Introduction
Facing the COVID-19 Pandemic, many uncertainties have arisen regarding the transmission of the pathogen, its complications, and the choice of management strategies, due to inconsistent scientific knowledge, rapid spread, and a high mortality rate, especially in vulnerable populations (1).
To reduce transmissibility, governments and health organizations have announced preventive measures to protect hospital beds. Hand hygiene, the use of face masks, the adoption of respiratory etiquette, and progressive social distancing and isolation measures1 were strongly encouraged during this period (2).
Another strategy encouraged was selective distancing, which involves isolating groups that are more likely to develop or have complications from the disease. This category includes people aged ≥ 60, people who are obese, people with chronic non-communicable diseases, and high-risk pregnant women (3). Of this group, the elderly develop more severe cases, which was considered an indication that associated morbidities such as coronary heart disease, diabetes mellitus, and hypertension would increase mortality and the occurrence of hospitalizations (4).
Although the elderly population has particularities that may affect disease progression, such as the presence of multimorbidity, physical frailty, and inflammatory and immunological alterations, the use of age as a central parameter for the adoption of selective social distancing for the elderly is debated. In this sense, other measures were considered, such as assessing the state of physical frailty instead of chronological age, which favored the prognosis of the elderly during the COVID-19 pandemic (5, 6).
Searching for a relationship between COVID-19 infection and frailty, a study conducted in England (7) with 383,845 participants aged between 37 and 73 observed a greater worsening of COVID-19 in pre-frail (risk ratio [RR] 1.47; 95 % confidence interval [CI] 1.26-1.71) and frail elderly (RR 2.66; 95 % CI 2.04-3.47).
Frailty is a transition from homeostasis to critical dysfunction of multiple biological and physiological systems. Due to its complexity and dynamic nature, this condition requires interventions that have a multi-systemic effect, such as physical activity (8). The frailty phenotype consists of five components: Unintentional weight loss, self-reported fatigue/exhaustion, decreased physical activity, decreased frail, those with one or two are considered pre-frail, and those with none are considered non-frail (9).
Decreased physical activity is one of the markers that comprise the frailty phenotype(8), for which there is no effective pharmacological treatment, with physical exercise as the therapeutic plan. Prevention and treatment of physical frailty and related conditions, such as muscle inflammation with loss of mass and strength, can be achieved through physical activity (10). Physical activity is defined as “any bodily movement produced by the skeletal muscles that requires energy expenditure” (11:15).
A prospective longitudinal study in Malaysia (12) of 2,324 people aged ≥ 60 analyzed the factors associated with the distinct stages of frailty transition. It was found that low levels of physical activity increased the likelihood of worsening transition to states of higher frailty (odds ratio [OR] 2.9; 95% CI, 2.2-3.7) and decreased the likelihood of transition to states of lower frailty (OR 0.3; 95% CI, 0.2-0.4; p < 0.05). Therefore, reducing opportunities for group or individual physical activity in gyms and outdoor environments during the pandemic may alter the state of physical frailty.
A survey of 937 non-frail elderly people in eight cities in Japan investigated the influence of the COVID-19 pandemic on physical activity in non-frail elderly people. It was observed the total time spent in physical activity by the elderly during the three waves of the pandemic decreased by 33.3%, 28.3%, and 40%, respectively, compared to the pre-pandemic period (13).
The association between reduced physical activity and social isolation has been described in the literature (14). However, the relationship between the degree and grade of adherence to protective measures among older adults during the COVID-19 pandemic, and how the effects of physical activity frailty present themselves as significant knowledge gap. In view of this, it is important to evaluate the effects of the protective measures of social distancing and isolation on frailty in the elderly and on the physical activities they perform. Thus, this study aimed to analyze the effects of social distancing and isolation caused by the COVID-19 pandemic on frailty in the elderly and on their physical activities in primary health care in a Basic Health Unit (BHU) in Brazil.
Materials and Methods
Type or Design of the Study
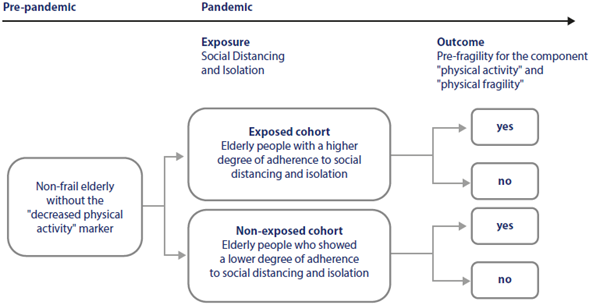
A prospective cohort study was developed from the establishment of a cohort of elderly people without the variables of interest (reduced physical activity and physical frailty) in the pre-pandemic period. The elderly were allocated into cohorts according to the degree of exposure to social distancing and isolation during the pandemic and were observed for their level of physical activity and transition to frailty (15).
