INTRODUCTION
Nearly 77.3 million people have been infected with the human immunodeficiency virus (HIV) since the epidemic started, and by 2017 it was estimated that 36.9 million people were living with HIV, of which 75% knew their HIV status.1 This pandemic remains a major global public health problem; however, since the peak of AIDS-related deaths in 2004, deaths have fallen by more than 51%. In the absence of a curative therapy, HIV is currently a lifelong infection.1,2
According to official data from 1990 to late 2018, an estimated 13,000 people were living with HIV and/or AIDS in Argentina, reporting 5,800 HIV cases in average yearly between 2017 and 2018. In the Salta Province, the HIV rate per 100,000 inhabitants (2017-2018) is 18, with 40.9% late diagnosis.3 In addition, the accumulated expenditure on medicines in this province as of December 2017 had reached almost US$707,000, out of a total of US$30,577,996 invested in the country’s total in the same date.4 With the introduction of high-activity antiretroviral treatment (HAART), the morbidity rates associated with HIV and AIDS have been significantly reduced, making of this infection a chronic treatable disease if diagnosed in early stages.5,6
Although HAART improves the patient’s clinical, immunological and viral response, it is extremely necessary to maintain a high level of adherence to the prescribed therapy,6,7 since failure to achieve this would result in an increase in viral activity and possibly a rapid resistance to medicines,8,9 with studies showing that incorrect adherence is related to increased hospital costs, the evolution to AIDS, in addition to being the main cause of therapeutic failure.10 According to a meta- analysis by Costa et al in Latin America and the Caribbean, adherence to HAART was 70% and the main barriers to adherence to treatment were alcohol consumption, depression, unemployment, and the burden of pills.11
Stigmatization and the patient’s failure to accept his or her disease are, among other factors, causing the lack of adherence to treatment.
Studies in the period 2007-2011 on the attitude of oral health professionals show that these professionals and dental students have a negative attitude towards care for HIV-infected patients, and despite having adequate knowledge about the disease and relying on biosecurity measures, they consider that caring for these patients is not their responsibility.12,13 Garbin et al reported in 2018 that dental students’ attitudes towards the dental care of infected patients were considered discriminatory.14
Stigma is a serious problem for patients living with HIV-AIDS (PLHIV) as they refrain from seeking treatment, fail to disclose their serological status, and isolate from society. This deteriorates their quality of life and complicates the control of the disease. A literature review on dental care shows that the approach to this phenomenon includes not only identifying discrimination by health professionals and exploring the knowledge of staff working in dental services, but also recognizing and describing the main biosecurity practices and the possibility of risk and contagion in the professional environment.15,16 Several studies report significant associations between HIV-related stigma and high levels of depression, low social support, and low levels of adherence to antiretroviral drugs and access to and use of health and social services.17,18
The oral cavity is a commonly affected site in PLHIV.19 Many patients seek dental treatment, and here is where the dentist’s role becomes important in the early detection of the stomatological conditions that appear as a result of immunosuppression. For this reason, PLHIV need easy access to health care providers. In Chile, in a similar study in 177 PLHIV aged 40.1 years in average, there were oral lesions in 93.8% of patients with low TCD4 lymphocyte counts, with candidiasis being the most common pathology.19
There are several studies on the perception about health professionals. In 2010, García- Sánchez et al used surveys with a qualitative methodology, showing that there is omission and discrimination in dental care to people with HIV/AIDS because of dentists’ fear of contagion due to misconceptions or lack of information about the true means of transmission of the disease and the likelihood of contagion during dental consultation while recognizing the presence and use of biosecurity measures.16
A study conducted by Garbin et al in Brazil found that 60.4% of respondents have a good level of knowledge and 43.8% have a negative attitude towards PLHIV.14 There were more positive scores in a study in dental students, with 83% showing a positive attitude towards care for PLHIV; however, 66.7% did not have a good level of knowledge on the subject.14
On the other hand, there are few reported studies regarding the perception about the dental benefits by people affected with this disease.
