Introduction
Cervical cancer is the fourth cause of cancer deaths in women worldwide 1. The incidence trend has been downwards, particularly in the developed countries, with rates lower than 6.5 per 100,000 inhabitants 2. However, it remains a concern in countries in Africa living in poverty; as well as in some other countries in Latin America and the Caribbean such as Peru, Bolivia, Paraguay and Haiti, with incidence rates higher than 30/100,000 3. Mortality rates are threefold higher in Latin America than in the United States and 4.
Colombia is in the group of countries with mean incidence rates, between 13.6 and 20.6/100,000, with downward trend, since in 1980 it showed rates greater than 35/100,000 2, which could be explained by better living conditions and increased coverage of better quality health services. The goal of reducing mortality by 6.8/100,000 for the year 2015 was already met in 2013, and it continues to decrease, thus placing the country bellow the average in South America, that lies by 7.1 per 100,000 2,5. It is reported that CC in young women is very rare 6, however, it should be underlined that in the United States 21 % of the new cases per year appear in women younger than 29 years 6. In Colombia, deaths due to CC and other uterine tumors are detected already in early ages; according to the mortality statistics presented by the National Statistics Department (DANE) in the last ten years 404 deaths in women aged between 15 and 29 years due to these two causes were reported, with rates ranging from 0.1/100,000 inhabitants in the group of 15 to 19 years old; up to 3.66/100,000 inhabitants in the group between 24 and 29 years old 7.
Risk factors are fully known. The human papillomavirus infection (HPV) is considered a necessary though not sufficient condition 8-11. Other risk factors are described such as precarious socioeconomic conditions, use of tobacco, initiation of sexual activity at an early age, having more than one sexual partner, sexual activity without using a barrier method, and early age at the first pregnancy 11,12.
In young women, the risk of contracting HPV is associated with an inadequate adaptive immune response, and, additionally, with physiological immaturity of the epithelium of the uterine cervix, since it is in much greater columnar type in transformation to squamous metaplasia, presenting an extensive ectopic area that, due to its fragility, can bleed, thus providing an entrance gate for the virus 13. Men play a very relevant role in the HPV due to their sexual behavior for they act as virus carriers, a particularly significant issue in countries whose male population customarily have multiple sex partners 14,16.
The first pregnancy at an early age (younger than 17 years) increases the risk of developing high-risk intraepithelial lesions or CC, even more when the patient is infected with high-risk HPV 17. It is believed that hormone changes due to pregnancy could intervene in the immune response against HPV, thus causing persistence or progression of the infection 12.
The use of tobacco has been associated with the risk of contracting CC, since in recurrent smokers the probability of this risk increases, even to double 18,19. Nicotine and carcinogens characteristic of tobacco have been found in the cervical mucus of smoking patients, supporting the hypothesis of a combined action of tobacco and HPV in progression and persistence of precancerous lesions, increasing the risk still further when the exposure to both agents occurs at early ages 20. It has been proved that the chemicals of tobacco act as carcinogens, producing a mitogenic effect that can later cause cell DNA damage and lead to Langerhans cell reduction and the decrease of immunomarkers in the cervical epithelium. This favors the loss of the capability of generating effective cellular immunity against HPV 21-23.
A correlation between CC and the presence of HPV with co-infections due to other agents in the vaginal tract, such as Herpes simplex type 2 and the Chlamydia trachomatis bacteria, has also been described 24. A relevant role of the latter in the development of CC is suggested, since it erodes the mucosa of the uterine cervix favoring the entrance of HPV and producing chronic inflammation that can interfere in the persistence of viral infection 25. In this sense, on the basis of results of a meta-analysis, Zhu et al. (2016) conclude that women with Chlamydia trachomatis infection have a higher cervix cancer risk 26.