Location
The first wave of data collection took place in a UBS in a capital city in southern Brazil, which had already been the subject of studies on physical activity and the frailty phenotype by the research group to which the authors belong, and the second wave in households in the same city. The region where the BHU is located has a population of 205,248 inhabitants, with growth in the older age groups in recent years, as evidenced by the trend toward a proportional decrease in children and young people and the aging of the population (15).
The research group collected data from the first wave before the COVID-19 pandemic was declared by the World Health Organization on January 30, 2020, in a UBS where patients were already the subject of a study on physical activity and frailty phenotype. With the state of emergency declaration, the authors prepared the matrix project entitled “Effects of social distancing and isolation generated by the COVID-19 pandemic on the condition of physical frailty, depressive symptoms, level of physical activity and nutritional status in elderly people in Primary Health Care,” of which the present study is one of the subprojects (15).
Population, Eligibility Criteria, Collection Period and Sample
The target population included elderly people aged ≥ 60 with a definitive active registration with the analyzed BHU. For the first wave of the study, before the pandemic, participants were selected from a sample of 389 older people who were not considered frail and did not have the marker “decreased physical activity” (n = 168). The study cohorts were organized during the second survey wave according to the degree of social distance and isolation (exposure) and observed for the occurrence of the variables of interest, decreased physical activity and/or physical frailty (outcomes [15]).
The inclusion criteria for the cohorts were age ≥ 60; definitive registration at the BHU; cognitive ability, screened by the Mini-Mental State Examination (MMSE)[16]), taking into account the level of schooling according to the cut-off points that consider illiteracy; low schooling (1 to 4 years of incomplete schooling); medium schooling (4 to 8 years of incomplete schooling); high schooling (8 or more years [17]) to answer the questions; not being frail elderly; not having the marker “decreased physical activity”; medium schooling (4 to 8 incomplete years); high schooling (8 or more years [17]) to answer the questions; being a non-frail elderly person; not presenting the marker “decreased physical activity” in the first wave of assessment and having taken part in both waves of data collection.
The exclusion criteria were being a wheelchair user, having lower or upper limb amputations and living outside the region covered by the UBS. The discontinuation criteria were death; moving out of the region covered by the UBS; hospitalization during the collection period; registration address not found and refusal to participate in the second wave of evaluation. Of the 168 non-frail elderly people who took part in the first assessment wave in 2019, 6 died, 29 moved house or were disconnected from the BHU, 2 were hospitalized, 31 refused to take part in the survey and 1 was not found at home, making a total of 100 elderly people assessed in the second wave.
The second collection took place during the pandemic period, from July to August 2021. The instrument used included data from the first wave, as well as the Degree of Adherence to Social Distancing and Isolation Scale. The average follow-up time was 762 } 102 days (469 and 954 [15]).
Study Variables and Data Collection Instruments
The level of physical activity and the state of physical frailty were the dependent variables of interest. Sociodemographic, clinical, and degree of social isolation and alienation were used as independent variables.
The elderly were given a structured questionnaire. It included identity, sociodemographic, and clinical questions. Frailty was classified using the following markers of the physical frailty phenotype: reduced handgrip strength; reduced gait speed; self-reported fatigue/exhaustion; unintentional weight loss and reduced level of physical activity (9). The level of physical activity was measured by energy expenditure using the Minnesota Leisure Time Activities instrument, validated for Brazilian Portuguese (18).
To assess the degree of adherence to social distancing and isolation, a Likert-type scale was organized, which assigns numbers correlated with the statement (19). After explaining the concepts of social distancing and isolation, the elderly were asked to recall the period from March to December 2020, the period before the COVID-19 vaccines were administered. The questions used were as follows: Did you practice social distancing? Have you practiced social isolation? Have you practiced social distancing and/ or social isolation without leaving your home? For each question, the answer was categorized as: 1 - never (< 10 days), 2 - rarely (10-14 days), 3 - sometimes (15-30 days), 4 - almost always (31- 90 days) and 5 - always (> 90 days). Scores 4 and 5 were considered to have a high degree of adherence; the others represented a low degree of adherence. The elderly were allocated into two cohorts based on their degree of adherence to social distancing and isolation (15).
For the systematic construction of the observational study, we used the recommendations of the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE [20]).
Data Processing and Analysis
Data were organized and coded using the Microsoft ExcelR computer program, version 2016, and analyzed using the R CORE TEAM (2020) statistical software, version 4.0.2. Descriptive statistical analysis was used to report changes during follow-up in sociodemographic and clinical characteristics, level of physical activity, frailty status, and degree of adherence to social distancing and isolation. Older people who did not provide complete information at the first and second assessment waves were excluded.
