Remark
| 1) Why was this study conducted? |
| The study was carried out with the purpose of producing quality information on cancer incidence and mortality in the Municipality of Pasto to contribute to the generation of epidemiological knowledge, planning and evaluation of policies for the control of the disease both locally and nationally. |
| 2) What were the most relevant results of the study? |
| The five-year follow-up of cancer incidence and mortality allows the behavior of the different types of cancer to be monitored. The results of the 1998-2017 trend show that in women the incidence of breast and thyroid cancer increased significantly and there was a decrease in cervical cancer. In men, the incidence of prostate cancer continues to rise, stomach cancer shows a slight decrease, and lung cancer remains stable. Regarding cancer mortality, in women it was observed that it continues to be higher due to breast cancer, followed by stomach tumors; in men the leading cause of death is stomach cancer followed by prostate tumors. |
| 3) What do these results contribute? |
| The results obtained indicate that the behavior of the disease follows the national trend regarding breast and cervical cancer in women and in men with prostate cancer. At the regional level, despite the slight decrease in stomach cancer, mortality continues to be a concern regarding the timeliness of diagnosis and treatment. In women, it is necessary to deepen the monitoring of thyroid cancer cases due to the increase in the last five years. This information serves to identify intervention priorities within the framework of decision-making in public health at the territorial level, as it has also facilitated the generation of new knowledge through research that contributes to cancer control. On the other hand, it has contributed to the National Cancer Institute (INC) planning control strategies and making incidence estimates based on mortality for the Colombian territory. |
Introduction
Cancer is a rising public health problem, due to its multifactorial origin and the growing adoption of risk habits that generate large burdens in both developed and undeveloped countries; and which impact health systems because treatments need to be evaluated with a multidisciplinary approach and supported by the use of different technologies; they also carry consequences at a social, economic, family and psycho-affective level 1-4.
According to the World Health Organization (WHO) cancer is the second cause of death in the world; in 2020, lung cancer caused the highest number of deaths, followed by colorectal, liver, gastric and breast cancer; it is estimated that 50 % of new cancer cases and 60% of deaths occur in developing countries 5-7. One third of the different types of cancer is preventable; and if patients receive a timely diagnosis, another third is curable. However, 75% of patients living in developing countries are diagnosed late, when they present tumors in an advanced stage or without a favorable prognosis. It is estimated that by 2040, the incidence of cancer will increase in all countries; however, it will be higher in low-income countries 7.
For countries, it is essential to have good quality statistics on the burden of cancer that allow an accurate diagnosis of the problem; and that, at the same time, may serve as a basis for designing, implementing, and monitoring control measures, in order to reduce the human, social and economic costs produced by this group of diseases. In this way, it would be possible to prevent them from exceeding the capacity of each country to combat them 8,9. In Colombia there are five population-based cancer registries (PBCR), which are recognized by the International Agency for Research on Cancer (IARC); and which provide high quality data on incidence in Cali, Pasto, Manizales, Barranquilla and Bucaramanga that allow valid statistics to be produced about patterns, trends, and cancer survival 8-10.
The Population Cancer Registry of the Municipality of Pasto (RPCMP) has kept this information permanently since 1998; and the estimated values are comparable with those reported by other cancer registries of similar populations. This information serves to identify intervention priorities within the framework of decision-making in public health at territorial level; it has also facilitated the generation of new knowledge through research that contributes to cancer control. On the other hand, together with that of the other PBCR, it has contributed to the National Cancer Institute (INC) planning control strategies and making incidence estimates based on mortality for the Colombian territory 10. In order to contribute to the knowledge of the behavior of this disease and contribute with quality data that support the implementation of intervention programs, aimed at reducing the burden of this disease in the local context, this study aims to determine the incidence and mortality by cancer in the municipality of Pasto during the period 2013-2017.
Materials and Methods
The Cancer Population Registry is a permanent cancer public health surveillance system that performs characterization reports on the epidemiological profile of cancer in the Municipality of Pasto, with indicators of morbidity and mortality in five-year periods. For this report, the following criteria were taken into account:
• Study population: it corresponds to the population residing in the municipality of Pasto, capital of the Nariño Province, which is located in the south-west of Colombia. According to data reported by the National Administrative Department of Statistics (DANE) in the last census of 2018, the Municipality had 352,326 inhabitants, 47.3% males and 52.7% females. Compared to the previous official census of 2005, the population has presented an aging represented by a decrease in the percentage of individuals in early ages, and an increase in the population in adulthood or elderly stages (Figure 1) 11.
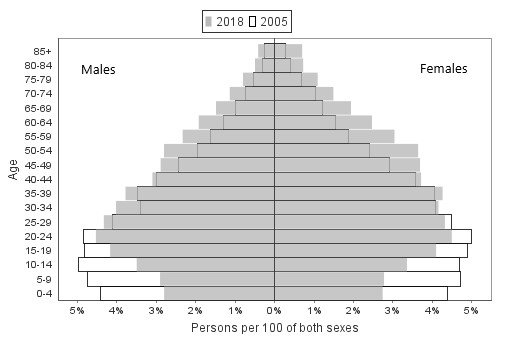
Figure 1 Population pyramid according to five-year age groups. Males and Females, Municipality of Pasto, 2005 and 2018. Source: Population estimates and projections for the period 2005-2018 DANE 11.
Definition of cancer case for incidence: there were included all malignant tumors (Code 3 of behavior in the CIEO-3) diagnosed in people residing in the Municipality of Pasto during the period 2013-2017 by any valid diagnostic method (histology, cytology, imaging, endoscopy, clinical or by death certificate) according to IARC 12. Basal cell and squamous cell carcinoma-type skin tumors (N= 955) were excluded. Cancer cases in persons of unknown age (N= 5) were also excluded.
