Introduction
Since the late 1960s, endoscopic retrograde cholangiopancreatography (ERCP) has been described as a new technique for diagnosing biliopancreatic diseases1. A few years later, papillary sphincterotomy was described for bile tract lithotripsy removal2,3, specifying this procedure’s diagnostic and therapeutic nature.
Although this endoscopic procedure is currently widely used to treat multiple pathologies such as choledocholithiasis or benign and malignant biliary stenosis, complications are not excluded, occurring in up to 15% of the procedures4 -post-ERCP pancreatitis is one of the most frequent complications.
There are multiple risk factors for each complication. However, a failed or difficult biliary cannulation is a common factor for these adverse events5 and is also closely related to the anatomy of the duodenal papilla.
Several duodenal papilla classification systems have been proposed over the past decade. These systems have been used to predict cannulation success, complication rates, and the need for more advanced access techniques6,7. However, so far, only the Haraldsson et al classification system (Figure 1), which classifies the duodenal papilla into 4 types, has been subjected to an intra- and inter-observer discordance study8, thanks to its simple classification scheme that admits within its types a wide variety of duodenal papilla presentation. Thus, any papilla can be categorized based on this classification. Additionally, this system is useful for predicting difficult biliary cannulation for experienced endoscopists and beginners, as it shows that types 2 and 3 papilla are the most difficult to cannulate9.
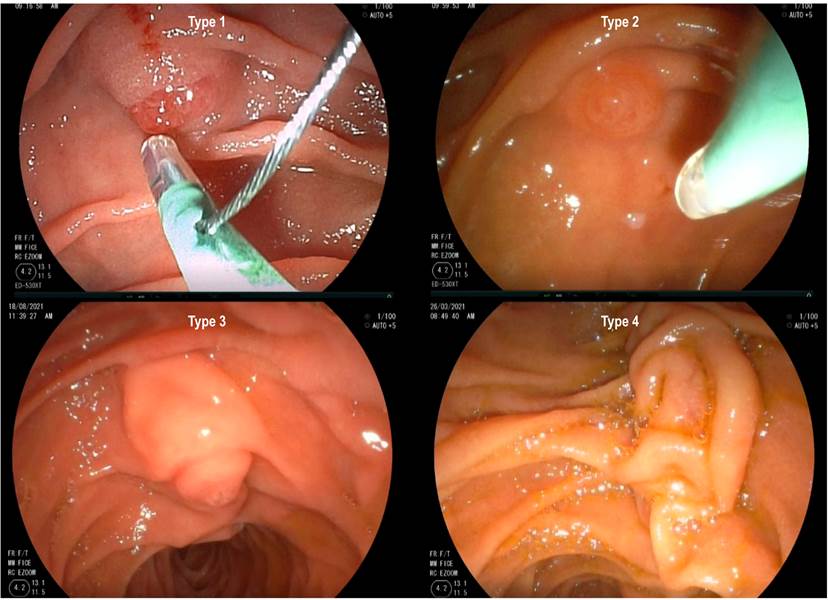
Figure 1 Types of duodenal papilla8. Type 1: “regular” appearance, without specific distinctive characteristics. Type 2: flat, with a diameter ≤ 3 mm. Type 3: protruded, pendulous, with prominent infundibulum. Type 4: ridged or “creased”. Adapted from: Haraldsson et al. United Eur Gastroenterology J. 2017;5(4):504-10. Including images from the research group.
The European Society of Gastrointestinal Endoscopy (ESGE) defines difficult cannulation when one or more of the following criteria is present: more than 5 contacts with the papilla while attempting to cannulate it, more than 5 minutes spent attempting to cannulate it after localizing the papilla, and more than one pancreatic duct involuntary cannulation or opacification10.
This study aims to identify the relationship between the morphological characteristics of the duodenal papilla -according to the Haraldsson et al classification system and post-ERCP complications in patients treated in a gastroenterology unit of a referral hospital in Lima.
Materials and methods
A prospective and analytical study that included 138 patients who underwent ERCP at Hospital Guillermo Almenara Irigoyen in Lima, Perú, a referral hospital where approximately 500 ERCPs are performed per year, according to the system registry. This was a convenience sampling. Patients who signed informed consent and agreed to be part of the study were involved until the sample size was completed. On the other hand, patients with ERCP and previous sphincterotomy, with anatomy altered by previous gastroduodenal surgery, periampullary neoplasia, and pregnant women were excluded. Endoscopic and clinical data were collected for statistical analysis using central and association tendency measures such as odds ratio (OR), with a 95% confidence interval (CI). The association between the variables was measured with the Chi-square test, and a p < 0.05 value was considered statistically significant.