The first and second cohorts were compared with the loss group to determine if there was a statistical difference between the proportions. Chi-squared test (when n ≥ 5) and Fisher’s exact test (when n < 5) were used to evaluate associations between reduced physical activity and frailty at the level of adherence to social distancing and isolation.
The Directed Acyclic Graph (DAG) minimum adjustment model was applied to sociodemographic and clinical variables to search for confounding covariates. For each confounding covariate indicated in the modeling, the Kaplan-Meier survival curves were presented, and the log-rank test was performed, comparing the survival curves for the outcome variables.
Several semi-parametric Cox proportional hazards models were built to obtain adjusted estimates of risk ratios. In the multivariable analyses, sociodemographic variables not indicated by the adjustment model were also included due to the heterogeneity of the sample and the crude estimates of hazard ratios (HR) were presented, with 95% CI, for the association between the covariates of interest and the level of frailty and decreased physical activity.
The Wald test was applied to the coefficient of the covariates in the survival models to calculate the p-value and the Schoenfeld residual analysis test was used to measure the assumption of proportional failure rates in the final Cox model. A 5% significance level was used for all statistical tests (15).
Ethical Aspects
The ethical principles of voluntary and consensual participation of the elderly were observed, by signing the informed consent form, following the recommendations contained in Resolution 466 of the National Health Council, of December 12, 2012 (21). The elderly participants were informed that they could refuse to answer any questions or even terminate their participation. The Human Research Ethics Committee of the Health Sciences Sector of the Federal University of Parana approved the research project, under opinion 4.766.196/2021.
Results
Table 1 shows that of the one hundred elderly people, most were female (63 %), self-declared white (74 %), aged between 70 and 79 (55 %), had a prominent level of education (41 %) and considered their financial situation to be average (45 %). The elderly who did not remain in the follow-up line were those in the lowest age group (60-69; 63.2 %) and female (62.3 %).
At the end of follow-up, 98 % of the elderly reported health problems, with cardiovascular diseases predominating (69 %). Multimorbidity affected 84 % of the elderly, with an even higher percentage using medication (92 %). Twenty-seven percent of participants reported falling in the second wave of the evaluation. The variable “polypharmacy” can be seen in 43 % of the elderly (Table 2 [15]).
Table 1 Distribution of Sociodemographic Characteristics of the Elderly (n = 168). Curitiba, Parana, Brazil, 2021
| Sociodemographic | First Evaluation Wave | Second Evaluation Wave | Losses | |||
|---|---|---|---|---|---|---|
| Variable | (n = 100) | % (CI 95 %) | (n = 100) | % (CI 95 %) | (n = 68) | % (CI 95 %) |
| Sex | ||||||
| Female | 63 | 63.0 (53.2; 71.8) | 63 | 63.0 (53.2; 71.8) | 43 | 63.2 (51.4; 73.7) |
| Male | 37 | 37.0 (28.2; 46.8) | 37 | 37.0 (28.2; 46.8) | 25 | 36.8 (26.3; 48.6) |
| Age Group | ||||||
| From 60 to 69 | 46 | 46.0 (36.6; 55.7) | 37 | 37.0 (28.2; 46.8) | 43 | 63.2 (51.4; 73.7) |
| From 70 to 79 | 50 | 50.0 (40.4; 59.6) | 55 | 55.0 (45.2; 64.4) | 21 | 30.9 (21.2; 42.6) |
| 80 or more | 4 | 4.0 (1.6; 9.8) | 8 | 8.0 (4.1; 15.0) | 4 | 5.9 (2.3; 14.2) |
| Education | ||||||
| Illiterate (< 1 year old) | 5 | 5.0 (2.2; 11.2) | 5 | 5.0 (2.2; 11.2) | 3 | 4.4 (1.5; 12.2) |
| Low schooling (1 to 4 years incomplete) | 27 | 27.0 (19.3; 36.4) | 15 | 15.0 (9.3; 23.3) | 21 | 30.9 (21.2; 42.6) |
| Average schooling (from 4 to 8 incomplete years) | 25 | 25.0 (17.5; 34.3) | 39 | 39.0 (30.0; 48.8) | 15 | 22.1 (13.8; 33.3) |
| High level of schooling (8 years or more) | 43 | 43.0 (33.7; 52.8) | 41 | 41.0 (31.9; 50.8) | 29 | 42.6 (31.6; 54.5) |
| Skin Color | ||||||
| White | 75 | 75.0 (65.7; 82.5) | 74 | 74.0 (64.6; 81.6) | 52 | 76.5 (65.1; 85.0) |
| Non-white | 25 | 25.0 (17.5; 34.3) | 26 | 26.0 (18.4; 35.4) | 16 | 23.5 (15.0; 34.9) |
| Marital status | ||||||
| Single | 6 | 6.0 (2.8; 12.5) | 5 | 5.0 (2.2; 11.2) | 6 | 8.8 (4.1; 17.9) |
| Married | 53 | 53.0 (43.3; 62.5) | 48 | 48.0 (38.5; 57.7) | 31 | 45.6 (34.3; 57.3) |
| Common-Law Marriage | 2 | 2.0 (0.6; 7.0) | 5 | 5.0 (2.2; 11.2) | 2 | 2.9 (0.8; 10.1) |
| Separate | 10 | 10.0 (5.5; 17.4) | 10 | 10.0 (5.5; 17.4) | 6 | 8.8 (4.1; 17.9) |
| Divorced | 9 | 9.0 (4.8; 16.2) | 10 | 10.0 (5.5; 17.4) | 9 | 13.2 (7.1; 23.3) |
| Widow | 20 | 20.0 (13.3; 28.9) | 22 | 22.0 (15.0; 31.1) | 14 | 20.6 (12.7; 31.6) |
| Financial situation | ||||||
| Good/Satisfactory | 43 | 43.0 (33.7; 52.8) | 40 | 40.0 (30.9; 49.8) | 30 | 44.1 (32.9; 55.9) |
| Median | 34 | 34.0 (25.5; 43.7) | 45 | 45.0 (35.6; 54.8) | 24 | 35.3 (25.0; 47.2) |
| Unsatisfactory | 23 | 23.0 (15.8; 32.2) | 15 | 15.0 (9.3; 23.3) | 14 | 20.6 (12.7; 31.6) |
Source: Own elaboration.
