Introduction
Parathyroid carcinoma is a disease with a prevalence lower than 0.005% in the general population. In a meta-analysis of20 255 cases of primary hyperparathyroidism reported in the USA, parathyroid carcinoma was found in only 0.74% of the observed patients 1. Metastases are rare, but are found especially in lymph nodes and lungs when they occur. In turn, liver metastases are even rarer with very few cases reported in the literature. The only curative treatment is complete resection when the disease is localized, but in the case of metastatic disease, only palliative management can be provided for biochemical control. This paper reports a case of parathyroid carcinoma with hepatic metastasis as the only dissemination site, which was treated with hepatic intra-arterial embolization achieving an acceptable transient biochemical control.
Case report
74-year-old patient with a history of hypertension, mixed anxiety-depressive disorder, stage B heart failure and NYHA (New York Heart Association) functional class II/IV, who was diagnosed with primary hyperparathyroidism three months before admission to the clinic. She presented with moderate hypercalcemia (13.4 mg/dl) and very high levels of parathyroid hormone (PTH) (942 pg/mL -the normal upper limit is 65 pg/mL). Physical examination revealed a mass of 2 cm in the territory of the right lower parathyroid gland without palpable adenomegaly. A parathyroid scan with Tecnecio Tc-99m sestamibi revealed only a capture of the above-mentioned mass, while computed tomography (CT) of the neck and thorax with intravenous contrast did not show other alterations.
Initially, the patient was given intravenous fluids and a dose of 4 mg of zoledronic acid intravenously, which reduced calcaemia to 12 mg/dl by the tenth day of administration, and then underwent oncologic surgery (total parathyroidectomy + thyroidectomy + central emptying). However, hypercalcemia was persistent and increased later, yielding serum calcium values up to 14.6 mg/dl, which required a second dose of intravenous zoledronic acid 15 days after surgery, and low doses of oral cinacalcet (120 mg daily) due to poor tolerance.
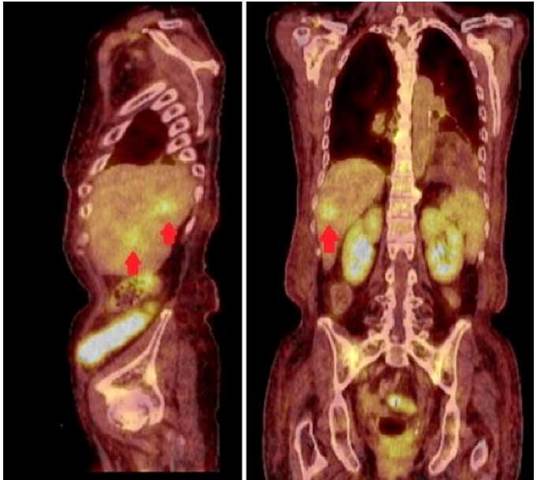
The lowest serum calcium value achieved with these interventions was 12.04 mg/dl. Multiple extension studies were performed, including neck ultrasound, cervicothoracic scan with Tecnecio Tc-99m sestamibi, and chest and abdomen contrast CT, which were all negative. A positron emission tomography (PET scan) with 18F-fluorodeoxyglucose (18F-FDG) was requested, and two hepatic metastases in segments V and VII were observed as the only site of disease persistence (Figure 1).
Source: Own elaboration based on the data obtained in the study.
Figure 1 Positron emission tomography with 18fluor-fluor-deoxy-glucose. In the sagittal section (left), the arrows point to two hypermetabolic lesions in segments V and VII of the liver. The coronal section (right) shows the largest lesion in segment VII of the liver.
A medical committee, in which a gastrointestinal surgeon and an endocrinologist also participated, discussed the management options for liver disease through surgical resection versus intra-arterial embolization. Considering the patient's opinion and the exposure to the lowest possible risk, intra-arterial embolization with polyvinyl alcohol microspheres in the right hepatic artery was chosen, and carried out without complications and excellent biochemical control after the intervention (Table 1). This allowed removing cinacalcet and zoledronic acid.
Table 1 PTH and serum calcium levels in the patient before and after hepatic arterial embolization of metastatic lesions (HAE).