Case definition for mortality: there were included all deaths from cancer according to the basic cause of death (codes C00-C906 in ICD-10) registered between 2013 and 2017 by medical personnel in people residing in the Municipality of Pasto. On the other hand, deaths from “non-specific site” uterine cancer (C55, N= 12), are redistributed into the “cervix uteri” and “corpus uteri” categories, taking into account the proportion of deaths observed by age, according to IARC guidelines 12.
Study variables and information processing. The analyzed data and the information collection process were established by the population cancer registries following the IARC guidelines, in order to allow the results to be comparable with national and international registries; these variables are described in the study on cancer incidence and mortality trends in Pasto, Colombia 10.
The information on morbidity was actively collected (direct review of the data in each source) in all the health institutions in the municipality of Pasto that generate information on patients diagnosed with cancer; they are: hospitals, clinics, oncology units, pathology laboratories, medical centers, specialized clinics and the Municipal Secretary of Health; being the last one the body in charge of processing the death certificates of the municipality. The information on mortality comes from the DANE’s vital statistics information system.
The topographic (site) and morphological (histology) coding of the tumors was performed with the International Classification of Diseases for Oncology, third edition (ICD-O-3) 13. It was carried out the conversion of the ICD-O-3 topographic codes to ICD-10 (International Classification of Diseases 10th edition); and some sites were grouped as it is done in the IARC Global Cancer Observatory (Table 1) 7. Similarly, for the analysis of mortality, the causes of death coded in ICD-10 were grouped according to the major categories of mortality from cancer of the WHO.
Table 1 Municipality of Pasto. Absolute and relative frequency of new cases of cancer, incidence rates by tumor site, raw and standardized by age per 100,000 inhabitants. Males and Females, 2013-2017
| Site | Males | Females | CIE-10 | ||||||
|---|---|---|---|---|---|---|---|---|---|
| N | % | CR | ASR | N | % | CR | ASR | ||
| Tongue | 4 | 0.2 | 0.4 | 0.4 | 14 | 0.7 | 1.3 | 1.1 | C01-C02 |
| Mouth | 2 | 0.1 | 0.2 | 0.2 | 6 | 0.3 | 0.6 | 0.4 | C03-C06 |
| Salivary gland | 8 | 0.5 | 0.9 | 0.9 | 7 | 0.3 | 0.7 | 0.6 | C07-C08 |
| Amygdala | 0 | 0.0 | 0.0 | 0.0 | 2 | 0.1 | 0.2 | 0.1 | C09 |
| Other oropharynx | 1 | 0.1 | 0.1 | 0.1 | 0 | 0.0 | 0.0 | 0.0 | C10 |
| Nasopharynx | 1 | 0.1 | 0.1 | 0.1 | 0 | 0.0 | 0.0 | 0.0 | C11 |
| Hypopharynx | 0 | 0.0 | 0.0 | 0.0 | 1 | 0.0 | 0.1 | 0.1 | C12-C13 |
| Esophagus | 21 | 1.3 | 2.2 | 2.2 | 10 | 0.5 | 1.0 | 0.8 | C15 |
| Stomach | 266 | 16.5 | 28.3 | 28.0 | 158 | 7.3 | 15.2 | 12.7 | C16 |
| Small intestine | 9 | 0.6 | 1.0 | 1.0 | 9 | 0.4 | 0.9 | 0.7 | C17 |
| Colon | 60 | 3.7 | 6.4 | 6.3 | 89 | 4.1 | 8.5 | 7.0 | C18 |
| Rectum | 46 | 2.9 | 4.9 | 4.9 | 47 | 2.2 | 4.5 | 3.8 | C19-C20 |
| Anus | 7 | 0.4 | 0.7 | 0.8 | 6 | 0.3 | 0.6 | 0.5 | C21 |
| Liver | 36 | 2.2 | 3.8 | 3.8 | 39 | 1.8 | 3.7 | 2.9 | C22 |
| Gallbladder | 38 | 2.4 | 4.0 | 4.1 | 89 | 4.1 | 8.5 | 7.0 | C23-C24 |
| Pancreas | 47 | 2.9 | 5.0 | 4.9 | 63 | 2.9 | 6.0 | 5.0 | C25 |
| Nose, sinuses | 2 | 0.1 | 0.2 | 0.2 | 2 | 0.1 | 0.2 | 0.2 | C30-C31 |
| Larynx | 11 | 0.7 | 1.2 | 1.2 | 2 | 0.1 | 0.2 | 0.1 | C32 |
| Trachea, bronchi and lung | 77 | 4.8 | 8.2 | 8.2 | 46 | 2.1 | 4.4 | 3.7 | C33-C34 |
| Other thoracic organs | 2 | 0.1 | 0.2 | 0.2 | 4 | 0.2 | 0.4 | 0.3 | C37-C38 |
| Bones | 6 | 0.4 | 0.6 | 0.6 | 7 | 0.3 | 0.7 | 0.6 | C40-C41 |
| Skin melanoma | 22 | 1.4 | 2.3 | 2.3 | 38 | 1.8 | 3.6 | 3.1 | C43 |
| Other skin tumors | 15 | 0.9 | 1.6 | 1.6 | 17 | 0.8 | 1.6 | 1.3 | C44 |
| Mesothelioma | 6 | 0.4 | 0.6 | 0.6 | 1 | 0.0 | 0.1 | 0.1 | C45 |
| Kaposi's sarcoma | 5 | 0.3 | 0.5 | 0.5 | 1 | 0.0 | 0.1 | 0.1 | C46 |
| Connective and soft tissue | 15 | 0.9 | 1.6 | 1.6 | 17 | 0.8 | 1.6 | 1.4 | C47, C49 |
| Breast | 3 | 0.2 | 0.3 | 0.3 | 423 | 19.7 | 40.6 | 35.1 | C50 |
| Vulva | - | - | - | - | 9 | 0.4 | 0.9 | 0.7 | C51 |
| Vagina | - | - | - | - | 4 | 0.2 | 0.4 | 0.3 | C52 |