Table 2 Distribution of the Clinical Characteristics of the Elderly (n = 168). Curitiba, Parana, Brazil, 2021
| Clinical Variable | First Evaluation Wave | Second Evaluation Wave | Los ses | |||
|---|---|---|---|---|---|---|
| (n = 100) | % (CI 95 %) | (n = 100) | % (CI 95 %) | (n = 68) | % (CI 95 %) | |
| Health problem | 98 | 98 (93; 99.4) | 98 | 98 (93; 99.4) | 64 | 94.1 (85.8; 97.7) |
| Cognitive impairment | 0 | 0.0 (0.0; 3.7) | 2 | 2.0 (0.6; 7.0) | 1 | 1.5 (0.3; 7.9) |
| Cardiovascular | 68 | 68.0 (58.3; 76.3) | 69 | 69.0 (59.4; 77.2) | 39 | 57.4 (45.5; 68.4) |
| Musculoskeletal | 26 | 26.0 (18.4; 35.4) | 27 | 27.0 (19.3; 36.4) | 19 | 27.9 (18.7; 39.6) |
| Digestive | 10 | 10.0 (5.5; 17.4) | 8 | 8.0 (4.1; 15.0) | 8 | 11.8 (6.1; 21.5) |
| Metabolic | 43 | 43.0 (33.7; 52.8) | 43 | 43.0 (33.7; 52.8) | 33 | 48.5 (37.1; 60.2) |
| Respiratory | 6 | 6.0 (2.8; 12.5) | 8 | 8.0 (4.1; 15.0) | 2 | 2.9 (0.8; 10.1) |
| Dyslipidemia | 40 | 40.0 (30.9; 49.8) | 43 | 43.0 (33.7; 52.8) | 29 | 42.6 (31.6; 54.5) |
| Auditory | 9 | 9.0 (4.8; 16.2) | 15 | 15.0 (9.3; 23.3) | 3 | 4.4 (1.5; 12.2) |
| Visual | 49 | 49.0 (39.4; 58.7) | 45 | 45.0 (35.6; 54.8) | 35 | 51.5 (39.8; 62.9) |
| Urological | 9 | 9.0 (4.8; 16.2) | 14 | 14.0 (8.5; 22.1) | 7 | 10.3 (5.1; 19.8) |
| Neurological | 4 | 4.0 (1.6; 9.8) | 15 | 15.0 (9.3; 23.3) | 4 | 5.9 (2.3; 14.2) |
| Chronic pain | 14 | 14.0 (8.5; 22.1) | 9 | 9.0 (4.8; 16.2) | 7 | 10.3 (5.1; 19.8) |
| Mental disorder | 20 | 20.0 (13.3; 28.9) | 8 | 8.0 (4.1; 15.0) | 7 | 10.3 (5.1; 19.8) |
| Gynecological | 5 | 5.0 (2.2; 11.2) | 1 | 1.0 (0.2; 5.4) | 1 | 1.5 (0.3; 7.9) |
| Other diseases | 3 | 3.0 (1.0; 8.5) | 10 | 10.0 (5.5; 17.4) | 6 | 8.8 (4.1; 17.9) |
| Number of Diseases | ||||||
| 0 | 2 | 2.0 (0.6; 7.0) | 2 | 2.0 (0.6; 7.0) | 4 | 5.9 (2.3; 14.2) |
| 1 | 14 | 14.0 (8.5; 22.1) | 17 | 17.0 (10.9; 25.5) | 11 | 16.2 (9.3; 26.7) |
| 2 | 19 | 19.0 (12.5; 27.8) | 19 | 19.0 (12.5; 27.8) | 18 | 26.5 (17.4; 38.0) |
| 3 | 33 | 33.0 (24.6; 42.7) | 23 | 23.0 (15.8; 32.2) | 11 | 16.2 (9.3; 26.7) |
| 4 or more | 32 | 32.0 (23.7; 41.7) | 39 | 39.0 (30.0; 48.8) | 24 | 35.3 (25.0; 47.2) |
| Multimorbidity | 84 | 84.0 (75.6; 89.9) | 81 | 81.0 (72.2; 87.5) | 53 | 77.9 (66.7; 86.2) |
| Polypharmacy | - | - | 43 | 43.0 (33.7; 52.8) | - | - |
| Hospitalization in the last year | 15 | 15.0 (9.3; 23.3) | 6 | 6.0 (2.8; 12.5) | 10 | 14.7 (8.2; 25.0) |
| Fall in the last year | 25 | 25.0 (17.5; 34.3) | 27 | 27.0 (19.3; 36.4) | 9 | 13.2 (7.1; 23.3) |
Source: Own elaboration.