The objective of this study was to determine the appraisal of PLHIV on dental care, in relation to demographic characteristics of the study population, the dental institutions where they are treated, and the reasons for concealing their diagnosis.
METHODS
A descriptive study was conducted. The study population consisted of all the PLHIV who attended the Provincial HIV/STIs and Viral Hepatitis Program, which operates under the Ministry of Public Health, in the province of Salta, in the period June-September 2015.
The research protocol was approved by the Advisory Committee on Teaching and Research (Ethics Committee) of the Hospital Señor del Milagro in Salta, Argentina.
A structured, self-administered, multi- response survey was created under the advice of the HIV/STIs Program, and administered by a psychologist who made part of the team of researchers. The survey was approved by three dentists: the head of the hospital’s dental service and two specialists in stomatology working at Salta hospitals. A pilot test was carried out with 36 surveys, and some modifications were made, thus obtaining the final questionnaire that was applied to the PLHIV.
To apply the survey, illiterate persons, patients under 15 years of age, and those who did not agree to answer were excluded. The document was delivered in a closed envelope, and once an informed consent was signed, the patients answered the survey anonymously, depositing the informed consent in one ballot box and the answered survey in another. At the end of the study, the number of both informed consents and surveys were counted to verify that they matched the number of study participants.
The survey consisted of 12 questions, including the following variables: age in years, date of HIV/AIDS diagnosis and time of evolution of the disease in months, gender (male, female and transgender); place of origin, and if dental care has been received in the last two years.
Other items included: if patients consulted public hospitals and health centers (public services) or private dental care offices (private services) and the reason for seeing a dentist (health or esthetic reasons), if they usually disclose their serological status (yes/no) during dental care, the preferred places for dental care (general or specialized places) and whether they perceive that the dentists have knowledge on HIV/AIDS.
A descriptive statistical analysis of the results was performed, tabulating and analyzing the data on an Excel© spreadsheet.
The categorical variables were expressed in frequency and percentage, and the continuous ones in means or standard deviation, with 95% confidence. The categorical variables were compared by Chi2 or Fisher’s exact test and the continuous ones by Student T-test or Mann-Whitney T test according to their distribution. A value of p < 0.05 was considered significant.
RESULTS
200 PLHIV were surveyed. They were 37 years in average (IQR 29.2-45.0). The time of evolution of the disease did not have a normal distribution, so the median evolution of the disease was 78 months (IQR 30-126); 82% of patients were from the Salta capital. There was a predominance of males with 108 (54%), and 13 (6.5%) transgender patients (Table 1). In comparing the general characteristics of the three genders, female patients were 40 years in average, males were 37 years, and transgender 34 years in average (p = 0.8); concerning the time of disease evolution: 102 months for females, 81 for males, and 75 for transgender, but these differences were not significant (p = 0.09).
Table 1 General data of surveyed patients (n = 200)
| Variable | n = 200 |
|---|---|
| Age in years - m (IQR) Male - n (%) | 37 (29.2-45.0) 108 (54.0) |
| Female- n (%) | 79 (39.5) |
| Transgender - n (%) | 13 (6.5) |
| Time of evolution from diagnosis (in months) - m (IQR) | 78 (30-126) |
| From Salta capital - n (%) | 165 (82.5) |
| From inner Salta - n (%) | 35 (17.5) |
Source: by the authors
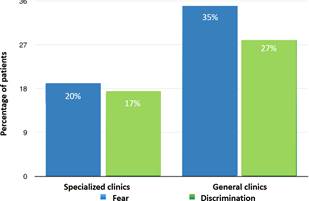
78% of patients consulted a dentist in the last two years and 80% indicated that oral care was more important for health than esthetics. 70% considered dentists to be trained and knowledgeable about HIV. 60% of surveyed patients sought help in public dental services, with 37% opting for various public hospitals in the province of Salta, and 23% for health centers both in the capital and throughout the province. The remaining 40% preferred to be treated in private offices (Figure 1).