| Cervix | - | - | - | - | 229 | 10.6 | 22.0 | 18.9 | C53 |
| Corpus uteri | - | - | - | - | 73 | 3.4 | 7.0 | 6.1 | C54 |
| Non-specific uterus | - | - | - | - | 4 | 0.2 | 0.4 | 0.3 | C55 |
| Ovary | - | - | - | - | 98 | 4.6 | 9.4 | 8.2 | C56 |
| Penis | 23 | 1.4 | 2.4 | 2.4 | - | - | - | - | C60 |
| Prostate | 417 | 25.9 | 44.3 | 44.2 | - | - | - | - | C61 |
| Testis | 70 | 4.4 | 7.4 | 7.0 | - | - | - | - | C62 |
| Other male genitalia | 1 | 0.1 | 0.1 | 0.1 | - | - | - | - | C63 |
| Kidney | 21 | 1.3 | 2.2 | 2.3 | 18 | 0.8 | 1.7 | 1.6 | C64 |
| Renal pelvis | 1 | 0.1 | 0.1 | 0.1 | 0 | 0.0 | 0.0 | 0.0 | C65 |
| Ureter | 1 | 0.1 | 0.1 | 0.1 | 2 | 0.1 | 0.2 | 0.1 | C66 |
| Urinary bladder | 33 | 2.1 | 3.5 | 3.5 | 23 | 1.1 | 2.2 | 1.8 | C67 |
| Eye | 6 | 0.4 | 0.6 | 0.6 | 7 | 0.3 | 0.7 | 0.6 | C69 |
| Brain and nervous system | 36 | 2.2 | 3.8 | 3.7 | 45 | 2.1 | 4.3 | 3.7 | C70-C72 |
| Thyroid | 30 | 1.9 | 3.2 | 3.1 | 262 | 12.2 | 25.1 | 22.3 | C73 |
| Adrenal gland | 0 | 0.0 | 0.0 | 0.0 | 1 | 0.0 | 0.1 | 0.1 | C74 |
| Other endocrine tumors | 1 | 0.1 | 0.1 | 0.1 | 0 | 0.0 | 0.0 | 0.0 | C75 |
| Hodgkin lymphoma | 10 | 0.6 | 1.1 | 1.1 | 8 | 0.4 | 0.8 | 0.8 | C81 |
| Non-Hodgkin lymphoma | 72 | 4.5 | 7.7 | 7.7 | 72 | 3.3 | 6.9 | 5.9 | C82-C86, C96 |
| Immunoproliferative diseases | 2 | 0.1 | 0.2 | 0.2 | 3 | 0.1 | 0.3 | 0.3 | C88 |
| Multiple myeloma | 22 | 1.4 | 2.3 | 2.4 | 20 | 0.9 | 1.9 | 1.6 | C90 |
| Lymphoid leukemia | 32 | 2.0 | 3.4 | 3.5 | 25 | 1.2 | 2.4 | 2.4 | C91 |
| Myeloid leukemia | 18 | 1.1 | 1.9 | 1.9 | 24 | 1.1 | 2.3 | 2.2 | C92-C94 |
| Unspecified leukemia | 10 | 0.6 | 1.1 | 1.0 | 8 | 0.4 | 0.8 | 0.6 | C95 |
| Myeloproliferative disorders | 4 | 0.2 | 0.4 | 0.4 | 3 | 0.1 | 0.3 | 0.3 | It includes ICD-O-3 9950/3, 9960-9965/3, 9971/3 y 9975/3 |
| Myelodysplastic syndromes | 13 | 0.8 | 1.4 | 1.3 | 13 | 0.6 | 1.2 | 1.0 | It includes ICD-O-3 9980-9983/3, 9985-9989/3, 9991/3 y 9992/3 |
| Other and unspecified malignant neoplasms | 75 | 4.7 | 8.0 | 7.8 | 102 | 4.7 | 9.8 | 8.2 | C26, C48, C76, C80 |
| All primary sites | 1,608 | 100 | 170.9 | 169.4 | 2,151 | 100 | 206.5 | 176.6 | C00-96 |
| All sites except C44 | 1,593 | 99.1 | 169.3 | 167.8 | 2,134 | 99.2 | 204.8 | 175.3 | C00-43,45-96 |
N: number of cases
%: Frequency of cases
CR: Crude incidence rate x 100,000 males or females per year
ASR: age-adjusted rates x 100,000 males or females per year
Quality criteria on incidence information: To evaluate the quality of the information, there were applied the following indices established by the IARC 12.
Percentage of cases with microscopic verification (%VM) or cytopathology.
Percentage of cases registered only by death certificates (% SCD).
Mortality-incidence ratio (M/I). It corresponds to the quotient between the number of deaths attributed to a specific cancer and the number of incident cases in the same period. Incident and mortality cases do not necessarily refer to identical cases.
Percentage of cancer deaths that were certified by medical personnel.
Percentage of deaths from cancer of unknown primary tumor site.
Analysis of the information
Incidence and mortality are presented both globally and specifically according to sex, age at diagnosis or death (18 five-year categories) and tumor site, using absolute frequencies (N), relative frequencies (%), crude rates (CR) and age-standardized rates (ASR).
For calculating the rates, it was used as population denominator the DANE's mid-year estimates and projections for the 2013-2017 period. Rates were adjusted for age by the direct method, using the standard world population 14.
To assess the trend in incidence, a trend analysis of annual rates was performed using joinpoint or segmented linear regression. three change points (joinpoints) and four linear segments were accepted. The annual percentage change (APC) was estimated for each segment and the average annual percentage change (AAPC) was calculated for the entire period. The models were fitted with the weighted least squares method and the final model was selected with the Monte Carlo permutation test. The trend analysis was carried out in the Joinpoint 4.0 program produced by the Surveillance Research Program of the National Cancer Institute of the United States 15.