Table 3 shows that most older people had a low level of adherence to social distancing and isolation (69%). Older people with reduced physical activity showed a low degree of adherence to social distancing and isolation (n = 17; 81%) during the pandemic.
There was no association between the degree of adherence to social distancing and isolation and the level of physical activity (p = 0.288). Of the one hundred non-frail elderly at baseline, 53% progressed to pre-frailty, 3% to frailty, and 44% remained nonfrail during follow-up. The pre-frail and frail elderly had a lower degree of adherence to social distancing and isolation (n = 36; 64.3%), but there was no association between the degree of adherence to distancing and physical frailty (p = 0.351 [15]).
Table 3 Association between the Degree of Adherence to Social Distancing and Isolation of the Cohorts and the Level of Physical Activity and the State of Physical Frailty (n = 100). Curitiba, Parana, Brazil, 2021
| Maintaining Social Distance and Isolation | Reduced PhysicalActivity | P value | |||
|---|---|---|---|---|---|
| No | Yes | ||||
| (n = 79) | % (CI 95 %) | (n = 21) | % (CI 95 %) | ||
| High | 27 | 34.2 (24.7; 45.2) | 4 | 19.0 (7.7; 40.0) | 0.288* |
| Low | 52 | 65.8 (54.8; 75.3) | 17 | 81.0 (60.0; 92.3) | |
| Maintaining Social Distance and Isolation | Frailty | P value | |||
| Non Frail | Pre-Frail or Frail | ||||
| (n = 44) | % (CI 95 %) | (n = 56) | % (CI 95 %) | ||
| High | 11 | 25.0 (14.6; 39.4) | 20 | 35.7 (24.5; 48.8) | 0.351† |
| Low | 33 | 75.0 (60.6; 85.4) | 36 | 64.3 (51.2; 75.5) |
Note: *Fisher’s exact test; chi-squared test, p-value < 0.05.
Source: Own elaboration.
Table 4 shows that women had 2.53 times (95% CI, 1.01-6.34) higher risk of being classified as pre-frail or frail compared to men during cohort follow-up. Older people with a high family income (> 4 minimum wages) showed physical frailty after a shorter observation period compared to older people with a medium family income (2 to 4 minimum wages). Women had a 2.13-fold (95% CI, 1.06-4.26) higher risk of having a reduced level of physical activity compared to men during the cohort 1 follow-up (15).
