Introduction
Celiac disease (CD) is an autoimmune inflammatory disease that affects the small intestine’s mucosa in genetically susceptible individuals; gluten ingestion is the triggering factor, and symptomatic improvement is observed with its withdrawal. A prevalence of 1% is described in the general population; in South America, a prevalence of 1.3% is estimated, and it is higher in countries with Caucasian ancestry, such as Brazil and Argentina. There are few population studies in Colombia, so its prevalence is unknown; its manifestation is variable, from a silent course to malabsorption syndromes. In the last century, there has been an increase in the use of gluten-based products, which could explain the rise in cases.
Case description
We present the case of a 41-year-old male patient from Argentina residing in a rural area; he has a domestic partnership, two children, and is a pedagogical advisor. He has no significant previous history.
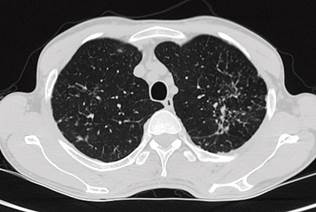
The clinical picture began after chest trauma due to a traffic accident. A chest CT was performed, and the incidental finding was apical fibrosis suggestive of tuberculosis (TB). He had no respiratory symptoms, and due to the imaging findings, he was taken for bronchoalveolar lavage with XpertMTB/RIF detection for TB. We decided to start tetraconjugate treatment with rifampicin/isoniazid/pyrazinamide/ethambutol (RHZE), and the first phase was completed with control of negative smears (Figure 1).
Source: Authors’ archive.
Figure 1 A chest CT shows fibrotic scarring changes in the left upper lobe with pleuroparenchymal tracts, traction bronchiectasis, and micronodules.
Since the beginning of treatment, the patient manifested gastrointestinal symptoms such as nausea, hyporexia, diarrhea, weight loss, and an increase in transaminases up to 5 times the upper normal limit, so the start of the second phase was suspended.
Once the transaminase values had normalized, the second phase of treatment with isoniazid and rifampin (HR) was initiated. Subsequently, the subject reported a reappearance of symptoms, so he consulted the emergency service. Given the severity, he was hospitalized for additional studies.
Liver and kidney tests and the hemoleukogram were normal, HIV was negative, and immunity studies with T lymphocyte subpopulation and immunoglobulins were normal. Stool, stool culture, and toxin C. difficile were negative; the colonoscopy and abdominal CT showed no abnormalities. In colon histopathology, eosinophils are slightly increased, with negative stains and no granulomas. A deficiency of vitamin B12, folic acid, and low prealbumin levels pointed to a probable cause of malabsorption.
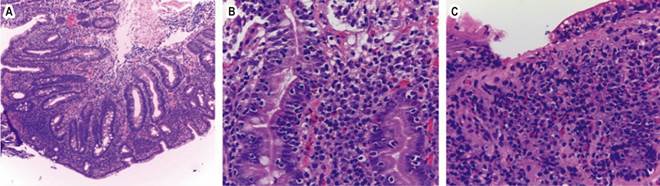
Given the patient’s origin, we studied less frequent causes of chronic malabsorptive diarrhea, such as CD. The antibody profile turned out positive, so an endoscopy (EDS) was performed to take duodenal biopsies (Table 1, Figures 2 and 3).
Table 1 Paraclinical results
| Paraclinical test | Result | Reference values for laboratory |
|---|---|---|
| Anti-transglutaminase IgG antibodies | 27.3 | Positive >10 IU/mL |
| Anti-tissue transglutaminase IgA (tTG IgA) antibodies | >200 | Positive >10 IU/mL |
IgA: immunoglobulin A; IgG: immunoglobulin G. Prepared by the authors.
Source: Authors’ archive.
Figure 2 A. Intestinal mucosa with villous atrophy, crypt proliferation (Marsh 3b), large mononuclear inflammatory infiltrate, predominantly lymphocytic (H&E, X1000). B. Lymphocytic infiltrate with exocytosis to the adjacent mucosa; no epithelial dysplasia observed (H&E, X400). C. Erosion of the mucosa due to the severe inflammatory infiltrate (H&E, X4009).
Source: Authors’ archive.
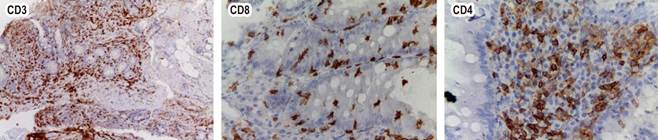
Figure 3 Immunohistochemistry: CD3 and CD8 positive in intraepithelial lymphocytes, CD4 negative in lymphoepithelial lymphocytes.
Considering the clinical symptoms, the results of complementary studies, and that the patient comes from Argentina, where the disease is most prevalent, the diagnosis of CD was confirmed. The timing between the start of medication and the manifestation of symptoms was striking, as well as the suspension of the drug that led to their resolution. Analyzing the potential relationship between the consumption of RHZE/pyridoxine and the symptoms of CD, we found that these medications may contain wheat-based excipients, which explains the patient’s symptoms not due to the adverse gastrointestinal effects of the antibiotic, but due to its excipients. Because of the patient’s residence, he based his diet on cultivated products without regular exposure to gluten derivatives, which explains the absence of previous symptoms that would guide the diagnosis.