Ethical considerations and confidentiality of information
The handling of the information followed the confidentiality rules established by the International Agency for Research on Cancer (IARC) 16, which regulates the use of data for scientific purposes without the disclosure of personal data, guaranteeing respect and non-maleficence towards patients. On the other hand, the Population Registry of Cancer of the Municipality of Pasto and the research derived from it have agreements with the sources of information to guarantee the adequate flow of data.
Results
Overall cancer morbidity and mortality
During the period 2013-2017 in the municipality of Pasto, there were 3,759 new cases; 1,608 in males (CR 170.9 cases per 100,000 males-year; ASR 169.4 cases per 100,000 males-year), and 2,151 cases in females (CR 206.5 cases per 100,000 females-years; ASR 176.6 cases per 100,000 females-years).
In this same period in the municipality of Pasto, there were 2,130 cancer deaths; 934 in males (CR 99.3 deaths per 100,000 males-year; ASR 97.8 deaths per 100,000 males-year), and 1,196 deaths in females (CR 114, 8 deaths per 100,000 females-years; ASR 95.1 deaths per 100,000 females-years).
Age-specific cancer morbidity and mortality
Cancer incidence rates increase with age; 57.5% of incident cases in males and 41.6% in females occurred after 65 years, while 1.5% and 1.2% of cases in males and females occurred in children under 15 years of age (Figure 2). The average age of diagnosis in males was 64 years and 60 years in females.
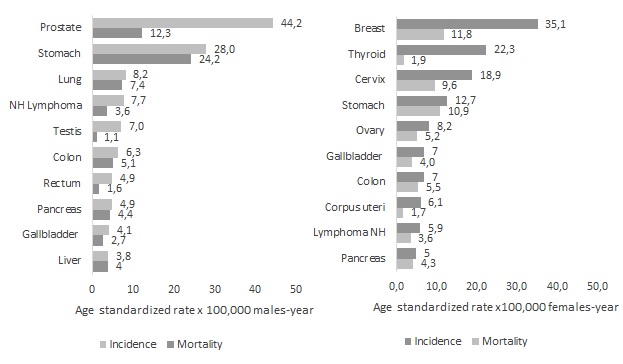
Figure 2 Municipality of Pasto. Age-specific Incidence (left) and Mortality (right) rates per 100,000. Males and females, 2013-2017. TEE: Age Specific rate x 100,000 inhabitants
Similarly, mortality was higher from 65 years on (Figure 2), both in males (61.6%) and females (57.8%). The average age of death for males and females is 67 years of age.
Specific morbidity and mortality by tumor site
In males, the tumors with the highest incidence rates were: prostate (ASR 44.2 cases per 100,000 males-years), stomach (ASR 28 cases per 100,000 males-years) lung (ASR 8.2 cases per 100,000 males-year), Non-Hodgkin's lymphoma (ASR 7.7 cases per 100,000 males-year) and testis (ASR 7 cases per 100,000 males-year). While in females, there were tumors of: Breast (ASR 35.1 cases per 100,000 females-year), thyroid (ASR 22.3 cases per 100,000 females-year), cervix (ASR 18.9 cases per 100,000 females-years), stomach (ASR 12.7 cases per 100,000 females-years) and ovary (ASR 8.2 cases per 100,000 females-years) (Figure 3 and Table 1).
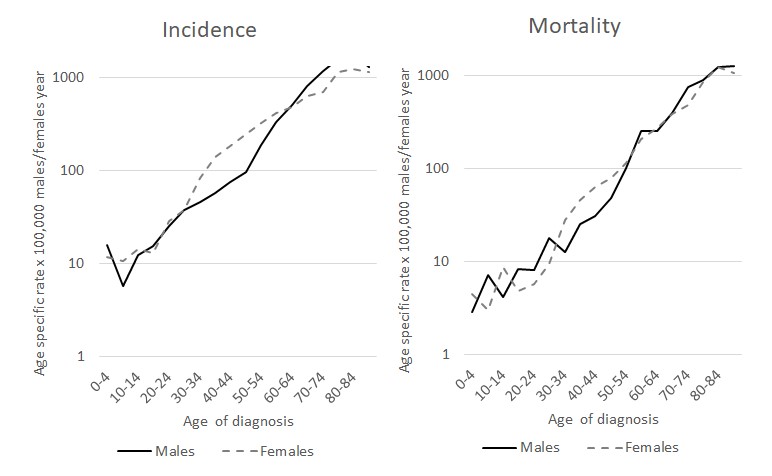
Figure 3 Municipality of Pasto. Incidence rates and deaths from cancer according to the first 10 incident sites in males (left) and females (right), period 2013-2017
The main causes of cancer mortality in males were tumors of: Stomach (ASR 24.2 deaths per 100,000 males-years); prostate (ASR 12.3 deaths per 100,000 males-years); lung (ASR 7.4 deaths per 100,000 man-years); colon and rectum (ASR 6.7 deaths per 100,000 man-years); and lymphomas and myeloma (ASR 6.0 deaths per 100,000 man-years). In females, there were tumors of: breast (ASR 11, 8 deaths per 100,000 females-years); stomach (ASR 10.9 deaths per 100,000 females-years); cervix (ASR 9.6 deaths per 100,000 females-years). year); colon and rectum (ASR 7.6 deaths per 100,000 females-years); and liver (ASR 5.4 deaths per 100,000 females-years). (Figure 3, Table 2).