Table 4 Proportional Hazards Models for the Association of Frailty and Decreased Physical Activity with Sociodemographic Characteristics. Curitiba, Parana, Brazil, 2021
| Physical Frailty | Decreased Physical Activity | |||
|---|---|---|---|---|
| Variables | Gross HR (95% CI) | Model | Gross HR (95% CI) | Model |
| Adjusted HR (95% CI) | Adjusted HR (95% CI) | |||
| Sex | ||||
| Male | 1. (Ref.) | 1. (Ref.) | 1. (Ref.) | 1. (Ref.) |
| Female | 1.56 (0.78; 3.12) | 2.53 (1.01; 6.34) | 1.64 (0.97; 2.76) | 2.13 (1.06; 4.26) |
| Education | ||||
| Low | 1. (Ref.) | 1. (Ref.) | 1. (Ref.) | 1. (Ref.) |
| Average | 1.17 (0.5; 2.74) | 0.99 (0.4; 2.49) | 1.58 (0.83; 3.02) | 1.45 (0.72; 2.89) |
| High | 1.26 (0.57; 2.77) | 1.04 (0.41; 2.61) | 1.36 (0.73; 2.55) | 1.31 (0.64; 2.67) |
| Age Group | ||||
| From 60 to 69 | 1. (Ref.) | 1. (Ref.) | 1. (Ref.) | 1. (Ref.) |
| 70 or more | 0.76 (0.41; 1.39) | 0.84 (0.38; 1.82) | 0.94 (0.59; 1.5) | 1.01 (0.55; 1.83) |
| Race/Color | ||||
| White | 1. (Ref.) | 1. (Ref.) | 1. (Ref.) | 1. (Ref.) |
| Non-white | 1.59 (0.79; 3.21) | 1.87 (0.82; 4.27) | 1.66 (0.99; 2.77) | 1.58 (0.85; 2.93) |
| Family income (MW†) | ||||
| Up to 2 | 1. (Ref.) | 1. (Ref.) | 1. (Ref.) | 1. (Ref.) |
| From 2 to 4 | 0.64 (0.3; 1.35) | 0.71 (0.28; 1.79) | 0.69 (0.4; 1.16) | 0.71 (0.36; 1.42) |
| More than 4 | 1.48 (0.72; 3.04) | 2.62 (0.98; 6.73) | 1.12 (0.64; 1.97) | 1.5 (0.71; 3.18) |
| Professional Status | ||||
| Not working | 1. (Ref.) | 1. (Ref.) | 1. (Ref.) | 1. (Ref.) |
| Working/pensioner | 0.88 (0.47; 1.61) | 0.6 (0.29; 1.25) | 0.88 (0.56; 1.39) | 0.75 (0.44; 1.28) |
| Multimorbidity | ||||
| Yes | 1. (Ref.) | 1. (Ref.) | 1. (Ref.) | 1. (Ref.) |
| No | 0.80 (0.38; 1.68) | 1.32 (0.52; 3.37) | 0.77 (0.44; 1.34) | 0.99 (0.49; 1.99) |
Note: Wald test used; †minimum wage.
Source: Own elaboration.
Discussion
Sociodemographic characteristics were similar after two years of follow-up, which is corroborated by a longitudinal study of 1702 elderly people in southern Brazil, in which no changes were observed after four years of follow-up (22).
The high percentage of multimorbidity (81%) was maintained during follow-up; these findings are supported by data from the Brazilian Longitudinal Study of Elderly Health (ELSI-Brazil), which included 9412 individuals aged ≥ 50 from 5 Brazilian macro-regions, in which the presence of multimorbidity was observed in 66.8% of the elderly aged 60 to 69, 73.3% of those aged 70 to 79, and 60.2% of those aged ≥ 80 (23).
Much lower figures were observed in Malaysia, where 3966 community- dwelling older people aged ≥ 60 were surveyed to determine the prevalence and factors associated with multimorbidity. Multimorbidity was found in 40.6% of the elderly (24). Similarly, a national study conducted in municipalities in Rio Grande do Sul with 676 elderly people aged ≥ 60 identified 45% of multimorbidity (25). Both studies examined fewer chronic diseases than the present study, which may explain the difference in the percentages observed.
Cardiovascular disease was prevalent, affecting 69% of the sample. In the analysis of the Royal College of General Practitioners- Research and Surveillance Center database, which included 1,275,174 primary care patients, cardiovascular disease was observed in 87.5% of the elderly aged 60 to 69, 74.2% of those aged 70 to 79, and 56% of those aged ≥ 80 (26). Lower values were observed in the longitudinal study conducted in the City of Sao Paulo, Sao Paulo, with data from three evaluation waves of the Health, Well-Being, and Ageing Study (Sabe), developed with samples of 2143, 1413, 1333 elderly participants (≥ 60). In the three evaluation waves, cardiovascular disease reached the following percentages: 17.9%, 22.2%, and 22.9%, respectively (27).
Physical inactivity can lead to increased blood pressure, type II diabetes mellitus, dyslipidemia, weight gain and central obesity. Physical inactivity alone or in combination with inadequate fruit and vegetable intake, alcohol abuse, and smoking are risk factors for cardiovascular disease. A cross-sectional study of 1553 elderly people participating in the Epidemiological Study of the Health Conditions of the Elderly in Florianopolis, Brazil, investigated the prevalence of simultaneous cardiovascular risk factors and their association with sociodemographic characteristics in elderly people in the southern region of Brazil. Physical inactivity was the most common cardiovascular risk factor (69.1%), observed in a significant percentage of women (73.4%). Among men, insufficient consumption of fruits and vegetables (67.2%) was the most common, followed by insufficient physical activity (61.8%[28])).
Among the numerous factors that contribute to physical inactivity, we highlight the lack of information about the importance of preventing chronic non-communicable diseases and the lack of time for physical activity. These factors could be minimized through prevention programs that focus on supported self-care and lifestyle changes.
