Introduction
Located anterior to the spinal column within the posterior and superior mediastinum, the esophagus’s positioning renders injuries from trauma an uncommon occurrence. Literature suggests an incidence rate of approximately 10%1. The severity of these injuries is largely contingent upon the nature of the trauma and the involvement of adjacent critical structures such as major blood vessels, the airway, and the heart, with mortality rates ranging from 12% to 50% among patients presenting with any form of fistula. These percentages can rise in instances of undiagnosed conditions1,2.
Diagnosing esophageal trauma presents a significant challenge due to the potential for injuries to remain unnoticed. When esophageal injuries lead to contamination of neighboring structures, they are associated with high rates of morbidity and mortality due to the risk of local or systemic infections, including mediastinitis. This condition can progress to sepsis, shock, and ultimately, death. Additionally, complications such as the development of abscesses, tracheoesophageal, or esophagocutaneous fistulas necessitate complex surgical interventions at advanced stages3.
For any suspected case of esophageal injury, initiating antibiotic therapy and withholding oral intake are recommended to mitigate the high risk of mediastinitis. Surgical intervention serves as the primary management approach, supplemented by diagnostic imaging aids in patients without hemodynamic instability4.
Esophageal trauma is deemed a surgical emergency. However, management strategies have primarily been outlined through a limited number of retrospective studies and expert recommendations, including options such as exploratory surgery and endoscopy5. This context sets the stage for presenting a case study focused on the successful endoscopic management of a sharp force injury to the thoracic esophagus.
Case presentation
We report on a 28-year-old male, employed in informal work, with no notable medical history, who was transferred to our emergency department from a lower complexity hospital. The patient presented with a sharp force injury to the face and neck, which had occurred two hours prior and resulted in significant bleeding.
Upon initial assessment at the originating center, the patient received primary care that included wound irrigation and suturing, fluid therapy, broad-spectrum antibiotics comprising clindamycin 600 mg and gentamicin 240 mg intravenously, and a single dose of tetanus toxoid administered intramuscularly.
Upon admission to our secondary care facility, the patient’s vital signs were within normal ranges: blood pressure (BP) at 120/70 mm Hg, heart rate (HR) at 60 beats per minute (bpm), partial oxygen saturation (SpO2) at 95%, and no signs of respiratory distress. The patient exhibited generalized pallor, weighed 75 kg, had a height of 173 cm, and a body mass index (BMI) of 25.1 kg/m2. Physical examination revealed a sutured wound approximately 1 cm in length in region I of the neck at the sternal notch level, covered with a dressing without active bleeding, and a wound on the left temporal region with a dressing, showing signs of old bleeding, mild edema, and periorbital bruising. No subcutaneous emphysema was palpable, and no other significant findings were noted on examination.
An upper gastrointestinal endoscopy (UGIE) performed at a secondary institution revealed linear mirror-image wounds of 1 and 2 cm in length, located 25 cm from the dental arch, with an extrinsic perilesional hematoma. There was no clear evidence of a break in continuity, and the Z line and diaphragmatic pinch were observed at the same level without erosions. The preliminary diagnosis was a wound in the upper third of the esophagus with no complications (Figure 1), and the patient was advised against oral intake.

Figure 1 Linear mirror-image wounds of 1 and 2 cm in length. Courtesy of Dr. Edgardo Sánchez Gamboa.
The initial chest radiography was inconclusive, leading to further imaging with a contrast-enhanced neck CT scan. This imaging revealed the presence of air in the perivertebral, carotid, and retropharyngeal spaces, extending into the thoracic and posterior cervical regions (Figure 2). A contrast-enhanced chest CT scan confirmed a diagnosis of pneumomediastinum, indicated by a hypodense image consistent with air tracing from the neck through the visceral and prevertebral spaces and involving the mediastinum (Figure 3). A multidisciplinary team decided upon a repeat UGIE to attempt the placement of a fully covered self-expandable metal stent to avert the development of mediastinitis.

