Hospitals are complex workplaces, where biological agents circulate, which represent risk, latent or manifest, or even unknown. The handling of sharps, electrical materials and floors with smooth surfaces, are characteristics of the vulnerability of safety conditions.
Although a needle accident may result in infection, with a latency period of 90 to 180 days; exposure to radiation; contact with drug mists or biological aerosols produced by investigative activities may show symptoms years later.
Even after the efforts of infection control measures, some risks remain neglected, such as disrespect for parameters related to filtration, flow and air renewal.
Improvements have been observed, but autopsy are still "forgotten". These workplaces have functional criteria and specific demands.
Despite the number of autopsies has decreased, its value is undeniable in determining the cause of death, detecting clinically unknown lesions, collecting samples for analysis, confirmation or correction a diagnosis. Often it is the only way of conclude it 1-4.
Autopsy rooms are considered as one of highest risk areas of the hospitals 2-6. A priori the death-causing agent is unknown, so there is a potential occupational exposure risk 6,7. Unexpected situations or accidents are frequent, due to the great heterogeneity of manipulated materials. Scalpels, needles, bones fragments and teeth can result in percutaneous injuries. Organ manipulation increases exposure to body fluids and blood, use of instruments, hoses and saws produce aerosols contaminating items or allowing inhalation 7,8.
This study discusses the risks that can cause accident and/or contamination in autopsies, especially biological ones.
METHODS
Exploratory study focusing on systematic review as facilitator to build analyses of risk situations. This method summarizes researches results, aiming to understand a particular fact, based on previous studies, producing innovative conclusions 9. The procedures include a descriptive qualitative approach.
The guiding question was: what are the main occupational risks in autopsy rooms?
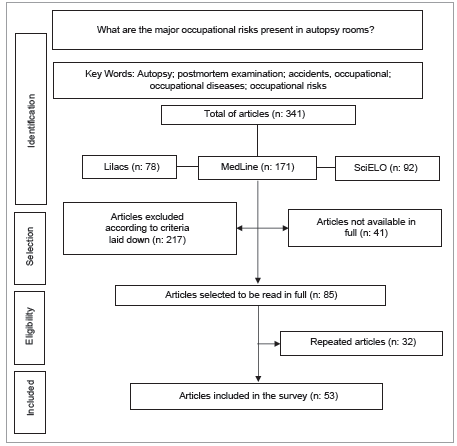
The search was conducted in databases: LILACS and MedLine, and in Scientific Electronic Library Online (SciELO) virtual library.
The Mesh terms and the boolean operators OR and AND were used, resulting in the combination: ("autopsy" OR "postmortem examination") AND ("accidents occupational" OR "occupational diseases" OR "occupational risks").
The search were developed in Jully 2018, and covered the period 2000-2017. Initially, the screening was done by titles and abstracts. All duplicates were removed. The studies were selected on the basis of the following criteria: a) language: Portuguese, English or Spanish; b) theme related to Biosafety in autopsy; and c) full text available. Abstracts, editorials, letters, articles with general content and without the specificity of autopsy were excluded. Then, the contexts were analyzed and integrated into sub-themes, according to the conceptual perspective of each context.
RESULTS
341 articles were found, which were analyzed for eligibility criteria for inclusion in the study. Duplicates and articles not available in full were removed, leaving 53 articles (Figure 1).
After reading, the articles were grouped by similarity and relevancy, into subtopics, to be discussed.
Occupational risks
Flavin 10 demonstrated that autopsy workers have a risk 10 times higher when compared to the population, and a 100-200 times greater chance of facing individuals without diagnosis, when compared to other healthcare professionals.
Most bodies sent to autopsy have no history or insufficient medical information. In addition, 20% to 30% of patients died in hospitals have important diseases or lesions not detected before death, but only during autopsy 3,4,11. Identification of the causes of morbidity and mortality, knowledge of the natural history of diseases, including previous outbreaks; can help to determine the risk represented by corpses 4,11. However, the occupation of the dead patient should also be considered. Drug addicts or prostitutes become more susceptible to violent or inexplicable deaths. But all patients should be considered suspected to contain pathogens, regardless of having a history of infection or belonging to a risk group 6,12.
