Introduction
‘Health literacy’ is the expression used to describe the ability to use information in health care services. It concerns the personal characteristics and social resources necessary for individuals and communities to access, understand, evaluate, and use information and services to make health-related decisions. It includes the ability to communicate, assert, and act upon such decisions (1-4).
The health literacy approach and shared decision-making are considered important tools that increase patient safety and improve communication between health care professionals and their patients (5, 6), which can favor better patient participation and autonomy in their care process. In this sense, the Agência Nacional de Vigilância Sanitária (National Health Surveillance Agency) guidelines emphasize the combination of health literacy and patient safety by improving the communication process which is essential for the development of a partnership relationship. Health care services with a safety culture centered on patient and family care must ensure the quality of communication at all levels of care as an integral part of health care (7, 8).
Primary health care (PHC) is considered to be the patient’s gateway to the Brazilian Unified Health System (better known by its acronym, SUS), where first contact takes place and basic care is provided by the health care services in which the population concerned lives or works (1, 9, 10). Even though they are in the same territory, PHC can come across a variety of people at different levels, who, to be welcomed in a comprehensive and qualified way, require an approach based on health literacy so that communication is effective (11, 12).
In the Shanghai Declaration 2020/2030, three cornerstones were established to promote health: Good governance, healthy cities, and health literacy. Health literacy was widely discussed at this conference, which took place in 2016 (1). Since then, the aim has been to improve it through better access to information and to enable people to make more informed decisions about their health and that of their families, from which they can more effectively advocate their political views and formulate adequate public policies (3, 13-15).
Health promotion addresses this wide range of determinants through a combination of strategies, including health promotion in all policies and the creation of supportive health environments; it also improves personal health literacy and health competencies. The drive to address health determinants is intrinsically linked to health equity and is fundamentally concerned with the distribution of power and resources within populations (14, 16-19).
The aim of studies on health literacy and patient safety is to help transform health care organizations into health literacy-responsive organizations, redesigning their structures and processes to support patients with low levels of health literacy to understand and use information and services to maintain their own health (20-22).
However, there is a growing need to further understand the effects of personal care experiences (e.g., patient-centered care) and patient-specific factors (e.g., socioeconomic status, health beliefs, level of health literacy) on patient-reported outcomes regarding health care provision quality (e.g., satisfaction with care). Improved insights into these interrelationships would enable the development of measures to initiate organizational change toward a more patient-centered and health literacy-friendly environment.
Initially, a preliminary search was conducted using the following descriptors: ‘Health literacy,’ ‘patient safety,’ and ‘primary care’ in the PubMed, Cochrane Systematic Reviews, and the Joanna Briggs Institute (JBI) Evidence Synthesis databases; no systematic, integrative, narrative, or scoping reviews covering the theme were found.
In this setting, the following research question was raised, based on the PCC strategy (population, concept, and context), which will be addressed below: How can health literacy contribute to the safety of PHC patients? Based on this, the review aimed to map the evidence regarding the impact of health literacy on care safety for adult PHC patients.
Materials and Methods
The present study was done following the JBI methodology for scoping reviews (23). The protocol was prospectively registered in the Open Science Framework (https://osf.io/8xjb9/?view_only=8d67d5618bf34fffa013d7f407a9cbfb ).
This scoping review covered experimental and quasi-experimental study designs, including randomized clinical trials, non-randomized controlled trials, before-and-after studies, and interrupted time series studies. Analytical observational studies, including prospective and retrospective cohort studies, case-control studies, and analytical cross-sectional studies were also covered. Descriptive observational studies, including case series, individual case reports, and descriptive cross-sectional studies were included. Qualitative studies focused on qualitative data were covered, including but not limited to projects such as phenomenology, grounded theory, ethnography, qualitative description, action research, and feminist research. In addition, texts and opinion pieces, as well as systematic reviews that met the inclusion criteria were also included, depending on the research question.
The search for articles was based on the descriptors indexed in the Medical Subject Headings (MeSH)/Descriptors in Health Sciences (DeCS): ‘Health literacy,’ ‘primary health care,’ ‘patient safety,’ and ‘risk management,’ using the Boolean operators AND and OR (Table 1).
Table 1 Descriptors and Keywords Used. Brasília, Distrito Federal, Brazil, 2023
| PCC | MeSH | Keywords | |
| Population | Primary health care | ||
| AND | |||
| Concept | Health literacy | OR | Information literacy |
| AND | |||
| Context | Patient safety | OR | Safety management |
Source: Research data.