The equipment used was Olympus® and Pentax® video duodenoscopes. The materials for cannulation were Endo-flex® sphincterotomes, Endo-flex®, and Endo-med® balloons and extraction baskets. The x-ray equipment was a C-Arc from General Electric®, and the electrosurgical equipment was from ERBE®.
The patients signed an informed consent form in compliance with the ethical principle of autonomy. All procedures included clear therapeutic medical instructions in compliance with the non-maleficence principle. A local ethics committee approved the study.
Results
Of the 138 patients, 93 (68.42%) were females, and 45 (31.58%) were males. The mean age was 51.46 years (95%CI: 48.78-54.14). The most frequent type of papilla was type 1 with 81 patients (58.7%), followed by type 3 papilla in 40 patients (28.9%), and type 4 papilla was the least common, with 6 patients (4.35%). Type 4 papilla required, on average, a longer cannulation time (6.83 min), while type 1 papilla required a shorter cannulation time (2.93 min). Although these results were not statistically significant, no differences were found in cannulation attempts and unintended passage to the pancreatic duct between the different types of duodenal papillae.
A statistically significant relationship was found between papilla type and precut performance (p = 0.0001). Precutting was performed in 18 patients (13.04%) and was more frequent in type 4 papilla (33% of the cases of this type of papilla) and type 3 (30% of the cases). The analysis of each type of papilla showed that type 1 had an OR = 0.11 (CI: 0.03-0.39); type 2, an OR = 0.65 (CI: 0.08-5.38); type 3, an OR = 6.57 (CI: 2.26-19.11), and type 4, an OR = 3.63 (CI: 0.61-21.41) (Table 1).
Table 1 Characteristics of the population according to the type of duodenal papilla
| Characteristics | Type of papilla | p value | ||||
|---|---|---|---|---|---|---|
| Type 1 | Type 2 | Type 3 | Type 4 | |||
| Median age (years) (95% CI) | 52,89 (49,42-56,36) | 53,68 (44,17-63,19) | 48,11 (43,04-53,18) | 50,5 (38,18-62,82) | 0,4615 | |
| Gender | Female, n (%) | 53 (65,43 %) | 7 (63,64 %) | 30 (75 %) | 3 (50 %) | 0.554 |
| Male, n (%) | 28 (34,57 %) | 4 (36,36 %) | 10 (25 %) | 3 (50 %) | ||
| Average cannulation time (minutes) | 2,93 | 3 | 3,67 | 6,83 | 0,1202 | |
| Average cannulation attempts | 2,94 | 3,18 | 3,33 | 3,83 | 0,3955 | |
| More than 1 passage to the duct of Wirsung | 9 (11,11 %) | 0 (0 %) | 5 (12,5 %) | 1 (16,67 %) | 0,645 | |
| Precut, n (%) | 3 (3,7 %) | 1 (9,09 %) | 12 (30 %) | 2 (33,33 %) | 0,0001 | |
| Total, n (%) | 81 (58,7 %) | 11 (8,05 %) | 40 (28,9 %) | 6 (4,35 %) | ||
CI: confidence interval.
Type 1 duodenal papilla was associated with less difficulty during cannulation (OR = 0.42; p = 0.02) compared to the other types and was statistically significant. The other types of papillae showed more difficulties during cannulation. Overall, no association was found between papilla type and difficult cannulation (p = 0.123) (Table 2).
Table 2 Papilla type and difficult cannulation
| Papilla Type | Difficult cannulation | OR (95%CI) | p = 0,123 | |
|---|---|---|---|---|
| Yes | No | |||
| 1 | 19 (23,46 %) | 62 (76,54 %) | 0,42 (0,20-0,88) | 0,02 |
| 2 | 4 (36,36 %) | 7 (63,64 %) | 1,29 (0,36-4,66) | 0,698 |
| 3 | 17 (42,5 %) | 23 (57,5 %) | 2,05 (0,95-4,42) | 0,066 |
| 4 | 3 (50 %) | 3 (50 %) | 2,3 (0,44-11,89) | 0,308 |
CI: confidence interval; OR: odds ratio.