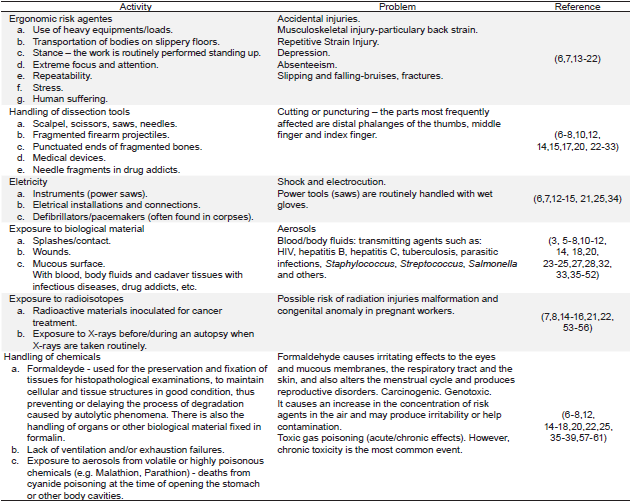
There are other risks during the autopsy. Table 1 shows the consequences of the risks identified.
Chemical agents
Formaldehyde, employed in the preservation of tissues, is the chemical most used in the autopsies. Despite high concentrations being required for the preparation of bodies, the concentration of formaldehyde in air depends on the contents of the fluid, kind of body, ventilation and work process. OMS studies 60 indicate concentrations above 1,2mg/m3 around the autopsy tables.
Formaldehyde is highly volatile and causes several symptoms, including ocular, mucosal and skin irritation 17,57,59. Long-term inhalation has been associated to an increased risk of developing cancer, especially lung cancer 14-17,57,59. OSHA limited occupational exposure to 0,75 ppm/8 hours and 2,0 ppm/15-minute periods 61.
Deaths from intoxication by organophosphates, like malathion, parathion, or cyanide, cause toxicity through inhalation, ingestion or dermal absorption. The greater risk is when the stomach is opened, as cyanide reacts with stomach acids and is converted into hydrogen cyanide, a highly volatile gas 12,15,18,22,35,60. Thus, they should be opened in biological safety cabinets. Personal items and contaminated clothing should be handled with gloves 7,36.
Neurotoxic gases used in acts of terrorism, like tabun, sarin, VX and soman; can penetrate slowly through gloves and rubber aprons and be absorbed by the skin. The bodies must be washed with water or alkaline solutions 25,37,38. The professionals must wear positive pressure protective suit, butyl or neoprene gloves; air purifying respirators with cartridges for organic vapors, since corpses can produce vapors. At ambient levels of 10 grams of agent/ m2 area, respirators can be used for until 24 hours 38.
Radioactive materials
Diagnosis or therapeutic procedures using radioisotopes before death can pose a risk to autopsy workers 8,16,21,54. Generally, diagnostic products have short half-lives and more penetrating emissions (gamma rays), while therapeutic and implant radioisotopes have longer half-lives and constitute risk for long time 53.
Thus, risk assessment should be performed to understand the extension of exposure from the dose administered to the patient, type of emission, radioisotope used and time of exposure 7. These will determine the procedures and protection equipment, as well as the safe release of the body for the funeral home. Bodies containing long half-life isotopes like Strontium-90 should not be submitted to autopsy and placed in sealed coffins 55. It is necessary to monitorize exposure and radiation levels. The instruments and the environment need to be decontaminated 8,14,15.
Electrical equipment and electronic devices
Electric equipment, like automatic saws, associated to the presence of water, increase the risk of shocks. Thus, preventive maintenance of equipment, insulation and grounding systems are important measures 7,14,15,25.
Another risk is implantable cardiac defibrillators used for tachyarrhythmias. The professionals may be hit by an electric discharge (25 to 40 Joules). This devise cannot be found before the autopsy, when found, the autopsy must be suspended until it is deactivated 12,34.