As to the protecting factors, the Centers for Disease Control in the US ( CDC) sustain that the use of barrier methods, such as condoms, when properly and constantly used, can prevent infections with some germs causing sexually transmitted diseases such as human immunodeficiency virus, Neisseria gonorrhoeae, Chlamydia tracomatis, and Trichomona vaginalis; however, their efficiency in preventing HPV and Treponema pallidum is lower because condoms do not cover all skin areas that could be infected or exposed to contagion with these pathogen agents 27. The protector factors also include vaccination for preventing infection with HPV of high oncogenic risk 28. Another factor that is being studied as possible protector is male circumcision. A systematic review of published studies performed by Grund et al. concluded that there is highly consistent evidence of an association of circumcision of the male partner with the protection of their partners against cervix cancer and cervical dysplasias 29.
CC screening through cytology has been able to reduce mortality by half in developed countries where human resources and good coverage are available guaranteeing quality, for instance in Great Britain where a reduction of 70 % of deaths due to CC is attributed to its effects 30. In the last decades, DNA of HPV detection for the initial screening has been promoted since it has greater sensitivity and specificity; and cytology is being postponed for patients with HPV-positive result. When cytology is used as initial screening test, an additional HPV test is recommended for patients with low risk (LSIL) or undetermined intraepithelial lesion 31,32.
Age of initiation of screening varies from one country to another. In Canada it is 24 years of age 33; in Sweden, New Zeeland and Chile, 25 years 34,35; in Spain, between 25 and 30 years 36; in the United States it was recently reduced from 25 to 21 years old 37; in the European Union it lies between 25 and 30 years 38; and in Colombia it changed in 2018 from 30 to 25 years 31. The reasons for not performing a cytology in women younger than 21 years include lack of resources or competent staff, financial costs, unjustified emotional costs, cervix lesions due to the administered treatments, presence of false positive measurements, overdiagnosis, overtreatment 6,39; additionally, it is considered unnecessary since most LSIL lesions remit spontaneously in young women in approximately a two-year period 40,41. However, screening for ccis still performed in adolescents in some countries, regardless of the recommendations of the guidelines 42,43.
This study aims at describing the frequency of the exposure to cc risk factors and the results of the Pap test in a particular group of adolescent women experiencing critical, socially caused conditions which make them particularly vulnerable to be at risk and/or under damage both physically and psychologically. These conditions include school unattendance; break up of family relations; lack of stable housing; vagrancy in the streets; participation in drug micro-trafficking networks; use of illegal psychoactive substances, alcohol and/or tobacco; participating in criminal networks; human trafficking for sexual exploitation; and child prostitution networks. It should be noted that these conditions have been verified by child protection agencies which in fact have promoted that adolescents come under their care while a reintegration into society and their families is achieved.
The agency for child protection where these young females live is attached to the Instituto Colombiano de Bienestar Familiar, cytology is included in their routine admission clinical tests. Since this information was on file, it was considered important to analyze them collectively, for there are no studies published in literature describing the results of cytology screening in adolescents prolongedly and intensely exposed to risk factors.
Materials and Methods
his research is framed in a cross-sectional retrospective study based on information of all cytology reports performed in females aged between 11 and 18 years who were examined in the period between January 2011 to June 2016, coming from one of the institutions for adolescent social service in the north of the city of Bogotá, Colombia. The cytology report format included identification data; demographic and gyneco-obstetric information, as well as information on risk factor exposure of the patients, beside the cytology results according to the Bethesda classification.
Samples for the smear were collected by two cytohistologists with more than ten years of experience at a level IV university hospital; these were processed in the pathology lab of this hospital by Pap stain and read according the Bethesda classification criteria. All positive and 10 % of negative cases were reviewed and confirmed by pathologists of the pathology lab.
At the time, all samples were taken with the individual consent of the young women having previously been informed about the procedure, as well as with the consent of their legal representative, in this case, the child protection institution. To the females having not become sexually active who accepted the test, the smear was performed with cotton swab, without using speculum. Results were delivered through the direction of the institution since it is their legal representative while they are under protection. Women with high level squamous intraepithelial lesion and those who presented pathogenic vaginal flora were referred to gynecological care to continue studying the cases or to receive treatment.