The case was discussed, and the diagnosis of pulmonary TB was questioned since positivity was demonstrated in the molecular test only. Cultures were negative, and the patient was respiratory asymptomatic. TB was ruled out, treatment was suspended, and therapeutic efforts were redirected toward recovering the patient’s nutritional status. Subsequently, no other hospital admissions were recorded, and the patient remains respiratory asymptomatic, with weight gain and nutritional recovery.
Discussion
CD, sometimes called celiac sprue or gluten-sensitive enteropathy, is an autoimmune condition triggered by dietary gluten that occurs in genetically predisposed individuals. Specifically, it is characterized by enteropathy at the small intestine level associated with systemic symptoms caused by secondary malabsorption and anti-transglutaminase antibodies.
Initially considered exclusive to countries with predominantly Caucasian populations, cases of CD have been reported worldwide over the years, but its exact prevalence is unknown. According to data extracted from a systematic review of the global prevalence of CD, a global prevalence of 1.4% (95% CI 1.1-1.7) was estimated based on the positive result for anti-transglutaminase antibodies, and an overall prevalence of 0.7% (95% CI 0.5-0.9) when the diagnosis was confirmed by biopsy. Furthermore, its distribution in the continents was estimated; Asia had the highest prevalence with 1.8%, followed by Oceania and North America with 1.4%, Europe and South America with 1.3%, and Africa with 1.1%1.
An annual increase of 7.5% in the disease has been reported, possibly due to greater recognition, the application of screening methods, and improvements in diagnostic techniques2. The estimated prevalence in Latin America is 0.46% to 0.64%. It is estimated that it affects 1 in every 100 people in Argentina. There are few studies for Colombia and no exact data3,4.
We presented a patient from Argentina, where this pathology is common. Incidentally, the diagnosis of TB with tetraconjugate onset (RHZE) was made. Subsequently, the patient began with gastrointestinal symptoms and elevated transaminases. The clinical picture was assumed to be an adverse effect of the medication. Still, given the intensity of the symptoms, extension studies were initiated with evidence of malabsorption syndrome due to weight loss, hypoalbuminemia, and vitamin B12 deficiency.
With these suggestive symptoms, studies for CD were performed, initially with serological evaluation. Because of the positive TTG IgA result (>10 times the upper normal limit), an EDS was conducted with a duodenal biopsy showing villous atrophy and crypt proliferation, resulting in a Marsh 3b histological classification that confirmed the diagnosis.
Biopsy of the small intestine is of utmost importance. Microscopically, in CD, the villi are markedly atrophic or absent, but the mucosa’s overall thickness is average due to crypt hyperplasia. There is an increase in lymphocytes and plasma cells containing immunoglobulin in the lamina propria and an accumulation of fat globules representing partially absorbed lipids on the surface of the epithelium. Although far from being pathognomonic, the increase in intraepithelial T lymphocytes is also a characteristic finding; in some cases, the villous architecture is only mildly atrophic or completely normal, and increased intraepithelial lymphocytes (IEL) may be the only evidence of the disease.
The most widely used grading system for CD in biopsies is a modification of the Marsh (Marsh-Oberhuber) criteria adopted by national institutes of health: Grade 0 = normal; Grade 1 = IEL only; Grade 2 = IEL plus crypt proliferation; Grades 3 a, b, c = mild, moderate, and severe shortening of the villi, respectively; and Grade 4 = atrophic mucosa with flat villi5.
The duodenal biopsy displays severe atrophy of the villi of the intestinal mucosa with a large lymphocytic infiltrate, and immunohistochemistry showed positivity for CD3 and CD8; the severity of atrophy and the presence of CD8+ cytotoxic lymphocytes are specific findings for CD over other entities.
In this case, the onset of symptoms after anti-TB treatment was established is striking because, in his usual diet, the patient did not include gluten-based products; after reviewing the excipients of the RHZE tablet, wheat starch was found within the components of pyrazinamide, which explains the appearance of symptoms at the start of treatment and their resolution when stopping it in both phases of treatment.
A case with similar characteristics was published by Cerezo-Lajas et al. in 2016 in which, as in this case, the tetraconjugate under the Rimstar® brand (the same one that our patient received) was supplied. A similar chain of events was observed: When the treatment was started, the symptoms began, and as soon as it was suspended, the symptoms resolved6.
Conclusion
The CD is a rare pathology in Colombia, leading to doubts about its presence here. However, due to migration patterns and industrialization, an increase in cases is expected. Wheat derivatives are increasingly used in preparing foods and other products; for example, they are part of medication excipients, which was our patient’s diagnostic key.
The index of suspicion should be increased in patients with symptoms of malabsorptive diarrhea, evaluating their response to a gluten-free diet.











 text in
text in 