Source: by the authors
Figure 1 Distribution of respondents according to place for dental care (n = 200)
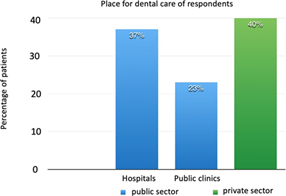
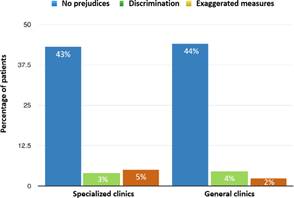
56.5% of respondents said that they prefer to be treated at general care centers, such as public hospitals, health centers, or private offices. The rest admitted that they prefer to go to places specialized in treating people living with HIV/AIDS. It was observed that 50.5% disclose their diagnosis to the treating professional and that they are treated with no prejudices (87%), although the remaining 13% felt discrimination or perceived that biosecurity measures were exaggerated, with no differences between the public and private sectors (Figure 2). Among those who choose not to disclose their diagnosis to the treating dentist, 54 patients argue that it is not necessary, and 55 are afraid of being discriminated. These numbers include both specialized and general clinics and are shown in percentages in Figure 3. There were no differences in age, gender, or time of disease evolution since diagnosis among those who disclose the diagnosis and those who do not (Table 2).
Source: by the authors
Figure 2 Appraisals on care type by patients who disclose the diagnosis (n = 101)
Table 2 Characteristics of PLHIV depending on whether or not they disclose their diagnosis in dental care
| Disclose the diagnosis | p | ||
|---|---|---|---|
| Yes | No | ||
| From the capital (n = 165) - n (%) | 93 (56.3) | 72 (43.7) | < 0.001 |
| From inner Salta (n = 35) - n (%) | 8 (22.9) | 27 (77.1) | |
| Transgender (n = 13) - n (%) | 6 (46.15) | 7 (53.85) | 0.08 * |
| Non-transgender (n = 187) - n (%) | 95 (50.8) | 92 (49.2) | |
| Time of evolution (months) - X (SD) | 96 (68.0) | 82 (67.0) | 0.14 ** |
| Age (years) - X (SD) | 38.8 (11.1) | 38 (11.6) | 0.62 ** |
| Public sector (n = 119) - n (%) | 68 (57.1) | 51 (42.9) | 0.03 * |
| Private sector (n = 81) - n (%) | 33 (40.7) | 48 (59.3) | |
| Prefers general center (n = 113) - n (%) | 51 (44.2) | 62 (54.8) | 0.06 * |
| Prefers specialized center (n = 87) - n (%) | 50 (57.5) | 37 (42.5) |
* by Chi2 test ** by Student T-test
Source: by the authors
Communicating the diagnosis to the treating dentist was statistically significant in patients from inner Salta and who prefer the public sector (p = 0.03). There was a greater, but not statistically significant, tendency to disclose the diagnosis among non-transgender patients and those who prefer a specialized center (p = 0.08) (Table 2).
DISCUSSION
The present study in PLHIV aimed to determine the appraisal on the dental care offered in the province of Salta, based on a survey with 12 questions, of which 6 asked about this specific topic.
With regard to gender, male patients were predominant (54%), similar to studies conducted by Pantoja and Estrada,20 but different from the study by Elizondo et al,21 in which out of 134 PLHIV, 30% were women and 70% were men, or Rungsiyanont et al,22 in which out of 299 PLHIV, 28.6% were men, 71% were women and 0.3% were transgender, in contrast with the present study, where 6.5% belonged to the latter. population the median age in our study group was 37 years (IQR: 29.2-45), comparable to the above-mentioned studies.20-22 In relation to the time of evolution of diagnosis, the median for this group was 78 months, similar to other studies.22-26
Studies in Latin American countries suggest that PLHIV may have trouble accessing dental care.20 78% of the study population saw a dentist in the last two years and 80% stated that oral care is more important for health reasons than for esthetics. To assess this variable, further studies can be conducted using the indexes of decayed, missing, filled teeth (DMFT), such as those performed by da Costa et al,27 who related oral health status with the quality of life of PLHIV. The authors measured the DMFT index and correlated it with the degree of depression, concluding that in this group of patients there was an association between high DMFT rates and depression.