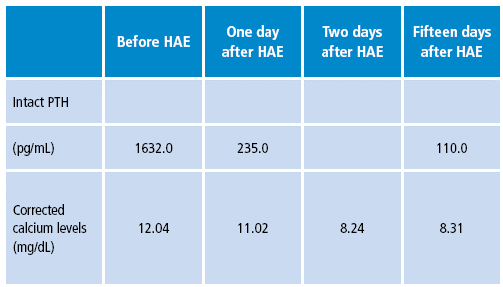
Source: Own elaboration based on the data obtained in the study.
Authorization for the publication of this case report was provided by the relatives of the patient.
Discussion
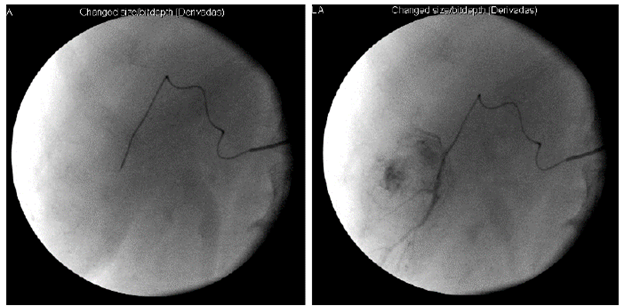
Parathyroid carcinoma was described for the first time in 1904 by De Quervain 2. This is a rare endocrine neoplasm, which accounts for less than 0.5% of all malignant endocrine tumors 3,4, and represents only 0.4% of all primary hyperparathyroidism cases in Western countries 5. (Figure 2)
Source: Own elaboration based on the data obtained in the study.
Figure 2 Hepatic arteriogram showing the vascularization of the two lesions before embolization (left) and the dye after embolization (right).
About 25% of patients develop distant metastases at some point, especially in lymph nodes (30%) and lungs (40%) due to lymphatic and hematogenous propagation. Less common sites include liver (10%), bone, pleura, and brain 6.
Morbidity and mortality are usually the result of hypercalcemia leading to neurological, cardiovascular, and kidney disease. An overall five-year survival rate has been estimated at 81% 4.
Preoperative diagnosis requires high suspicion based on biochemical and clinical parameters 7-10 such as severe hypercalcemia -generally higher than 14 mg/dl, which is considerably high for the parathyroid hormone (PTH)-, high preoperative levels of alkaline phosphatase, palpable cervical mass, tumor size greater than 3cm, bone involvement due to the disease (brown tumors), and development of nephrolithiasis.
To date, en bloc resection is the only potentially curative treatment in localized disease 3,11-13, but therapeutic options are reduced 8,13-15 in cases of recurrent or non-operative metastatic diseases, which are usually limited to controlling hypercalcemia, since antitumor therapy with chemotherapy or radiotherapy is not effective.
Likewise, percutaneous or laparoscopic radiofrequency ablation and selective arterial embolization of metastases are useful palliative alternatives that have been previously used in isolated cases 16.
Hepatic intra-arterial embolization interrupts the delivery of oxygen and nutrients to tumor cells by destroying them without compromising healthy liver tissue. This is a palliative option reserved for patients who are not candidates for surgical management or do not respond to medical management and have preserved liver function. This technique has been successfully used in other neuroendocrine tumors 17,18.
The main expected benefit in a patient with metastatic non-surgical parathyroid carcinoma is the reduction of the functional tumor mass to decrease parathyroid hormone secretion, obtain the consequent reduction of serum calcium levels, and improve secondary symptoms. However, such benefit is usually transient, and reports an average duration between 6 and 42 months in other types of tumors, mostly due to the formation of new blood vessels and the development of collateral circulation 19,20.
The effectiveness of intra-arterial embolization in hepatic metastases of a parathyroid carcinoma for tumor and biochemical control cannot be evaluated on a large scale, although success has been reported in similar cases 16, including cases of hypercalcemia in neuroendocrine tumors producing PTH-related peptide (PTH-rP) 21.
Conclusions
To date, this is the first case known and reported in Colombia in which a parathyroid carcinoma with hepatic metastases as the only dissemination site has been documented through PET-CT 18F-FDG and treated with hepatic intra-arterial embolization. Biochemical control of the disease was achieved, highlighting the potential role of this non-invasive therapy in special situations such the one exposed in this article.
This case was presented as a poster at the 13th Colombian Congress of Endocrinology, Diabetes and Metabolism in April 2015 22.