Search Strategy
The search strategy aimed to find published and unpublished studies and was performed in three steps. The first search, which was done in December 2022, consisted of an initial search in the electronic databases Medline (PubMed) and Virtual Health Library. Next, the words contained in the title, abstract, and keywords of the articles found were analyzed. The descriptors were compared to those registered in MeSH for searches in PubMed, while DeCS was used for searches in the Virtual Health Library (VHL).
In the second step, which was done in February 2023, the search strategy, including all the keywords and indexing terms identified, was adapted for each database and/or information source included. The search strategy was tested by two reviewers. The following databases were included: Medline (PubMed), Web of Science, Scientific Electronic Library Online (SciELO), VHL, Scopus, Cinahl, and Google Scholar in the gray literature (Table 2). The reference list of all the evidence sources included was examined for additional studies in April 2023. The third stage was done between March and May 2023, with the extraction and analysis of data from all the selected studies.
Table 2 Search Strategy. Brasília, Distrito Federal, Brazil, 2023
| Database | Strategy |
| PubMed | ((((“health literacy” [MeSH Terms] OR “health literacy” [All Fields]) AND “Primary Health Care”[MeSH Terms]) OR “Primary Health Care” [All Fields]) AND “Patient Safety”[All Fields]) OR “Risk Management” [MeSH Terms] |
| Web of Science | (“health literacy” OR “Information Literacy”) AND “Primary Health Care” AND (“Patient Safety” OR “Risk Management”) |
| SciELO | (“health literacy” OR “Information Literacy”) AND “Primary Health Care” AND (“Patient Safety” OR “Risk Management”) |
| VHL | “Letramento em saúde” AND “Atenção primária à saúde” AND (“Segurança do paciente” OR “Gestão da Segurança”) |
| Scopus | (“health literacy” OR “Information Literacy”) AND “Primary Health Care” AND (“Patient Safety” OR “Risk Management”) |
| Cinahl | (“health literacy” OR “Information Literacy”) AND “Primary Health Care” AND (“Patient Safety” OR “Risk Management”) |
| Google Scholar | “Letramento em saúde” AND “Atenção primária à saúde” AND (“Segurança do paciente” OR “Gestão da Segurança”) |
Source: Research data.
Inclusion Criteria
The PCC strategy was used to draw up the research question in which: Population refers to studies where the participants were users of PHC services, in this case, adults who received health care (excluding studies where participants received home care); concept refers to studies that addressed care, techniques, protocols, or health literacy methods used to improve health care; context refers to studies on patient safety, patient engagement and/or self-management in PHC. Patient safety entails not subjecting the user to avoidable risks resulting from the care or assistance provided, as well as preventing any complications (7). Thus, all studies that addressed this context along with the concept and participants described above were included in the search.
Original studies available in full, classified in line with the JBI Sumari and their methodological potential, as well as gray literature, were also included. The studies included had been published until February 2023, in all languages, and covered the review theme. Publications on websites, editorials, and book chapters were excluded.
Study Selection and Evidence Source
After the search, all the identified citations were grouped and uploaded to the Mendeley V.1.19.4 bibliographic software and duplicates were removed. After a pilot test, the titles and abstracts were then screened by three independent reviewers to assess the inclusion criteria for the review. Potentially relevant sources were retrieved in full and their citation details were imported into the JBI System for unified information management, evaluation, and review (JBI Sumari [24]).
The full text of the selected citations was assessed in detail according to the inclusion criteria by three independent reviewers. The reasons for excluding evidence sources in the full text that did not meet the inclusion criteria were recorded and reported. Any disagreements that emerged between the reviewers at each step of the selection process were settled through discussion or by consulting one or more additional reviewers. The results of the search and study inclusion process were reported in full in the final scoping review and were presented in a flow diagram (Figure 1) of Preferred Reporting Items for Systematic Reviews and Meta-Analyses extension for Scoping Reviews (PRISMA-ScR [25]).
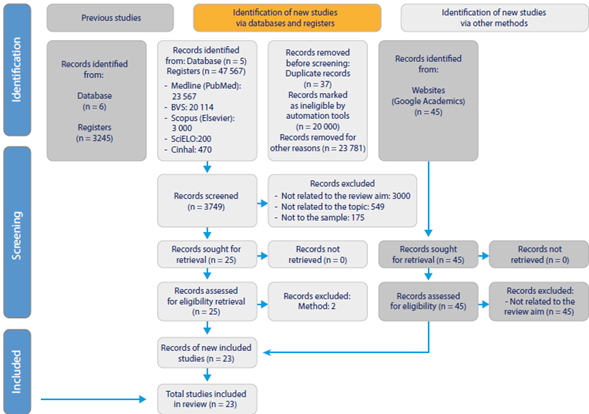
Source: Based on (25).