Ergonomic risk agents
Ergonomic risk agents are directly related to the routine 13-16. The use of heavy equipments and the movement of corpses 21,22 affect principally the assistants by physical effort. To avoid this, mechanical means should be used, like cranes or "transfer systems", which work as a conveyor belt between the stretcher and the autopsy table 21.
Non-height adjustable tables demands inadequate postures or use of platforms. When it is not possible to adjust the height, use lifting elements, with supports and non-slip surfaces, avoiding improvisations with boxes 17,20,21.
Seated position, repetitive and monotonous movements contribute to spinal problems, muscle pain, tendinitis and bursitis 13,17,18.
Factors like responsibility, focus, pressure and suffering of family members, view of burned or mutilated bodies, sounds, structural deficiencies, as frequent inadequacy of exhaust systems, which cause the presence of smells; cause tension, suffering, irritation, insomnia, increase of mental pathologies like fatigue, chronic stress and Burnout Syndrome 19.
Accident risk agents
Autopsy rooms have several accident risk agents. Emphasis given to inadequate physical arrangement, humidity and presence of power cables on the floor. It's recommended to use waterproof electrical outlets, suspended above the work area 21. A drainage system for waste water and fluids produced and the use of non-slip flooring will reduce falls, humidity and prevent the proliferation of microorganisms.
The use of sharps, scalpels, scissors, forceps, knives and saws can cause percutaneous injuries, exposing workers to infections 12,14,15,22,24-26. Babb 30 recorded accidental puncturing of hands during autopsies, 38% among assistants and 12% among forensic pathologists. About 67% were inflicted on the distal fingers, the index fingers and the middle fingers of the non-dominant hand.
The corpse may contain perforating objects from a previous medical intervention not documented, like filters in the vena cava 31. There are reports of HIV contamination after accidents with fragments of needles in autopsies of subcutaneous intravenous drug user 17,27. There are other infections that can be transmitted by direct inoculation, like tuberculosis, blastomycosis, hepatitis B and C, rabies, tularemia and some types of viral hemorrhagic fever 6,7,23,25. Radiologic examination helps to locate these fragments.
Biological agents
Discrepant diagnoses are common and a substantial number of infections are detected only after postmortem analysis, even the most common such as pneumonia, sepsis, meningitis, peritonitis and endocarditis 3,5. 80% of coexisting infections are ignored; and even when diagnosed during life, the autopsy reveals that disseminated infections, such as bacterial endocarditis and acute pyelonephritis are underdiagnosed 62.
The presence of asymptomatic diseases without morphological evidence during autopsy poses a risk (50) and shows the importance of investigation the cause of death. The diagnosis will provide information, facilltate the contact management, infection patterns, control of outbreaks and identification of new infections and threats 3,11.
Autopsy professionals are exposed to pathogens transmitted by direct or indirect contact, by aerosols or by injuries and accidents caused by sharps 7,8,10,23,28,29,32. This risk is exacerbated by high seroprevalence of certain pathogens.
Exposure to aerosols is important in the autopsy room. Aerosols are particles smaller than 5 pm, remaining suspended in the air for long periods of time, or carried away by air and inhaled. These particles pass through the respiratory tract, reaching the pulmonary alveoli 8,12,33. However, particles with diameters greater than 5 pm (droplets) also pose a risk. They are heavier and reach smaller distances, being restricted to the autopsy table.
Aerosols are generated by fluid aspirators and hoses that spray water over tissues. The saws applied to the bones produce large amounts of dust and aerosols, distributed throughout the room and remain in the air for up to 1 hour, within a radious of up to 15 m from the saw, despite the ventilation system 33. However, even compression and dissection of the lungs using autopsy tools can produce aerosols and droplets 12.
Nonetheless, infection is a complex multifactorial process, requiring the presence and exposure to pathogen, and a susceptible host. Susceptibility is related to aspects which determine the individual's resilience 63. Pathogens have parameters to be analyzed, including virulence, transmission mode, drug resistance, stability, endemicity, availability of treatment and effective prophylactic measures. Regarding the activity, the concentration, volume of the manipulated material and the possibility of aerosol formation need to be assessed 63. This analysis will determine the risks and protection and containment measures 23.