Table 2 Municipality of Pasto. Absolute and relative frequency of deaths from cancer, mortality rates by tumor site, crude and standardized by age per 100,000 inhabitants. Males and Females, 2013-2017
| Site | Males | Females | CIE-10 | ||||||
|---|---|---|---|---|---|---|---|---|---|
| N | % | CR | ASR | N | % | CR | ASR | ||
| Oral cavity | 9 | 1.0 | 1.0 | 0.9 | 10 | 0.8 | 1.0 | 0.7 | C00-14 |
| Esophagus | 28 | 3.0 | 3.0 | 2.9 | 15 | 1.3 | 1.4 | 1.1 | C15 |
| Stomach | 232 | 24.8 | 24.7 | 24.2 | 139 | 11.6 | 13.3 | 10.9 | C16 |
| Small intestine | 2 | 0.2 | 0.2 | 0.2 | 5 | 0.4 | 0.5 | 0.4 | C17 |
| Colon and rectum | 63 | 6.7 | 6.7 | 6.7 | 98 | 8.2 | 9.4 | 7.6 | C18-20 |
| Liver | 38 | 4.1 | 4.0 | 4.0 | 70 | 5.9 | 6.7 | 5.4 | C22 |
| Pancreas | 42 | 4.5 | 4.5 | 4.4 | 54 | 4.5 | 5.2 | 4.3 | C25 |
| Lung | 70 | 7.5 | 7.4 | 7.4 | 60 | 5.0 | 5.8 | 4.8 | C34 |
| Melanoma and other skin tumors | 19 | 2.0 | 2.0 | 2.0 | 28 | 2.3 | 2.7 | 2.2 | C43-44 |
| Breast | 146 | 12.2 | 14.0 | 11.8 | C50 | ||||
| Cervix | - | - | - | - | 120 | 10.0 | 11.5 | 9.6 | C53 |
| Corpus uteri | - | - | - | - | 22 | 1.8 | 2.1 | 1.7 | C54 |
| Ovary | - | - | - | - | 64 | 5.4 | 6.1 | 5.2 | C56 |
| Prostate | 120 | 12.8 | 12.8 | 12.3 | - | - | - | - | C61 |
| Bladder | 20 | 2.1 | 2.1 | 2.0 | 13 | 1.1 | 1.2 | 1.0 | C67 |
| Lymphomas and myeloma | 56 | 6.0 | 6.0 | 6.0 | 63 | 5.3 | 6.0 | 5.0 | C90, 81,82, 85,96 |
| Leukemias | 42 | 4.5 | 4.5 | 4.2 | 47 | 3.9 | 4.5 | 4.2 | C91-C95 |
| Other neoplasms | 193 | 20.7 | 20.5 | 20.5 | 242 | 20.2 | 23.2 | 19.3 | - |
| All sites | 934 | 100 | 99.3 | 97.8 | 1,196 | 100 | 114.8 | 95.1 | C00-96 |
N: number of deaths
%: Frequency of deaths
CR: Crude mortality rate x 100,000 males or females per year
ASR: age-adjusted rates x 100,000 males or females per year
Specific morbidity and mortality by tumor site and age groups
Cancer morbidity and mortality according to age is distributed as follows:
In the age group of 0-14 years, lymphoid leukemia represent the highest proportion of incident cases for both sexes: 37.5% in males, and 24% in females; followed by cancer of the brain and central nervous system, 16.7 % in males; and myeloid leukemia, 16.0% in females. Brain tumors and lymphoid leukemia account for approximately 67% of deaths for both sexes.
In the group of 15-49 years, testicular cancer ranks first in males with 24.2%; followed by stomach cancer, 12.5%. Regarding females, the higher proportion of cases was for breast cancer, 24.4%; and thyroid cancer, 23.7%. The main causes of mortality for males were tumors of the stomach, 29.8%; and testis, 8.6%. In females, they were breast tumors, 16.8%; and cervix, 14.7%.
In the 50-64 age group, there was a higher incidence in males of prostate cancer, 20.7%; and stomach, 19.2%. Regarding females, there was a higher incidence of breast cancer, 25.5%; and cervix, 12.5%. In this age group, in males, there was a higher percentage of deaths due to stomach tumors, 30.2%; and lung tumors, 8.6%. Regarding females, there was a higher incidence of breast tumors, 15.8%; and cervix, 13.5 %.