Access to dental services by PLHIV around the world varies between clinics specializing in PLHIV care and non-PLHIV clinics.19,21,23-26In this study, 60% of respondents sought dental care in the public sector and the rest consulted private clinics. In turn, 56.6% indicated that they prefer to be treated in regular places, such as hospitals, health centers, and private offices, just as non- PLHIV people, as Aguilera et al also found. However, Elizondo et al observed that males prefer to go to a private dentist, perhaps because this group has a higher monthly income than women.21
Timely comprehensive dental care is highly important for people living with HIV/AIDS because of the common manifestations of the syndrome.19,23 Health professionals are one of the main providers of support for PLHIV in both the health and personal dimensions. It has been reported that an actual or perceived stigmatizing attitude by the professional22,26 has a negative impact, eventually causing non-adherence to treatment, irregular attendance to consultations, and sometimes total abandonment of health care.12
The present study highlights the attitude of dentists in the province of Salta, since a high percentage of PLHIV who disclose their diagnosis perceive no prejudices in the service, an attitude that could favor adherence to treatment. 50.5% of the study population discloses its diagnosis, a higher proportion than studies carried out in other countries.20,25 Among those who choose not to disclose their diagnosis, 54.5% do so for fear of discrimination. In the Elizondo et al 21 study, 48.7% of women and 30.9% of men informed the dentist of their HIV+ diagnosis. Although PLHIV (61.5% of women and 78.7% of men) consider that it is important for the treating professional to be aware of their HIV condition, they do not disclose it because they fear they would be denied attention or that inconveniences would arise during dental care (62.5% of women and 43.6% of men). In turn, 65.0% of women and 70.3% of men believed they had the right not to disclose their HIV status to the dentist.21 13% of the surveyed patients in our study perceived exaggeration in biosecurity measures, a lower percentage compared to the findings by Aguilera et al25 (78%) and Pantoja et al.20 These results contrast with studies in Saudi Arabia, where 98.1% of 430 surveyed general dentists put off HIV patients to the last appointment in the day, while 84.7% refer them to a specialist. In addition, 100% reported double-glove use and that discrimination against these patients was 33% higher in private clinics than in government institutions.28 In our study, 70% of patients perceived that dentists knew about HIV/AIDS, which does not necessarily reflect the level of knowledge that professionals may have. It is therefore suggested for future studies to compare what the patient perceives about the dentists’ knowledge and the actual knowledge they have, since studies measuring these variables are lacking.
It should be borne in mind that lack of acceptance of the disease influences adherence to treatment, and considering the high percentage of satisfactory and non-judgmental care, it is suggested to incorporate strategies for the professional practice to influence the reduction of stigmatization and therefore cooperate with adherence to treatment.
While this survey measures many parameters in relation to PLHIV appraisal on dental care, the measuring instrument could be refined and transformed into a Likert survey, which measures different dimensions in relation to the quality of care offered by dentists and thus further refine some of the content. Also, based on these results, qualitative or mixed research projects could be conducted with a different research design, as done by García- Sánchez et al.16
Among the limitations of this study is the sampling for convenience, as the survey was applied to patients attending the program. A stratified sampling is therefore suggested in relation to the rural and urban population, as well as by gender.
While the quantitative approach of studies on perception has some limitations, surveys can be considered as the best way to conduct these types of research projects.
CONCLUSION
PLHIV’s appraisal on dental care was positive because there were no prejudices. On the other hand, some patients consider it appropriate not to disclose their diagnosis for fear of discrimination or because they think it is not necessary. However, there was a low percentage of discrimination and stigmatization, which could be further reduced with additional education and training for dental staff, auxiliaries, and secretaries. Interdisciplinary work would help PLHIV in comprehensive care, thus avoiding one more reason for non-adherence to treatment.