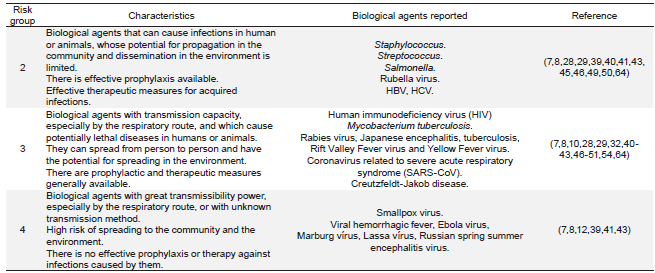
Biological agents are classified into 4 risk groups (RG), increasing in degree of protection and containment required. RG3 and 4 agents have respiratory transmissibility power, and therefore pose greater risk 9,23. Table 2 shows the RG of etiological agents of diseases most frequently reported.
RG1 agents do not cause disease in healthy adults and their absence is justified by the fact that the normal flora of a healthy person is composed of RG2 agents.
DISCUSSION
This study identified the following pathogens: M.tuberculosis, hepatitis virus, HIV and prions responsible for transmissible spongiform encephalopathies. All of them maintain infectivity after death 28,40-42,64, cause diseases often asymptomatic, with no morphological evidence at autopsy.
a) Mycobacterium tuberculosis
Tuberculosis is most prevalent among HIV-positive individuals, prison inmates, intravenous drug users, and ethnic groups in countries with high TB rates. The emergence of multidrug-resistant strains emphasizes the importance of risk assessment.
It is not uncommon cases of active tuberculosis be identified only after autopsy. The presence of nonspecific symptomatology, cost-effectiveness of diagnostic tests and early death, are the most frequent causes of undiag-nosed tuberculosis 54.
A study in the USA, from 1985 to 1988, identified 5,1% of cases of tuberculosis during postmortem 48. This data may explain the higher incidence of tuberculosis among autopsy workers (10%) compared to pulmonologists (4%) and other medical specialties (1%) 10,41. 90% of cases of occupational tuberculosis occurred due to aerosolized bacilli12.
Nolte 7 described an outbreak of multidrug-resistant tuberculosis, attributed to positive pressurization of an autopsy room, where exhausted air circulated through the facility. However, transmission of tuberculosis can also occur in facilities with adequate pressurization and exhaust systems, but lacking proper personal respiratory protection.
Sterling 45 showed the presence of viable bacilli 24 to 48 hours after the embalming of a body, demonstrating the potential for aerosol transmissibility during formalin-fixed tissue dissection.
Another occupational infection is tuberculosis verrucosa cutis, which accounts for 5-10% of cases of infections among autopsy workers 44. The bacillus can be introduced into the skin through previous lesions or punctures.
It is advisable to introduce 10% formalin into the lungs through the trachea, as well as immerse the organs in it for 24 hours, after evisceration and before dissection. All unfixed tissues need to be manipulated in a biological safety cabinet. Bodies not yet fixed must not be handling. Sputum, pus, tissue and urine samples must be manipulated as little as possible, to avoid splashing and aerosol formation. The instruments used must be sterilized, preferably by physical means 7. Other recommendations include restricting the movement of people in the room and the use of hand saws in place of power equipments (46). Biosafety measures should include engineering and administrative controls, ventilation recommendations (negative pressure and exhaustion by HEPA filters), respiratory protection with N95 masks and post-exposure chemoprophylaxis.
b) Human immunodeficiency virus
The risk of seroconversion of autopsy personnel after contact with HIV positive blood is low (0-0,42%) 12,14 and most documented cases occurred after injuries caused by sharps, especially needles 6,51. This percentage may be underestimated when compared to the risk associated with deep accidental scalpel injuries. Post-exposure seroconversion will depend on the patient's viral load, inoculated volume and worker's susceptibility 6,51. The viral load on CD4+ T cells in the peripheral blood is higher during the acute phase and in the late stages of the disease. Thus, autopsy titers may be higher than in living patients 12.