Confidentiality was protected by excluding personal identification in the tabulation process and in the analysis. This work was performed in compliance with the ethical guidelines of the Declaration of Helsinki (2013) and the Resolution 8430 of 1993 of the Colombian Ministry of Health. According to the latter, this research was classified as without risk since it was a collection of anonymous documentary information. It was approved by the Human Research Ethics Committee of the San Jose Hospital in Bogotá, Record number 20 of October 26, 2016.
The findings were entered in Excel (Microsoft) version 2016, and were tabulated and analyzed with the Epi Info 3.5.1 program. Distributions of absolute and relative frequencies were used, measures of central tendency and dispersion were calculated.
Results
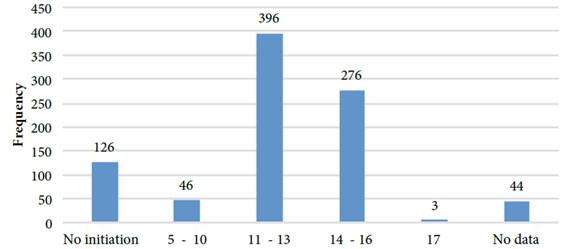
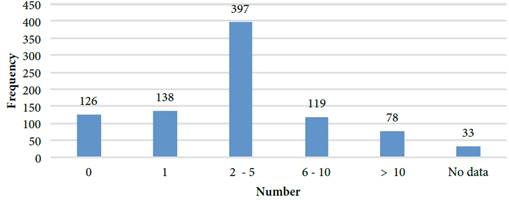
Among the obtained results, 891 reports were established in the research period. Average age of the young females was 15.24 years (sd: 1.33), in a range between 11 to 18 years. Initiation of sexual relations was between 5 and 17 years of age; 75 percentile corresponds to 14 years of age, and 25 percentile to 12 years (mean = 13, interquartile range = 2) (figure 1); 126 adolescents (14.1 %) expressed never having had sexual relations. The number of sexual partners varied between 0 and 120. The highest frequency laid in the interval between 2 and 5 (figure 2).
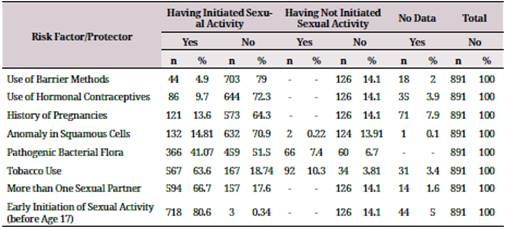
It is worth to mention that the contraceptive methods used were various; 75 % of the studied population declared that they used no contraceptive methods. Condoms were used by only 4.9 % of the females and 14.6 % (n = 121) declared having had at least one pregnancy. Considering the use of tobacco, 76.7 % (n = 659) habitually used tobacco before entering the child care institution, and, according to the caregivers, they reported smoking even 100 and more cigarettes day.
Regarding the risk factors/protectors of CC in marginalized adolescents it was confirmed that 48.5 % (n = 432) presented pathogenic flora in the sample, represented by Trichomona vaginalis, fungi consistent with Candida sp and suggestive of bacterial vaginosis. 15.3 % of the patients presenting pathogenic flora declared not having initiated sexual life (table 1).
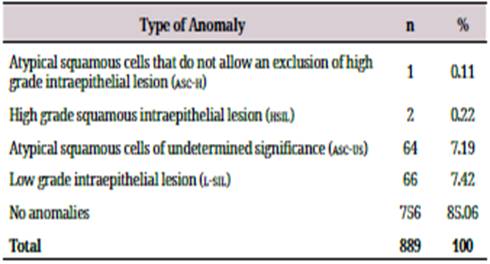
The cytology results according to the Bethesda classification showed anomalies in the squamous cells of 15.04 % of patients (n = 134). The frequency of HSIL was 0.2 % corresponding to two patients (table 2).