Figure 1 Flowchart for the Search and Selection Process of Studies for the Scoping Review
Data Extraction
Both reviewers used the JBI Sumari tool to extract the data from the studies included in this review. After this step, the data were presented in a table with the following information: Article title, publication year, country, study objective, population/sample, study design, main conclusions, findings related to the question of this scoping review, and levels of evidence. To classify the level of evidence of the materials selected in this review, the guidelines of Melnyk and Fineout-Overholt (26) were used (Table 3). Disagreements between the reviewers, when found, were settled by a third reviewer.
Table 3 Evidence Levels Classification
| Level of evidence | Classification |
| Level I | Evidence from a systematic review or meta-analysis |
| Level II | Evidence obtained through well-designed rigorous research |
| Level III | Evidence from well-designed controlled trials without randomization |
| Level IV | Evidence from well-designed case-control and cohort studies |
| Level V | Evidence from systematic reviews of qualitative and descriptive studies |
| Level VI | Evidence from single descriptive or qualitative studies |
| Level VII | Evidence from the opinion of authorities and/or specialist committee reports |
Source: Adapted from (26).
Results
Study Inclusion
Of the 23 studies selected, 6 were published in 2020; 3 were published in 2022; followed by 4 studies in 2016; 3 studies in 2014 and 2017; 2 studies in 2022; and only 1 study was published in each of the following years: 2013, 2015, 2018, 2019, and 2021 (Figure 2).
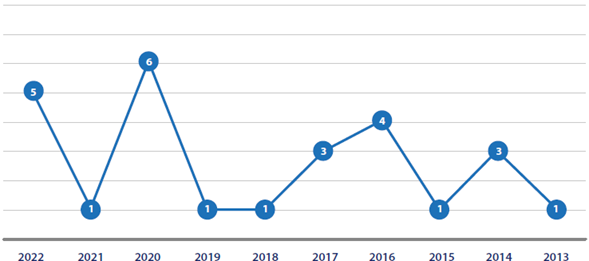
Source: Research data.
Figure 2 Distribution of Publication Periods by Year (N = 23). Brasília, Distrito Federal, 2023
Regarding the country where the studies were conducted, most of them (11) were done in the United States; 3 studies in the United Kingdom; 2 studies in Germany, Japan and Australia; and only 1 study in Sweden, Spain, and China (Figure 3).
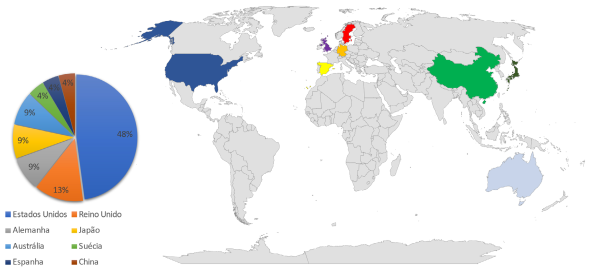
Source: Research data.
Figure 3 Distribution of Publications by Country (N = 23). Brasília, Distrito Federal, 2023
The data extracted from the articles is shown in Table 4 for a better overview of the information related to the objectives and questions posed by the present study.
Table 4 Data Extraction. Brasília, Distrito Federal, 2023
| Title | Year/ level of evidence | Country | Study objective | Study design | Main findings/contributions of health literacy to patient safety |
|---|---|---|---|---|---|
| Quality and availability of information in primary healthcare: The patient perspective(27) | 2020/VI | Sweden | To explore the life experiences of patients communicating with and receiving information from PHC. | Qualitative study | The findings would increase patient safety, financial efhciency, and free resources for PHC: Concerns regarding quality and attention to the continuity of follow-up with another health care professional; security regarding the content of the information received; easy access to PHC and health care professionals; and the introduction of strategies using health literacy. It should be emphasized that health literacy favors patient involvement and continuity of care with PHC professionals, resulting in improved care safety. |
| The impact of health literacy on desire for participation in healthcare, medical visit communication, and patient reported outcomes among patients with hypertension(28) | 2013/II | The United States | To clarify how health literacy influences patients’ interest in participating in health care, communication of medical appointments, and patient-reported outcomes of appointments. | Cross-sectional study | In this specific population -hypertensive patients- both the patients with low and adequate health literacy expressed a similar desire to participate in medical decision-making; the patients with low literacy asked their medical doctors fewer questions about medical issues (due to fear of being judged as having a limited ability to understand information). The real challenge a low level of health literacy poses is not being able to have a clear and meaningful conversation about treatment options and alternatives. Thus, by providing strategies that facilitate health literacy, patient safety will be promoted. |
| The impact of health literacy, patient centered communication and shared decision- making on patients’ satisfaction with care received in German primary care practices(29) | 2016 / VI | Germany | To explore the extent to which subjective health literacy skills and the perceived application of patient-centered communication and shared decision-making are associated with patient satisfaction with the care provided by their general practitioner. | Cross-sectional survey | The role of management regarding leadership and continuous education of health care professionals is key to improving the safety of the care provided. The importance of implementing interventions to initiate the transformation process towards literate health care in the organization. Not only implementing certain interventions but also considering measures to change the organizational culture toward a more patient-centered understanding of care. |
| Association between health literacy and patient experience of primary care attributes: A cross- sectional study in Japan -(30) | 2017/VI | Japan | To examine the association between health literacy and patient experience of primary care attributes. | Cross-sectional study | The study population may have influenced the result since the basic literacy rate is estimated to be 99 %. The importance of health literacy for effective communication between patients and doctors has increased care safety. Patients with low health literacy may be likely to not understand or remember the content of the health education offered in PHC. Health literacy was positively associated with the patient’s experience of PHC. |