Studies have demonstrated the viability of the virus in blood, pleural and pericardial fluids of cadavers stored at 20°C after 16% days 6,39. It was isolated from cranial bone, spleen, brain, cerebrospinal fluid, blood, bone marrow and lymph nodes during autopsy in bodies stored at 6°C, after five days from postmortem 12,23. In 2006, HIV was detected in corpses six days after a tsunami in Indonesia 23.
Surfaces and materials should be decontaminated with 0,5% sodium hypochlorite, 1% glutaraldehyde, or 3% hydrogen peroxide. However, besides corrosive, sodium hypochlorite reacts with formaldehyde to produce dichloromethyl ether, a powerful carcinogen 12.
c) Hepatitis B and C
Viral hepatitis is the most frequently disease reported 6, but there is a lack of studies about the prevalence of occupational infectious.
Hepatitis is universally distributed. Its prevalence coefficients are directly related to the populations at risk (drug users, prostitutes, individuals with tattoos, transplant patients, etc.) 6,7,39,40,41,44.
Gharehdaghi 40 showed a 15,5% risk of HIV, HBV and HCV contamination in the handling of bodies (2,6%, 3,8% and 9%, respectively). These data are important because HBV is about 100 times more transmissible by blood and aerosols than HIV 6. HBV is highly infectious and its transmission can occur after exposure to infected blood in extremely small amounts. However, the risk of occupational acquisition is low, due to the routine vaccination. Nonetheless, there is no immunoprophylaxis for HCV; although, the risk of transmission after percutaneous exposure (2,7-10%) is lower than that of hepatitis B (30%) 6,25,46.
Data show that 3% of reported cases of acute hepatitis C are associated with needle puncture 6,8. Among autopsy professionals who have suffered perforations, the chance of acquiring HBV infection is 5%; however, if the blood contains the HBsAg antigen, the risk may be higher (up to 30%)29.
HBV persists on surfaces at room temperature for 7 days, allowing for indirect transmission 6.
Autopsy helps to clarify the cause of death, vital for epidemiological surveillance to detect emergencies, diagnose isolated cases or during disease outbreaks.
Public health is currently in crisis, reflecting on the quality of facilities and services. Therefore, it is important to implement biosafety principles to prevent, reduce, eliminate and control risks, which could compromise public health, the environment and thus improve quality. Therefore, it is necessary to break requires breaking paradigms, such as changes in habits and culture.
In planning autopsy areas, physical space should be an essential aspect as it contributes to ensuring safety. This areas needs to be subdivided according to minimum safety standards. The first of them, "clean areas", includes offices and reception spaces. The second is a "transition area" made up of passage zones, such as corridors; access locker rooms, where personal protection equipment is stored; sanitary facilities; storage areas for bodies and parking of body transportation vehicles. The last, "dirty area", composes of: postmortem room, waste storage; decontamination and cleaning areas. In addition, a risk assessment is important for determinate the Biosafety Levels (BSL). BSLs can be applied to autopsy, as they guide the safe management of biological agents. There are 4 levels, but since there are no RG 1 agents in autopsies, the levels begin at BSL2. BSL2 provides protection for most blood-borne agents where universal precautions are required for routine operations. BSL3 provides protection against potentially airborne agents, which can cause serious or potentially lethal diseases. BSL4 provides protection against exotic agents, with unknown pathogenic potential, and cause fatal diseases, for which there are no vaccines or treatments.
In Brazil, 72% of the etiological agents of notifiable diseases are RG2, 19% are RG3 and 9% are unknown agents 65. These data corroborate the results of this study, showing the importance of adopting universal precautions during when handling all cadavers. However,it is important to evaluate each autopsy, and choose less hazardous methodologies, such as the diagnosis of viral hemorrhagic fevers using a skin fragment, or diagnosis of SARS using immunohistochemical methods or molecular biology ♠