In the population aged 65 and over, prostate cancer (35.5%), and stomach cancer (16.9%) in males were the most frequent sites; while in females, there was a higher incidence of breast cancer (12.8%), followed by stomach cancer (10.7%), which displaces cervical cancer (7.3%). The main causes of cancer mortality in males were tumors of stomach, 22.1%; and prostate, 18.6%. Regarding females, they were tumors of stomach, 12.0%; and breast, 9.6%.
Cancer incidence trend 1998-2017
In the incidence trend analysis (Table 3, Figure 4), the following was identified:
Table 3 Municipality of Pasto. Trend of the incidence of the most frequent tumors in Males and Females, 1998-2017
| Tumor | Period | APC | CI APC 95% | p-value | AAPC | CI AAPC 95% | p-value |
|---|---|---|---|---|---|---|---|
| Breast Females | 1998-2017 | 3.6 | (2.4;4.8) | 0.00 | 3.6 | (2.4;4.8) | 0.00 |
| Cervix | 1998-2017 | -2.1 | (-3.4; -0.8) | 0.00 | -2.1 | (-3.4; -0.8) | 0.00 |
| Thyroid | 1998-2001 | -19.6 | (-51.4; 33.1) | 0.37 | 5.0 | (-2.7; 13.3) | 0.21 |
| 2001-2017 | 10.4 | (7.5; 13.4) | 0.00 | ||||
| Stomach Males | 1998-2012 | -3.2 | (-4.5;-1.8) | 0.00 | -1.2 | (-3.0;0.7) | 0.22 |
| 2012-2017 | 4.7 | (-2.1; 11.9) | 0.17 | ||||
| Lung Males | 1998-2017 | 1.4 | (-1.0; 3.9) | 0.24 | 1.4 | (-1.0; 3.9) | 0.24 |
| Prostate | 1998-2017 | 5.2 | (3.6; 6.8) | 0.00 | 5.2 | (3.6; 6.8) | 0.00 |
APC: Annual percentage change
CI APC: Confidence Intervals for Annual Percentage Change
AAPC: Average Annual Percentage of Change
CI AAPC: Confidence intervals of the average annual percentage of change
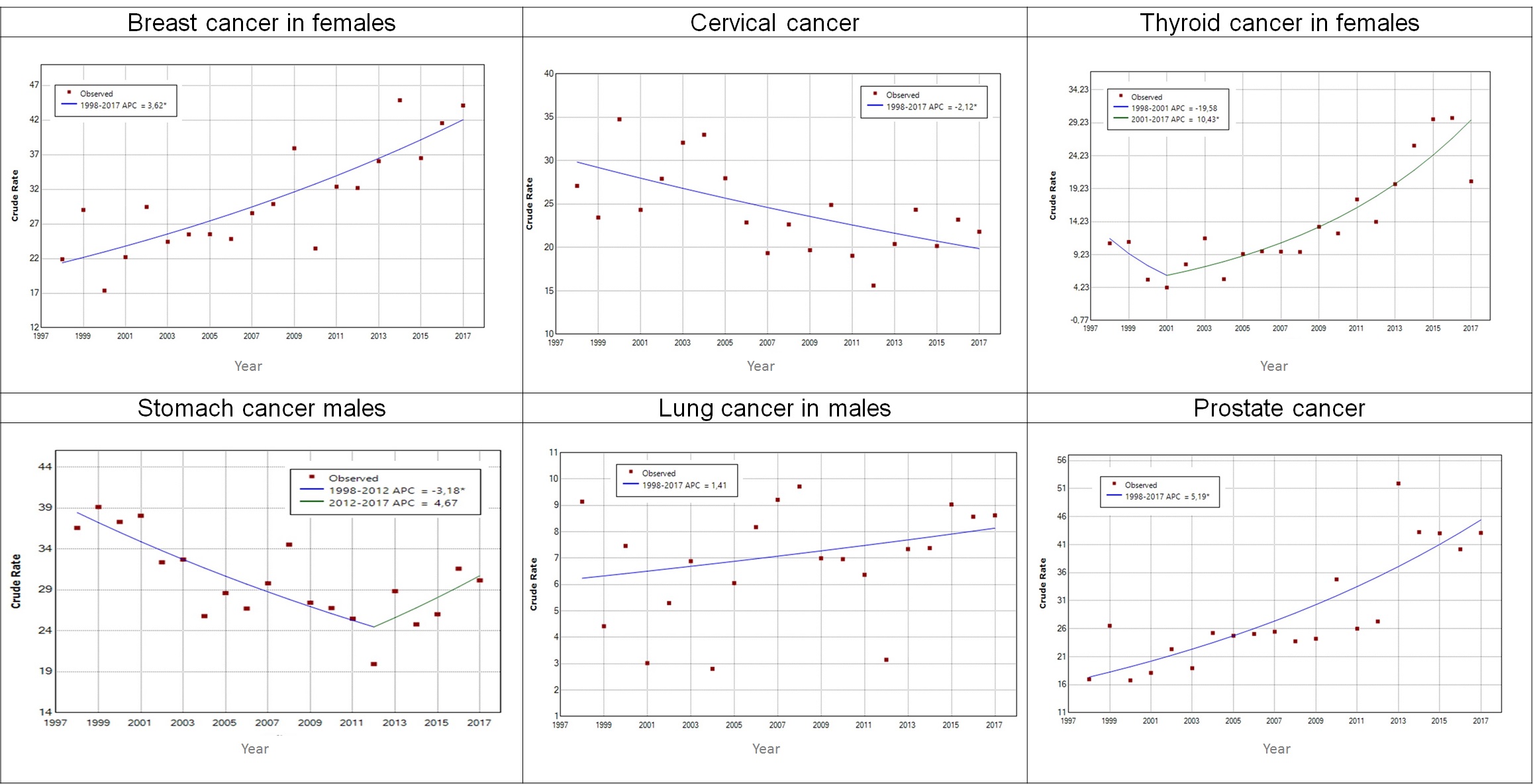
Figure 4 Municipality of Pasto. Trend of the incidence of the most frequent tumors in Males and Females, 1998-2017
The incidence of breast cancer in females increased 3.6% annually (p-value= 0.00), from an ASR of 21.9 in 1998 to 44.1 cases per 100,000 females-years in 2017.
The incidence of cervical cancer decreased 2.1% annually (p-value= 0.00), from an ASR of 27.1 in 1998 to 21.8 cases per 100,000 females-years in 2017.
The incidence of thyroid cancer in females did not present significant changes in the period 1998-2001 (p-value= 0.37); from this year on, it increased 10.4% annually (p-value= 0.00), from an ASR of 4.23 in 2001 to 20.36 cases per 100,000 females-years in 2017.
The incidence of stomach cancer in males decreased significantly by 3.2% annually (p-value= 0.00), from an ASR of 36.6 in 1998 to 19.4 cases per 100,000 males-years in 2012. From this year on, until 2017, an increase in incidence rates (4.7%) can be seen; however, it is not statistically significant.
The incidence of lung tumors in males was constant (p-value= 0.24), and the average of their age-adjusted incidence annual rates was 6.83 cases per 100,000 males-years.
The incidence of prostate tumors increased significantly by 5.2% annually (p-value= 00.00), from an ASR of 16.98 in 1998 to 43.1 cases per 100,000 males-years in 2017.
Morbidity and mortality information quality indices
The aforementioned results must be interpreted taking into account the following quality indicators.
The percentage of incident cases of cancer with microscopic verification (%VM) was 83.9% for all tumors; being 83.9% for males, and 83.8% for females. The percentage of registered cases whose only evidence was the death certificate (%DCO) for all tumors was 4.7%; being 4.7% for males, and 4.9% for females. The remaining cases were diagnosed by other methods. The main quality indicators by site are presented in Table 4.