| Relationship between Teach-back and patient-centered communication in primary care pediatric encounters(31) | 2017/VI | The United States | To propose and test a theoretical framework on how the use of teach- back can influence communication during clinical appointments. | Cross-sectional study | Teach-back has increased the prospects for patient- centered communication. Involving parents in clinical training can help promote technique and ensure safe care. |
| Expanding the universal medication schedule: A patient- centred approach(32) | 2014/VI | The United States | To promote patient understanding, adherence, and safety by improving medication labels. | Cross-sectional study | A need to consider approaches other than medication labels to promote the safe use of prescription medication. Increased counseling and education, use of plain words and explicit instructions, increased contact with medical doctors and pharmacists. Patient-centered care combined with health literacy promotes patient safety. |
| Survivorship care plan information needs: Perspectives of safety-net breast cancer patients(33) | 2016/VI | The United States | To identify the information needs and survival care plan preferences of low literacy and multilingual patients to support the transition from oncology to primary care and continuous learning in survival. | Focus groups | A study directed towards groups of patients with a low level of health literacy, in the context of care transitions, regarding survival information needs among breast cancer patients to increase their safety. Women turned to peer support and community organizations in the absence of information from providers. There is lower interest in a treatment summary and higher interest in information and education about what to do and post-treatment management. By promoting health literacy, feelings of concern over the disease are reduced, favoring the quality of safe care. |
| Health literacy of patients on oral anticoagulation treatment- individual and social determinants and effect on health and treatment outcomes(34) | 2021/VI | Spain | To evaluate the relationship between health literacy and health and treatment outcomes (compliance with oral anticoagulants, management of normalized ratio and occurrence of complications) in patients with cardiovascular pathologies. | Observational, analytical, and cross-sectional study. | Health literacy has a relevant influence on the adequate self-management of anticoagulant treatment and the frequency of complications, but the ‘social health support’ dimension is essential for optimal self-management. The study showed a significant association between scores in all dimensions of health literacy, with patients with higher scores experiencing fewer complications, fewer emergency room admissions, and lower hospitalization rates. |
| Implementing routine health literacy assessment in hospital and primary care patients(35) | 2014/VI | The United States | To establish a standardized approach for assessing and reporting health literacy in inpatient and outpatient practice at a large academic medical center. | Cross-sectional study | This initiative entailed changing the existing practices of the nursing team; discussions with nurses in hospital and clinical settings provided valuable insights into the barriers and facilitators to implementing a health literacy screening tool, even in settings with varying patient populations. Incorporating health literacy assessment into patient screening will not only facilitate large-scale research on the effect of low health literacy on patient safety processes and outcomes but will also enable the targeted development and dissemination of patient education resources that address the needs of adults with low health literacy. |
| The safety of health care for ethnic minority patients: A systematic review(36) | 2020/I | Australia | To establish how ethnic minority populations are conceptualized in the international literature and the implications of this in framing our findings; the evidence of patient safety events emerging among ethnic minority health care users internationally; and the individual, service and system factors that contribute to unsafe care. | Systematic review | The studies showed that ethnic minorities experienced higher incidence rates of health care associated with infections and dosage errors. It was found that reduced interaction between ethnic minority patients with health care professionals and systems, with a focus on prejudice, and a lack of communication and level of understanding, which entails health literacy, can result in unsafe care. |
| A cluster- randomized study on the Risk Assessment and Management Program for home blood pressure monitoring in an older population with inadequate health literacy(37) | 2020/II | China | To compare the blood pressure control rate of participants after group assessment and risk management care, with participants in standard care. | Randomized controlled prospective study | The study results showed a significant increase in blood pressure control after the intervention, especially in patients with limited health literacy, with the target group becoming more engaged and adherent to treatment, thus reflecting on patient safety. |
| Improving health literacy knowledge, behaviors, and confidence with interactive training(38) | 2022/VI | The United States | To describe the development, implementation, and evaluation of an interactive health literacy intervention in primary care clinics. | Pre- and post-training descriptive design | 70 % of the team post-training, and 82 % of the survey participants one year post-training stated they were able to clarify and correct misunderstandings within the primary care setting. Most misunderstandings that had been corrected included medication, including doses, frequencies, refills, and issues related to inhaler use and immunization, reducing the risk of adverse events and increasing patient safety. Clinical teams can improve the way they provide information and health education to patients and their families; multidisciplinary learning sessions were an opportunity to learn more about each other’s interactions, regardless of role. Educating health care professionals is a necessary step in promoting safety. |