Regarding medication use, polypharmacy was reported by 43% of the elderly. Similar data were observed in a study conducted in 17 European countries and Israel in the pre-pandemic period of COVID-19, using data from the Survey of Health, Ageing, and Retirement in Europe (Share). The results showed a prevalence of polypharmacy ranging from 26.3 to 39.9%. Switzerland, Croatia and Slovenia had the lowest prevalence rates, while Portugal, Israel and the Czech Republic were the countries with the highest prevalence of polypharmacy (29).
Most of the elderly in this sample progressed to pre-frailty or frailty. A prospective cohort with a three-year follow-up and a sample of 11,165 Chinese elderly aged ≥ 65 also observed progression to pre-frailty (46%) and frailty (10%) [30]). Discrepant data were observed in a cohort study using data from Sabe, conducted in the city of Sao Paulo (Brazil), with a four-year follow-up of 1399 elderly people aged ≥ 60. It was found that 27.7% had pre-frailty throughout the follow-up, 48% remained non-frailty, and 1.8% transitioned to frailty (31).
The diagnosis of physical frailty has gained prominence during the COVID-19 pandemic. An observational study in the UK and Italy with 1564 participants suggested that frailty was a better predictor of clinical progression than age or multimorbidity (32). Similar data were found in a study in New York City (United States of America) of 31,770 elderly people aged ≥ 65, which showed that frailty was a specific risk factor for hospitalization due to COVID-19 and for serious outcomes (33).
As physical frailty is a reversible condition, it requires appropriate care planning, as the chances of reversing physical pre-frailty are greater than those of frailty. A meta-analysis of a total of 42,775 community-dwelling elderly found that while a quarter of the elderly had a return to non-frail status from pre-frail status, only 3% of the frail elderly showed improvement (34).
Most of the elderly showed a low degree of adherence to social distancing and isolation (69%) in the second wave of the evaluation. In this study, there was no association between social distancing and isolation as a protective measure against COVID-19 and a decrease in physical activity among the elderly. Comparable results were observed in the cross-sectional study to assess the association between socioeconomic status, social participation, and physical activity during the pandemic in 999 Japanese elderly (≥ 65). There was no association between a decrease in physical activity among women who engaged in vigorous physical activity before the pandemic and restrictions at the onset of the COVID-19 pandemic (p = 0.40). In addition, women with social participation were more likely to increase or maintain physical activity (OR 1.67; 95% CI 1.13-2.45) [35]).
Divergent data were entered based on data from the Behavioral Survey (ConVid), a cross-sectional survey conducted in different states of Brazil with a sample of 9173 older people (≥ 60). Social distancing was adopted by 30.9% of the elderly, 12.2% did not adhere to it, and 56.9% practiced intense social distancing, indicating a high degree of adherence to social distancing (36).
A decrease in physical activity occurred in 21% of the sample. Different results were observed in the analysis of the CHARIOT COVID-19 Rapid Response study with 6219 participants from the United Kingdom. After the introduction of the social restrictions of the COVID-19 pandemic, a decrease in physical activity was reported in 50.9% of the sample, 8.6% maintained the level and 40.5% showed an increase in physical activity (37). Although studies suggest an association between decreased physical activity and social distancing and isolation, some data indicate the need for more in-depth research on this topic (38).
Concerning the divergent results for the percentage of adherence to social distancing and isolation measures during the COVID-19 pandemic, it must be considered that the studies used different assessment instruments. This reinforces the need to validate and standardize instruments that can verify adherence to protective measures throughout the pandemic and post-pandemic periods. The predominance of older people with a high level of education (41%) and multimorbidity (81%), as well as the fact that the patients included in the cohorts were not frail and had reduced physical activity, may have influenced the low level of adherence to social distancing and isolation.
ELSI-Brazil, which included 6149 individuals aged ≥ 50, investigated sociodemographic factors according to the occurrence of multimorbidity and the occurrence of protective behaviors against COVID-19. Participants with higher levels of education were less likely to stay at home during the COVID-19 pandemic. During the restrictive measures, 9.3% of people with multimorbidity reported leaving home for health care, while only 4.4% of people without multimorbidity left for the same reason (39).
There was no association between the physical frailty of the elderly and the degree of adherence to seclusion and restraint. In the pre-pandemic period, using data from the Longitudinal Population Health Index Survey of 606 older people (≥60 years old) and data collected from 2015 to 2018, similar to the current study, they found no association between social isolation and frailty. The researchers add that isolation may be an option and therefore have less of an impact on health than feeling lonely (40).
Also, in contrast to this study, a prospective cohort study of 593 older people (≥ 65) in Takasaki City (Japan) examined the relationship between frailty and the implementation of COVID-19 countermeasures. There was an association between the follow-up period in which the countermeasures were implemented and frailty (p = 0.003). However, it was not possible to determine whether the elderly complied with the preventive restrictions (41).