Discussion
This study presents the results of Pap tests and risk factors of CC in females younger than 18 years who have lived in critical social conditions. Exposure to CC risk factors was considerably high. The initiation of sexual life turned out to be at an earlier age than in adolescents of the general population, reported between 15 and 16 years old by other authors (44-47). The number of sexual partners to whom they have been exposed throughout their lives is high, although the median turned out to be lower than the one reported by Saleh et al. in Great Britain, who found that 78 % of adolescent females referred to colposcopy had had between 2 and 10 sexual partners 48.
The use of barrier methods was very low and coincides with the figure reported by Mendoza et al. in adolescents of Cali, Colombia, with just 5 % 47. In other countries, slightly higher frequency rates have been found, such as, for instance, 11.8 % in the study of Posso et al., and 14.7 % in the research of Del Río et al. 44. It is noteworthy that the number of previous pregnancies is low (14 %) considering that % of adolescent females did not use any contraception methods. Mendoza et al. reported previous pregnancy in 33 %, Saleh et al. found one previous pregnancy in 36 % of the adolescent females 47,48.
Regarding the anomalies in the Pap test, the frequency found in our study was the same as the one reported by Del Río et al. 44. By contrast, Mendoza et al. found only 7 % of presence of anomalies in adolescents of the general population in the city of Cali, Colombia 47. This difference may suggest a high frequency of HPV infection in the group of teenagers in critical social conditions.
For its part, frequency of high grade lesions was very low, as it is described in literature, and lies bellow what was reported by similar studies such as Del Río et al. with 3.2 %, Michala et al. with 2 %, and Mendoza et al. with 0.7 % 44,45,47,49,50.
High exposure to risk factors can be explained as a consequence of the critical social conditions under which these adolescents have lived since very early ages, thus favoring the presence of multiple factors simultaneously. A similar study conducted in Malaysia in adolescents of a child protection center who have lived in the streets found that adolescent females have also been exposed to initiating sexual relations at an early age; sexual relations without protection, with multiple partners, and, furthermore, with males with a high probability of being carriers of sexually transmitted diseases 51.
However, it appears that the preoccupation over the change in the sexual behavior ofthe adolescents is not only limited to these particular groups, but it concerns also to the population in general 52. Therefore, it is sustained that the risk of cervical infections, inflammatory processes, and precancerous lesions not detected before in young females is growing 53.
The American and Canadian guidelines do not recommend CC screening in females younger than 21 years of age since the risk-benefit relation is not favorable and because the frequency of lesions requiring medical treatment is much too low 54. However, experts of the American Society of Colposcopy and Cervical Pathology (ASCCP) in 2012 highlight that each country should adjust the guidelines according to the local conditions and suggest to consider health resources, training of healthcare workforce, adherence, and patients' expectations in each country 55. For its part, the Colombian Ministry of Health envisages within the frame of its guidelines the case of women younger than 25 years of age and orders: "It will perform an opportunity screening by cytology, based on the criterium and the assestment of previous history and risk factors performed by the physician or the nurse in order to justify its performance" 56.
The considerations outlined above suggest that teenage females with early and intensive exposure to CC risk factors could be included in screening programs following conservative and expectant protocols observing the evolution of lesions before initiating invasive procedures in the patient's uterine cervix.
On the other hand, gynecology consultations could be the opportunity for the adolescents to become aware of the implications of the exercise of sexuality, as well as to learn about risk factors, pregnancy prevention, prevention of sexually transmitted diseases (STDS), and the natural history of CC and how to prevent it. In this consultation, young females who have already initiated sexual relations should be assessed for the presence of STDS, they should also receive the corresponding treatment if they are test-positive, and subsequently entering a screening program for CC, if advised by the physician.
Finally, the particular characteristics of the adolescent females included in this study compels the health sector to be aware of the existence of serious social issues such as sexual exploitation of children, trafficking in narcotics and crime networks that operate taking advantage of hostile family and school environments. This environment, attractive for some adolescents, favors abuse and the consequent exposure to risk factors for multiple pathologies. Multisectoral and multidisciplinary intervention is essential to approach this complex problem area given the present and future consequences it entails