| Engaging women with limited health literacy in mammography decision-making: Perspectives of patients and primary care providers(39) | 2020/VI | The United States | To identify opportunities to meet the needs of both parties involved in the development of interventions to improve decision- making regarding mammography among women with limited literacy. | Qualitative study | A team-based approach can be a practical solution that supports information sharing by a lay health educator and targeted decision-making with health care professionals. Strategies that can support patients with limited health literacy to better engage in discussions regarding mammography are highlighted, including refraining from assuming that mammography is common knowledge and sharing the process-focused information about breast cancer screening desired by patients. |
| Improving health literacy in a Japanese community population: A pilot study to develop an educational programme(40) | 2018/VI | Japan | To evaluate a program designed to improve health literacy in a certain population, aiming to go beyond functional health literacy. | Mixed method | During the program, participants have acquired not only knowledge and skills but also experienced a change in their beliefs and behaviors. The development of individuals who are more motivated to learn about health systems, who collaborate with the professional team, maintain and promote their health and that of the people around them which contributes to the engagement and awareness of individuals about their role in ensuring safe care. |
| Understanding quality use of medicines in refugee communities in Australian primary care: A qualitative study(41) | 2016/VI | Australia | To explore the barriers and facilitators to the use of quality medication experienced by refugees, pharmacists, general practitioners, and nurses working in PHC. | Qualitative study | A multifaceted approach including patients, communities, and health care professionals is ideal. The evaluation of strategies along with community involvement is essential to move forward and perform a more systemic approach toward patient safety. |
| Empowering people to help speak up about safety in primary care: Using codesign to involve patients and professionals in developing new interventions for patients with multimorbidity(42) | 2017/VI | The United Kingdom | To explore production methodologies, which may improve intervention development and provide a mechanism for translating the available evidence into patient intervention proposals centered on multimorbidity and safety. | Two participatory design methods | The scenario proved useful in everyone’s understanding, from different points of view. Safety in terms not only of avoiding errors but also of the need for more holistic care geared towards the patient’s needs. Better communication and sensitivity between patients and professionals. |
| Test result communication in primary care: Clinical and office staff perspectives(43) | 2014/VI | The United Kingdom | To understand how laboratory test results are conveyed to patients in primary care and the insights into how this process can be improved. | Qualitative study | The study shows that making patients aware of their responsibility for checking test results can help reduce possible errors. To help reduce error potential. |
| Assessing health literacy in safety net primary care practices(44) | 2016/VI | The United States | To address patients’ health literacy deficits within primary care settings through the use of the Newest Vital Sign. | Cross-sectional exploratory study | The long-term benefits of addressing health literacy: Improving patient follow-up related to prescribed treatment plans, increasing their understanding of health promotion messages, increasing timely follow-up appointments, and improving the quality of care and healthier long-term outcomes. |
| Assessing mobile phone digital literacy and engagement in user-centered design in a diverse, safety-net population: Mixed methods study(45) | 2019/VI | The United States | To describe the variations in patient involvement in the app design process, with a focus on limited health literacy, limited English proficiency, and limited digital literacy. | Cross-sectional study | The need for a better understanding of how to consider, define, and incorporate digital literacy when implementing the use of health technologies, along with continued efforts to better include vulnerable populations in research. |
| The evidence‐based development of an intervention to improve clinical health literacy practice(46) | 2020.VI | The United Kingdom | To improve the awareness, skills, and practice of health literacy to improve patient experience. | Intervention | Health care professionals play a key role in building the health literacy responsiveness of health care systems to ensure that they meet the health literacy needs of the population. The approach to the development of the intervention adopted in this project resulted in an intervention that was improved through feedback from the medical doctors who performed the training and from a group of patients and caregivers. |
| An electronic medication module to improve health literacy in patients with type 2 Diabetes Mellitus: randomized controlled pilot study(47) | 2020/II | Germany | To evaluate the influence of a medication module within an electronic patient-led health record on improving health literacy. | Exploratory, prospective, randomized, and controlled study | Having access to the electronic medication platform seemed to influence some aspects of health literacy and patient safety in medication management. |