Differences between countries in the understanding of restrictions during the pandemic may explain the differences between the data collected and the association with physical frailty. In some countries, the population was instructed to take daily exercise outdoors; in others, they were not allowed to leave their homes. The harsh winter season, compared with countries with milder climates, also affected compliance with the restrictive measures and their impact on the health of the elderly population (42).
Elderly women are about twice as likely as men to be physically inactive. This is supported by a study from Sweden, which found an association between lower levels of physical activity (steps per day) and women (p < 0.0001) [43]). Worldwide, about one in three women and one in four men do not get enough physical activity to meet the recommendations of at least 150 minutes of moderate-intensity physical activity or 75 minutes of vigorous-intensity physical activity per week to stay healthy (44).
Older women are about two and a half times more likely to be classified as pre-frail or frail. Female gender is associated with higher rates of frailty, multimorbidity, sarcopenia, physical and functional impairment, and abdominal obesity, which leads to chronic inflammation. The higher prevalence of frailty in women may be due to their greater need for health care (45). Despite the high percentage of frailty in women, mortality rates are lower compared to men, suggesting the male-female health-survival paradox (46).
According to the 2015-2016 ELSI survey, 16.4% of men have difficulty with basic activities of daily living (BADLs) and 45.2% need assistance, while 18.7% of women have difficulty with BADLs and 66% need assistance. When it comes to receiving help, the proportions are reversed, with women receiving help 74.9% of the time and men 86.6% m(47). Although women are culturally the primary caregivers throughout their lives, they tend to receive less care than men as they age.
Women’s lower participation in physical activity is associated with less access to leisure time and lower-intensity activities than men. Lack of safe recreational areas, traditional roles, cultural norms, and inadequate community and social support also negatively affect women’s physical activity levels (48). The most common barriers to adherence to physical activity programs reported by women were lack of a place to exercise, lack of companionship, lack of energy, and fatigue or lack of motivation (49).
Older people with a high family income (> 4 minimum wages) showed physical frailty after a shorter observation period compared to older people with a medium family income (2 to 4 minimum wages). This finding differs from the literature, which has found an association between physical frailty and low family income among the elderly (50). The association between high family income and physical frailty in the elderly observed in this study is based on a reduction in the physical activity marker. Researchers have suggested that low levels of household activity to maintain the home and use of personal vehicles for transportation affect levels of physical activity and frailty (51).
Limitations of the study include the study design (cohort), which poses the risk of losing participants during follow-up; the sample consisted only of elderly people living in the community (primary health care), which may not reflect the same reality as elderly people living in long-term institutions; the use of a self-reported instrument to assess the level of physical activity - Minnesota Leisure Time Activities - and the consideration of a one-year periodmfor the references of physical activities of the elderly.
Management of frailty in the elderly according to the Physical Frailty Consensus - ICFSR International Clinical Practice Guidelines for Identification and Management - must include polypharmacy, management of sarcopenia, treatable causes of weight loss and fatigue (depression, hypotension, hypothyroidism and vitamin B12 deficiency); Offer multicomponent exercise programs to all frail older adults; refer frail older adults to an exercise program with progressive resistance training; provide protein-calorie supplementation when weight loss or malnutrition is diagnosed; and emphasize the importance of oral health (52).
These results help to plan professional practices in gerontological care; it is recommended to continue monitoring elderly people with multimorbidity, cardiovascular diseases and polypharmacy, during the restrictive measures and even after, because of the high percentage of these conditions found during the COVID-19 pandemic and reflected even after the declaration of the end of this public health emergency of international importance; Screening for physical frailty is recommended since more than half of the initial non-frail sample became pre-frail in a two-year follow-up; Supporting high-income elderly people with their health needs is recommended as a way to prevent physical frailty; Strategies involving the practice of physical activity are recommended, especially for women, since a decrease in physical activity was associated with female gender and the latter with frailty.
Conclusion
Sociodemographic characteristics remained similar between the first and second waves. Regarding frailty, a significant percentage of the elderly transitioned to pre-frailty and showed a decrease in physical activity as a prevalent marker of physical frailty.
The null hypothesis of the study was supported; there was no association between social distance and isolation among the elderly during the pandemic period and a decrease in physical activity and transition to frailty. Among the elderly who changed their baseline condition from non-frail to pre-frail and frail at follow-up, high family income (> 4 minimum wages) was identified as a confounding factor. In addition, this study suggests that elderly women have a higher risk of reduced physical activity, pre-frailty and frailty compared to elderly men.
There was a high percentage of older people with a low degree of adherence to social distancing and isolation as a protective measure due to the COVID-19 pandemic; however, there was no association between social distancing and isolation of older people during the pandemic period and physical frailty, as well as concerning decreased levels of physical activity.











 text in
text in