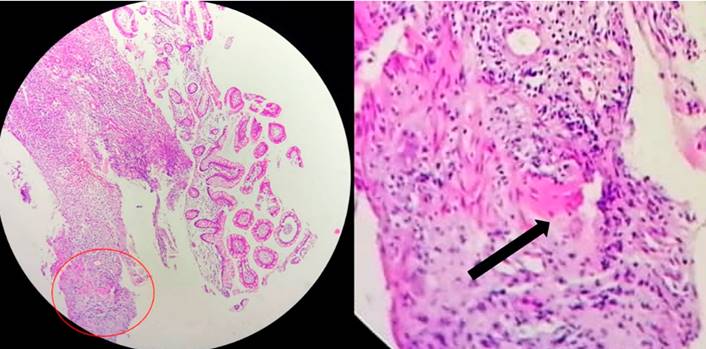
Figure 2 Biopsy: colon mucosa; in the submucosa, there is a non-necrotic, non-caseating granuloma with incipient multinucleated giant cells. Circle: granuloma. Arrow: giant cell. Image owned by the authors.
A month later, he consulted for abdominal pain, so a new CT scan was performed, which reported enteritis in the jejunum, pneumoperitoneum, and collections. He was taken to a laparotomy, noting obstruction of the proximal and distal small intestine, granulomas in the middle of the small intestine, perforation of the middle jejunum with a plastron that compromised the distal ileum, and a fistulous tract. An intestinal resection and anastomosis were performed. Once TB treatment was completed, biological therapy was started with adalimumab up to a maintenance dose of 40 mg subcutaneously every 2 weeks. The clinical evolution was favorable; 1 year later, he attended an outpatient gastroenterology check-up on clinical remission and without complications, and a new colonoscopy showed no alterations (Figure 3).
Discussion
CD usually occurs between the second and fourth decades of life, as in the present case7, with a certain predominance in women8. The patient had no risk factors, such as family history or smoking9.
In the case presented, the constitutional and respiratory symptoms led to a rapid diagnosis of TB, which could explain the gastrointestinal findings as an extrapulmonary manifestation. However, given the persistence of symptoms despite having implemented anti-tuberculosis therapy, CD was considered a differential diagnosis.
Although controversial and reserved for very selected cases, when there is confusion between CD and TB in countries where TB is frequent, some authors recommend a therapeutic trial with anti-tuberculosis drugs to corroborate the clinical improvement at 3 months and healthy mucosa at 6 months in almost 100% of patients with TB10, which did not occur in this patient. In addition, the MRE, histopathology, and laboratory findings, such as elevated fecal calprotectin (with approximate sensitivity and specificity of 90% and 80%, respectively)11,12 allowed the diagnosis of CD.
The patient had a moderate CDAI; steroids would be indicated13, but they were not started since the patient was finishing the second phase of treatment for TB. It should be clarified that steroids in doses greater than 15 mg of prednisolone each day confer an odds ratio of 7.7 for infections. However, this is not an absolute contraindication to starting them in cases like this14. Azathioprine is an alternative, although it does not induce remission of an active disease. Another option to consider, since it is a man under 35 years of age, would have been methotrexate to avoid the increased risk of hepatosplenic lymphoma due to thiopurines, but it is not recommended for the induction of remission of the disease13.
The patient had a stenosing and penetrating complication of CD. This event and being under 30 are risk factors for recurrence, which occurs in up to 84% of post-surgical cases15. It was decided to start biological therapy; vedolizumab, an antibody against α4β7 integrin, has shown benefit in CD16 and even good tolerance without an increase in the risk of opportunistic infections compared to placebo17. Even so, no evidence supports it as a first-line medication since it does not seem superior for the induction or maintenance of remission compared to other biologicals18. Thus, and adding to the complications and high risk of the patient, anti-tumor necrosis factor (anti-TNF) was started, which was a difficult decision since infliximab, for example, has shown a relative risk of 18.6 for TB activation19. There is no clarity on when to start anti-TNF in TB. Still, case series show safety in those with an evident clinical response, drug susceptibility results, and who have completed the first two months of the intensive anti-tuberculosis phase19,20.
Patients like this require multidisciplinary management where not only the gastroenterologist but also other specialties such as pulmonology, infectious disease, internal medicine, and coloproctology supervise their treatment.
Conclusion
The diagnosis of CD in a patient with TB is difficult due to the similarity of intestinal involvement between these two entities. The difficulty is also therapeutic since beneficial treatments for CD, such as steroids, can be omitted, and the start of biological therapy can be delayed. Considering the contraindications of these drugs and applying algorithms that allow the two entities to be differentiated is of great clinical use to improve outcomes and avoid complications.











 text in
text in