| Electronic health literacy among linguistically diverse patients in the Los Angeles county safety net health system(48) | 2022/VI | The United States | To describe patterns of technology access and use, in addition to levels of health literacy among English-speaking and patients with limited English proficiency in a Los Angeles safety-net health care system. | Exploratory study | Not only access to technology must be considered, but also the design and perceived usability of telehealth and the individual health literacy of patients, so that they can use the technology as a tool to ensure safe care. |
| Health literacy: An educationally sensitive patient outcome(49) | 2015/VI | The United States | To discuss how health literacy, defined as “the extent to which individuals have the ability to obtain, process, and understand basic health information and services needed to make adequate health-related decisions” (49:1363), is an educationally sensitive patient outcome. | Conceptual study | Medical doctors’ health literacy leads to better patient outcomes through the use of strategies by the health care provider to assess the patient in their own self-care and ensure adequate health literacy and safety of the measures being implemented on the patient. |
Source: Prepared by the authors.
Discussion
To discuss the evidence found in this review, the following categories were delimited: ‘The impact of health literacy on patient safety in PHC;’ ‘Interventions that contribute to health literacy in PHC,’ and ‘The assessment of users’ and professionals’ perspectives on health literacy.’
The Impact of Health Literacy on Patient Safety in PHC
The framework used to design health literacy interventions targets learning stimulation and motivation, recognizing that patient involvement in the learning process is likely to be a key contributing factor to their ability to understand and act on health-related recommendations (49). For this purpose, it is necessary to develop strategies that meet their preferences and needs effectively, in balance with the provider’s knowledge, skills, and structural constraints (39).
Health literacy can be a key factor in the self-management of care, as shown in a study that assessed adherence to the use of oral anticoagulants in patients with cardiovascular diseases. Patients with higher levels of health literacy reported being confident in their ability to manage information, empowerment, and self-efficacy. In addition, they had better self-care, treatment management, excellent appointment attendance, and fewer complications, room admissions and hospitalizations (34). A cluster-randomized controlled study aiming to carry out high-quality blood pressure monitoring at home found that interactive group education and subsequent individual counseling can reduce the rate of patients with uncontrolled hypertension compared to conventional individual counseling. Positive effects were found in patients with both adequate and inadequate health literacy (37).
Patient-centered care that respects individual preferences and needs is attainable when health care organizations strengthen interpersonal relationships and shift away from disease-oriented care, trying to produce the best outcome for the patient (29). Some aspects that should be considered in decision-making are information provision / patient education (focused on benefits and risks), clear medical doctor-patient communication and structure for decision-making (39).
A randomized controlled trial (28), using data registered in the Patient-Physician Partnership, evaluated the effectiveness of intensive interventions directed to patients and medical doctors to improve adherence among hypertensive patients. There were no significant differences in the desire of users with low and adequate literacy levels to become engaged with their health care. However, users with a lower level of health literacy asked fewer questions, while still asking those of a psychosocial nature, and experienced less shared decision-making, whereby the medical decision was imposed (28).
In this context, health literacy saw a significant improvement following the educational intervention. Valuing the patient’s role based on their own knowledge led to a change in the beliefs and behaviors of health care service users who became active participants in the system. Investing in the motivation of individuals to learn about health care systems and to collaborate with their health care providers with the necessary knowledge and skills can enable them to maintain and promote their own health and that of their families and loved ones (40).
Communication is among the international goals for patient safety, since it is vital for individuals living in society, especially in the health and illness process (30). Patients with limited health literacy tend to not understand or remember the content of the health education offered by their primary care provider (30). Another study (38) found that parents with poor health literacy experience worse outcomes and care deficits in terms of their children’s health. Poor communication compromises safety and leads to patient and family dissatisfaction with health care (38).
It is worth understanding that patients seek different types of information beyond technical aspects; they also consider the recommendations, the step-by-step process, and knowing what should be expected from a process involving their health. Due to the time constraints of appointments, professionals and patients find it beneficial to offer tools and professionals who can reiterate the educational content, summarize what health decisions have been made, and support the continued retention of information in environments outside the doctor’s office (39).