Table 4 Municipality of Pasto. Quality indices of the main sites. Males and Females, 2013-2017
| Site | Males | |||
|---|---|---|---|---|
| N | *%VM | **%DCO | ***M/I | |
| Prostate | 417 | 87.8 | 3.6 | 0.3 |
| Stomach | 266 | 91.0 | 2.6 | 0.9 |
| Trachea, bronchi and lung | 77 | 67.5 | 7.8 | 0.9 |
| Non-Hodgkin lymphoma | 72 | 91.7 | 2.8 | 0.5 |
| Testis | 70 | 98.6 | 0.0 | 0.2 |
| All primary sites | 1,608 | 83.9 | 4.3 | 0.6 |
| Site | Females | |||
| N | *%VM | *%DCO | *M/I | |
| Breast | 423 | 97.6 | 0.9 | 0.3 |
| Thyroid | 262 | 95.0 | 0.4 | 0.1 |
| Cervix | 229 | 94.8 | 1.7 | 0.5 |
| Stomach | 158 | 78.5 | 8.2 | 0.9 |
| Ovary | 98 | 81.6 | 5.1 | 0.6 |
| All primary sites | 2,151 | 83.8 | 4.9 | 0.5 |
*%VM: percentage of cases with microscopic verification (cytology-hematology and histology of the primary tumor)
**% DCO: percentage of cases registered only by death certificates
***M/I: mortality-incidence ratio
On the mortality basis, 99% of all cancer deaths were certified by medical personnel; and 6.1% were deaths due to tumors of unknown primary site. In addition, the registered deaths with unspecified uterine cancer (C55) were 0.6%.
Discussion
For cancer control, Colombia has issued a series of regulations and policies focused on achieving effective interventions that have an impact on the burden of the disease; however, in the implementation of the regulations, the health system focuses attention on assistance, which generates a high social and economic cost to the country, without being able to implement effective health promotion and prevention programs 17.
The epidemiological indicators on cancer in the Municipality of Pasto, which covers rural and urban areas, were determined through the use of standardized methodology to maintain a reliable information system with adequate quality criteria for the collection and processing of data. That offer the possibility of comparison of the information at the national and international level, following the example of the Population-based Cancer Registry of Cali-Colombia, a pioneer in the implementation of a population-based registry 18.
For the analysis of the results, the data obtained are compared with those reported by population registries at national and international level. Under these criteria, in the analysis of the behavior of the most frequent types of cancer during the period 2013-2017, it is carried out based on the comparison with data published by the IACR for the Period 2008-2012, Epidemiology of cancer in Colombia and trend of incidence and mortality due to cancer in Pasto 1998-2012 8,10,19.
In men, gastric cancer continues to be a problem for the municipality, in the period 2008-2012 the incidence rate (APR) was 26.7 per 100,000 men/year and in the analysis period it was 28.0 per 100,000 men/year, values that when compared with the data reported by the IACR for the period 2008-2012, they are higher than the values of regions of Ecuador, such as Quito (21.2), Manabí (18.7), Guayaquil (14.0) and Cuenca (19.6), which due to their geographic location, ethnic, cultural and migratory affinity are related to the Municipality of Pasto. Regarding the incidence rates published by the Colombian population cancer registries, it is higher than that reported by the Cancer Registry of Cali (20.2), Manizales (20.3), Bucaramanga (17.1), Barranquilla (4.4) and Medellin (12.4) 19. However, in the trend analysis of cancer incidence in Pasto 1998-2017, a significant decrease in incidence rates was observed. Result that should continue to be monitored because when performing the analysis in the 2012-2017 period, an increase is observed that suggests revising the offer of services for diagnosis in the environment and other causes of probability of variations in the incidence trend (Figure 4).
Regarding gastric cancer mortality, the rate for the observation period was 24.2 per 100,000 males/year; this figure is higher than the one for the 2008-2012 period, which reported an ASR of 21.5 per 100,000 males/year 10; and to that published for Cali in the period 2011-2015, which was 14.4 males/year 20. According to data collected by Infocáncer for Colombia, stomach cancer continues to be the one that takes the most lives in the national territory (12%), which is explained by the country's geographic diversity, miscegenation, and Helicobacter pylori infection 21. In the Municipality of Pasto, although the decrease has been significant in the period 1998-2012, however, it still remains in the first place of mortality for males, which is probably due to the lack of attention to important aspects, such as those suggested by Triana et al. (22, referring to "screening, early diagnosis, regular monitoring of the evolution of the disease and timely treatment".
In the study on gastric cancer mortality trends carried out in Quito, Ecuador, during the period 1985-2013, they observed that although there has been a decrease in rates in the periods analyzed, these tend to remain stable and attribute the behavior to changes economic and social situations that the country has gone through 23.
In prostate cancer, in the period 2013-2017, a notable increase in incidence rates (61.9%) was observed when compared to the previous five-year period (2008-2012), going from a rate of 27.3 to 44.2 per 100,000 males/year; this figure is similar to that reported in other national registries, such as Manizales (64.1%), and Cali (65.4%) 19. However, there are differences in the behavior observed in the population cancer registry of Cali, where prostate cancer incidence rates increased significantly during the last 60 years, and rapidly between 1986 and 2002, and then reached a plateau around 2005. However, in the last decade, there has been a decrease 8,24 (Figure 4). In the analysis of the behavior of this type of cancer in Central and South America, the increase is attributed to the implementation of policies that guide detection, diagnosis and treatment, which emerged for Colombia in 2013 25, with the Ten-Year Plan for Cancer Control 2012-2021; as well as with the implementation of Resolution 247 of 2014 of the Ministry of Health and Social Protection of Colombia, which establishes the "report for the registration of patients with cancer as an information tool for the monitoring, follow-up and control of cancer patients”; as well as for the implementation of the clinical practice guideline (GPC, for its initials in Spanish) for early detection 26 in specialized health institutions, which is probably the case for the Municipality of Pasto.
Regarding mortality from prostate cancer, the estimate made for Colombia in the period 2007-2011 was 12.6 per 100,000 people/year 27. For the municipality of Pasto, the values for the five-year periods 2008-2012 and 2013-2017 were 12.2 and 12.8 males/year, respectively. These figures reflect a similar behavior between that of the municipality and the national one, as it has been observed in the trend of gastric cancer; this increase could be interpreted as another indicator of the epidemiological profile of cancer in the municipality, which is becoming increasingly similar to the observed behavior at the national level. Other evidence or indicators of this similarity between the local epidemiological profile and the national one is evident in the behavior of cancer in females.