Figure 2 Neck CT scan with contrast, showing the presence of air in the perivertebral space with adjacent edema. Courtesy of Dr. Edgardo Sánchez Gamboa.
During the follow-up esophagoscopy, linear mirror-image wounds with well-defined edges, measuring 1 and 2 cm in length at 25 cm from the dental arch, were identified and approximated with two endoscopic clips each (Figure 4). A nasogastric feeding tube was placed under endoscopic guidance. The placement of a fully covered esophageal stent was deemed inadvisable due to its proximity to the cricopharyngeal muscle and the associated high risk of stent migration.
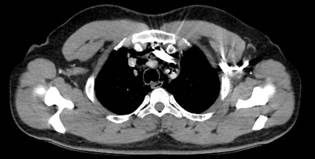
Figure 3 Chest CT scan with contrast, illustrating pneumomediastinum as evidenced by a hypodense air image in the visceral and prevertebral space. Courtesy of Dr. Edgardo Sánchez Gamboa.
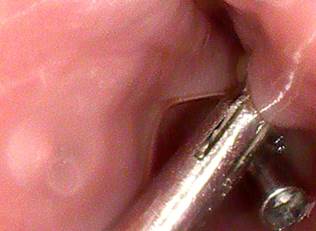
Figure 4 Linear mirror-image wounds approximated with double endoscopic clips. Courtesy of Dr. Edgardo Sánchez Gamboa.
On the seventh day following surgery, an esophagram was conducted to guide postoperative management strategies. This imaging study showed a satisfactory passage of contrast material through the esophagus into the stomach, without any indication of a tracheoesophageal fistula (Figure 5). Given the patient’s swallowing difficulties, another UGIE was advised.

Figure 5 Esophagram demonstrating appropriate flow of contrast medium through the esophagus. Courtesy of Dr. Edgardo Sánchez Gamboa.
During the third UGIE, a healing wound was observed in the proximal esophagus. The patient subsequently recovered without any complications or difficulties swallowing, leading to his discharge from the hospital.
Discussion
Esophageal trauma is acknowledged as a clinical condition linked to significant mortality. Hence, the essence of its management lies in the prompt identification and early intervention6. Surgical exploration is warranted for patients exhibiting hemodynamic instability, whereas stable patients might start with diagnostic imaging, such as plain chest radiography. This method is particularly useful for detecting free air within the mediastinum7. In our case, however, the initial chest radiograph did not provide conclusive results, prompting further assessment through UGIE, known for its 100% sensitivity in excluding injuries8. During the procedure, only a linear mirror-image wound was observed. There was no evident disruption of continuity, nor suspicion of mediastinal air, suggesting that withholding oral intake could be the most appropriate approach. Subsequent diagnostic evaluations, including contrast-enhanced CT scans of the chest and neck, confirmed the presence of pneumomediastinum. CT imaging has been documented as a valuable tool for identifying esophageal trauma and its associated local complications9, as the case we present.
Management strategies vary from conservative approaches, such as the cessation of oral intake, administration of broad-spectrum antibiotics, and radiological monitoring, to surgical interventions like esophagectomy. Situated between these conservative and surgical extremes is minimally invasive management via endoscopic techniques, reserved for patients without local or systemic complications who are stable from a hemodynamic standpoint10. In this case report, the patient maintained hemodynamic stability without any signs of an inflammatory response or clinical decline. Thus, the possibility of an endoscopic approach involving the placement of a fully covered esophageal stent was contemplated as a therapeutic option. However, this strategy was ultimately not pursued due to concerns over bronchoaspiration and intolerance of the device, largely because of its proximity to the cricopharyngeal muscle and a high risk of stent migration-a complication observed in up to 34% of patients with fully covered stents11.
Given the patient’s clinical stability, the specific locations of the two esophageal wounds, their linear nature with well-defined edges, and to circumvent additional complications, the decision was made to apply endoscopic clips to approximate the traumatic wounds. This method has rarely been delineated in the context of esophageal perforation treatment. Case reports have documented the use of over-the-scope clips (OTSC) and hemostatic clips, achieving up to a 100% effectiveness in restoring continuity in instances of esophageal perforation among patients undergoing peroral endoscopic myotomy (POEM)12. In contrast to our investigation, where conventional hemostatic clips were employed for esophageal perforation closure, there is scant literature, even though recent years have seen the introduction of less invasive techniques for gastroesophageal tract repairs. This topic remains contentious due to the lack of standardization in clip usage, with the preference still leaning towards the insertion of fully covered stents as the initial treatment choice13.
It is pertinent to mention that the European Society of Gastrointestinal Endoscopy supports the deployment of clips for sealing perforations of up to 2 cm14. Our study aligns with the criteria for such intervention, deemed an appropriate approach in patients exhibiting hemodynamic stability. Furthermore, there is a noted case of successful esophageal fistula correction using endoscopic clips in a patient suffering from esophageal trauma due to a foreign body. Follow-up examination revealed total resolution of the leakage15, reinforcing the potential of endoscopic clips as a viable emergency alternative for managing traumatic esophageal perforations.
Conclusion
Digestive endoscopy offers a minimally invasive therapeutic avenue, which results in decreased hospitalization duration, reduction in work-related leaves, lowered risk of systemic complications such as mediastinitis, and diminished pain from more invasive surgical techniques. At present, various strategies exist for the treatment of esophageal trauma, dependent on the patient’s hemodynamic condition, and the wound’s location, shape, and size, necessitating personalized treatment plans for each patient.











 text in
text in 