Health literacy can be improved by providing information, effective communication, and structured education, in which health care professionals can personalize and target care according to the user’s profile (40). The various cultures, traditions and the context in which they live must be considered for adapting the most suitable strategy to be used (41). A study carried out with refugees in Australia mentions the importance of an interface with facilitators who can help them make decisions (41). A multifaceted approach involving patients, communities, and health care professionals is ideal.
Interventions that contribute to health literacy in PHC
Health literacy strategies can be taught, and skill learning can be measured (49). Health care professionals, regardless of their category, have a key role to play in the development of health systems’ capacity to address health literacy to ensure that they meet users’ literacy needs (38, 46). However, a large number of health care professionals are unaware of alternative strategies that can improve and facilitate communication with users. In this sense, it is essential that health care professionals who provide direct care to patients know the principles of health literacy and how to implement them in practice, as this is a necessary step to promote safety and improve care in all contexts, including primary care (38).
The lack of information continuity and transfer between patients and several different health care professionals has been identified as a source of uncertainty and vulnerability among primary care users in Switzerland (27). Interactive professional-centered interventions were associated with improved knowledge, behaviors, and confidence among team members regarding the use of health literacy strategies. This type of study can lead to better outcomes, such as the prevention of misunderstandings related to medication, immunization, and preventive care (49).
In one study, a pop-up notification was implemented in the electronic medical record system so that medical doctors and nurses, when providing care to a patient at risk of low health literacy, could apply the health literacy knowledge learned during the educational intervention (46). Pictogram-based medication instruction sheets, written at a lower level of health literacy, along with demonstration, teach-back/ show-back and the availability of dosing tools can complement these professionals’ verbal advice and reduce dosing errors (49).
Three studies (45-47) used digital resources as their intervention, one of which highlighted that the level of user engagement can vary according to health literacy, spoken language proficiency, and digital literacy. A better understanding of how to consider, define, and incorporate digital literacy when developing health-related information technology is needed, as well as continued efforts to better engage vulnerable populations in research. Ownership of a smartphone, even with daily personal use, does not accurately predict comfort or ability to use basic phone features such as text messaging (45).
It is important to ensure that an intervention is effective, efficient, and sustainable (38). Adequately monitoring the quality of a study and the various stages of a complex intervention, along with meticulous planning of a pilot study that tests unrecognized variability sources, is a must before implementing essential intervention studies (47). Two interventions targeting digital health literacy did not produce a statistically significant effect (45, 47), presenting various limitations and problems in their implementation, such as difficulty in understanding the proposal by the target population; inadequacy and inefficiency of the technique applied; low engagement (45); short implementation period of the intervention; no access to the proposed digital tool; and a high drop-out rate among study participants (47).
The effectiveness of interventions can be maximized when they are in line with and based on the best and most recent scientific evidence and through feedback from the target population (46). The creation of realistic practical scenarios relating to the primary care environment also leads to an increased possibility that participants will recognize how the principles of health literacy can be applied (38). Although a shorter training period may be more attractive to busy professionals, a full day of health literacy training may be necessary to address all the relevant issues of the educational intervention, which corroborates the literature findings on the subject (46).
Other factors that increase the effectiveness of the educational intervention entail multi-component training with small group work and role-playing; identifying barriers to changes and devising plans to overcome them; and involving a local opinion leader and/or team representative in the training (46).
The Assessment of Users’ and Professionals’ Perspectives on Health Literacy
Health literacy is a predictor of individual health status and enables the identification of people in vulnerable situations and the effective management of health inequalities. A study (34) has shown a strong relationship between the dimensions of health literacy and the social determinants that comprise the axes of health inequality (34).
In PHC, patient safety goes beyond technical measures and includes the relational context of care, which is responsive to the patient’s priorities and must be agreed upon between health care professionals and patients. Different needs must be addressed and active communication with patients is recommended to avoid making assumptions about their capacity and priorities. Participatory design studies seem to be useful for understanding not only how a recommendation should be perceived, but also how it should feel in practice (42).
In a qualitative study, semi-structured interviews were conducted with refugee health care leaders, pharmacists, nurses, and general practitioners to explore the barriers and facilitators to quality medication use experienced in the PHC setting in Australia. Five barriers were found: communication, language restriction, cultural issues, limited health literacy, and financial costs. Communication barriers were the most common and impacted quality access to medication, which highlighted the vital role of interpreters and training for health care professionals in providing cross-cultural care. Collaboration between health care professionals can improve the safe use of medication and users can benefit from a medication review carried out by a pharmacist. Low health literacy in a person’s mother tongue can limit the effectiveness of translated resources, although written information is useful. In addition, pictograms designed to support medication instructions for consumers with low health literacy can be misinterpreted, especially in cross-cultural contexts (41).