With regard to lung cancer, the Municipality of Pasto maintains a relatively stable ASR of incidence in males (8.2 per 100,000 males/year), (Figure 4); which is lower than that reported for the period 2008-2012 for Manizales (10.3), Cali (13.9) and Bucaramanga (10.1) 19. With respect to mortality, as in incidence, the rate does not show substantial changes. For the period 2008-2012, it was 7.3; and in the period 2013-2017, it was 7.4 per 100,000 males/year. According to the analysis of the epidemiology of cancer in Colombia, lung cancer in the last two decades showed a decrease from 12.6 to 10.6 per 100,000 inhabitants in males; and 6.9 to 6.3 per 100,000 inhabitants in females. These results are attributed to the constant decrease of tobacco consumption in Colombia 21
In females, the analysis of the behavior of the most incident types of cancer with respect to the previous five-year period showed that breast cancer is in first place (ASR 35.1 per 100 females/year), following the trend observed at global level; however, according to the Globocan 2020 report, it is below the incidence calculated for Colombia (ASR 48.3) 28. Thyroid cancer (ASR 22.3 per 100,000 females/year) was in second place; followed by cervical cancer, with an ASR of 18.9 per 100,000 females/year.
It is important to note that breast and prostate cancer are hormone-dependent; and they require estrogen and testosterone for growth; and the probability of developing those tumors increases with age 29. Due to their high incidence, several countries encourage periodic screening tests, by mammography or digital rectal examination plus serum detection of Prostatic Antigen Analysis (PSA), respectively. This, added to the fact that diagnostic tests based on high-resolution images have increased their detection capacity in asymptomatic cancers with limited or null growth, has generated an increase in the reporting of their incidence 30. These policies have also been implemented at regional level; a fact that can be seen reflected in the results obtained for these two types of cancer during the five-year study period.
In the five-year study period, thyroid cancer, which has an ASR of 22.3 per 100,000 females/year, replaced cervical cancer in second place, which has an ASR of 18.9 per 100,000 females/year. Until the previous five-year period, cervical cancer occupied the first position as the most frequent cancer.
The increase in the incidence rates of thyroid cancer during the period 2001-2017 was also observed in the Manizales Colombia cancer registry, which went from 12.3 per 100,000 in females per year in the period 2003-2007, to 23.2 in the five-year period 2008-2012, which represents an average annual percentage increase of 13.4% 31. In the study carried out by Rossi et al., they report that thyroid cancer is one of the most diagnosed worldwide in females under 25 years of age. However, it is reported that there are some limitations for the analysis of over-diagnosis because there is no information about the stage, size of the tumor, histological classification and surveillance policies in each country, which could be the inputs to determine the real rates of incidence 32.
The analysis carried out in the study by Nan Li, et al, in the United States, argues that there are multiple causes for obtaining a significant change in the incidence rates of thyroid cancer, which may be related to the improvement in the diagnosis of the disease, access to the health system, and/or exposure to radiation, variables that should be investigated, especially for a context such as that of the Municipality of Pasto 33. This finding in the study period is important to advance research on this type of cancer that contributes to improving the quality of the RPCMP information.
Cervical cancer in the Municipality of Pasto, as observed in the 1998-2017 trend analysis, has decreased significantly, which can be explained by compliance in the locality with the country's regulations (Law 1384 of 2010); national public policies (Ten-Year Plan of Public Health - PDSP and Ten-Year Plan for Cancer Control in Colombia - PDCCC 2012-2021); and the Comprehensive Health Care Routes 34,35 in terms of promotion, specific protection, prevention, early detection, diagnosis, care and timely treatment of cervical cancer within the framework of the Global Strategy to accelerate the elimination of uterine cancer as a public health problem of the WHO 36, on which the municipality of Pasto has worked in recent years in the effective implementation of the set of public health measures for the primary prevention of cervical cancer: promotion of healthy lifestyles, and specific protection through vaccination against the Human Papilloma Virus (HPV), thus becoming one of the pioneers in Colombia in terms of agreements with health insurers for the implementation and compliance of HPV DNA screening adopted through the Health Promotion and Maintenance Route 34. Additionally, the municipality is promoting the approach and comprehensive care of users with preneoplastic lesions and cervical cancer under the care modality in the Cancer Care Functional Unit attached to the San Pedro Hospital Foundation (FHSP, for its initials in Spanish), in the Municipality of Pasto
Limitations and advantages
In recent years, there have been difficulties for the cancer registry in obtaining information on cancer diagnosis and treatment institutions due to the overload in the notification of data to other information systems, such as the High-Cost account, Individual Registry Provision of Health Services (RIPS), and the National Public Health Surveillance System (SIVIGILA). These difficulties delay the operation of the registry and the dissemination of epidemiological information in a timely manner.
It is necessary to mention that in this publication, the calculations of the crude and adjusted rates of incidence and mortality were made taking into account as population at risk, the latest intercensal projections adjusted by DANE from the 2018 census. These projections, compared with the previously available and that were used for previous reports, present a reduction of the population estimates; therefore, there may be an increase in the population risk of cancer in this five-year period, compared to the previous ones, as a result of methodological aspects.
On the other hand, the percentage of cases registered with microscopic verification, and cases with the death certificate as the only evidence, is similar to that recommended by the IARC for population-based studies 19.
Conclusion
The monitoring of cancer incidence and mortality indicators by population registries for five-year periods, plus the comparison of the behavior at national and international levels, provides the basis for evaluating the implementation of public policies through intervention strategies, especially those related with prevention and care. In addition, they are essential to strengthen research on this topic.











 text in
text in 