Most users are willing to trust the health care system and its professionals, but a lack of communication and continuity of care is an obstacle. PHC users in Switzerland rated the language skills of health care professionals as poor, hindering the establishment of a bond. The stress caused by the reduction of the minimum time spent in each appointment resulted in feelings of incomprehension and aversion by patients towards health care professionals. Furthermore, the lack of information continuity and transfer between patients and several different health care professionals has been identified as a source of uncertainty and vulnerability (27).
The perception of systemic inertia inherent to PHC has a negative influence on user satisfaction, which impacts aspects such as monitoring and receiving test results (27). According to an American study that assessed the communication of test results, the responsibility for communicating test results is not clear among health care professionals; communication does not follow standards or protocols and normal results are not commonly reported. The communication of abnormal results by non-health care professionals, as they have no knowledge of how to clarify doubts, leads to anxiety among patients (43).
Effectiveness in communication is needed at several stages of the health and illness process, as shown in a study assessing breast cancer patients’ perspectives on information regarding their care and survival plan. According to a study (33), a written document with a survival plan is no replacement for direct communication with professionals about treatment, symptom management and transition, which was assessed as a failure by the participants. In the absence of information, patients turned to peer support and community organizations. Data suggests that patients are less interested in a treatment summary and more interested in information and education regarding what to do and how to manage survival. Some women report the need for better communication related to side effects, pain, healthy eating, and reconstructions. This lack of information leads to concern, fear, and anxiety in patients (33).
Health literacy is part of the complexity inherent to health care services, which must provide tools to improve written, oral, and documental communication to improve patient-centered care. A study (35) evaluated the level of health literacy of patients at a medical center in the United States through an initial screening and the information included in the patient’s record, based on a model of improvement in which health care professionals participated in the training. The participating nurses adopted the new process quickly and reported it as beneficial for patient education discussions. A key facilitator for the adoption and acceptability of the instrument being evaluated was the support of the leadership and the integration of all stages of the project into the existing infrastructure and workflows. The initiative promoted change in the nursing team’s practice and provided important information regarding barriers and facilitators to health literacy. The evaluation of health literacy enabled the team to increase their awareness of low health literacy among the patients they treated, which allowed them to develop adequate resources, carry out large-scale research into the consequences of low health literacy, and evaluate the effect of the system’s interventions according to patients’ level of health literacy (35).
Implementing the assessment of users’ level of health literacy and training health care professionals to use it routinely can improve the quality of care and promote healthier long-term outcomes. An exploratory cross-sectional study evaluated the perceptions and perspectives of patients and professionals regarding the use of the Newest Vital Sign health literacy assessment tool. It showed that health care professionals, especially medical doctors, are unaware of the tools needed to assess patients’ literacy. At the study’s conclusion, the routine application of the Newest Vital Sign tool was recommended during the user’s admission appointment, since it covers the various dimensions of health literacy, is quick (3-5 minutes) and easy to apply by professionals and acceptable to users (44).
A study assessed patients’ perceptions of the Universal Medication Schedule to expand it. According to the participants, clear and concise words and sentences should be used whenever possible; in addition, there was a greater acceptance of the term ‘half’ instead of the fraction ‘½’. Improving prescriptions is not enough to promote safe and consistent medication use, and additional support for patients is needed. Participants suggested that dosage instruments should be made available, since measurements can vary and are not well known. They also asked for the maximum dosage of painkillers to be specified and for the use of medication to be linked to specific times (32).
Conclusions
The contributions of health literacy are vast since patients and professionals become partners and get involved in the search for safe, quality care, where the focus is placed on patients and their individual needs. The impact may not be noticeable immediately, as the established safety culture requires time to change, but this process of reflection and change must be initiated. Communication is the keyword, but it also presents a daily challenge within the context of health care teams. Engaging patients and their families with strategies that enable a comprehensive assessment of health conditions and consider individual variations in each context is essential in terms of primary health care. Creative and more visual strategies facilitate understanding and improve acceptance of what is new. Synthesizing the results can contribute to decision-making and guiding care practices, leading to increased safety for both patients and the professional teams in PHC.
The impact of using strategies based on health literacy assists communication, patient engagement in their care and, consequently, the safety of care in PHC. Health care based on evidence-based pillars that ensure patient safety emphasizes the need for health-literate patients who understand their role in the health-disease process, focusing on health promotion and prevention, which are the foundations of PHC care.











 text in
text in 