The overall rate of post-ERCP pancreatitis in our study was 2.9%. In the analysis for each type of papilla, type 1 showed an OR = 0.23 (0.02-2.22); type 2, an OR = 4.43 (0.39-43.48), and type 3, an OR = 2.53 (0.34-18.59) for post-ERCP pancreatitis, although no statistical significance was obtained (p = 0.376).
The bleeding rate was 1.45%, and the perforation rate was 0.72%. Type 2 reported a higher complication rate with 9.09% of pancreatitis and 9.09% perforation. In the general analysis, perforation presented a statistically significant association with papilla type (p = 0.009). Still, the risk for each type could not be determined due to the lack of events in some types of papillae (Table 3).
Discussion
Findings showed that the duodenal papilla type is significantly associated with post-ERCP perforation. Type 2 showed higher rates of pancreatitis (9.09%) and post-ERCP perforation (9.09%). There was an association between the type of duodenal papilla and precutting, and it is more likely to be performed in types 3 (OR = 6.57) and 4 (OR = 3.63).
Over the last few years, several studies have been published comparing different difficulty levels of biliary cannulation according to the duodenal papilla morphology17,19,20. However, these studies differ in the type of classification. They are based on different parameters such as the Viana classification, which divides the type of papilla according to the parameter combinations such as the papilla shape, the oral segment protrusion of the papilla, the number of transverse folds, and the presence of a diverticulum7. Other studies classify the type of papilla according to the oral protrusion and papilla pattern11. Moreover, other simpler and more classic studies, such as Canard’s classification12 and according to the primary characteristic of the duodenal papilla (large, small, and protruded)6, are different from the classification proposed by Haraldsson et al which is the only one that has undergone a discordance intra- and inter-observatories study so far.
A retrospective study published in China in 2020 reveals that type 2 and 3 papillae require more time for cannulation and have a higher failed cannulation rate (12% and 11.1%, respectively) compared to type 1 and type 4 papillae (1.7% and 6.25%)13. Conversely, our results show that the types of papillae requiring more cannulation time were type 4 (6.83 minutes) and type 3 (3.67 minutes), although it was not statistically significant.
In 2019, Haraldsson et al found that type 2 and 3 papillae were more difficult to cannulate (OR = 1.89 and 1.61, respectively) compared to type 1 and 4 papillae. In addition, the median cannulation time was significantly longer for type 2 papilla (269 seconds) and type 3 papilla (245 seconds), both with a p < 0.05 value, compared to type 1 papilla (139 seconds)9. In Canada, a retrospective study was conducted using the Haraldsson classification and found that the OR for difficult cannulation was higher for type 2 (AOR = 3.73; 95%CI: 1.28-10.84) and type 3b (AOR = 3.97; 95%CI: 1.76 to 8.99). Additionally, these types were associated with post-ERCP pancreatitis (AOR = 7.28 and 4.25, respectively)14, unlike our study, which found that only type 1 papilla was less difficult to cannulate (OR = 0.42). However, we found no association between the type of papilla and difficult cannulation. Meanwhile, the average cannulation times shown in our study were higher, especially for type 4. We found no association between the type of papilla and post-ERCP pancreatitis.
On the one hand, the overall post-ERCP adverse events rate was higher in type 2 papilla (18.18%), while no adverse events were observed in type 4 papilla in our study, contrary to what Balan et al presented, they obtained a significantly higher rate for patients with type 4 papilla12. Conversely, in his multicenter study, Canena concluded no significant difference in the adverse events rate between the different papilla types. However, they used a different classification system7.
Pancreatitis was the most frequent adverse event, with a higher rate in type 2 papilla (9.09%). This finding was similar to what Chen et al found. Their study showed that type 2 papilla had the highest percentage of post-ERCP pancreatitis (20% compared to 6.78% for type 1; 1.59% for type 3, and 6.25% for type 4; p = 0.020)13. In 2019, Haraldsson et al also reported a higher rate of pancreatitis for type 2 papilla (9.4%), but with no significant differences compared to the other papillae9. In turn, Mohamed et al used Haraldsson’s classification with a modification: they divided type 3 papilla into 3a (protruding or bulging) and 3b (pendulous or redundant), and separated papillae associated with periampullary diverticula into type D. For them, pancreatitis was also the most frequent adverse event, it was significantly higher in type 2 and 3 papillae14. Another study conducted in Shanghai considered 5 types of papillae, where findings showed that pancreatitis was also the most frequent adverse event, showing the highest rate for papillae classified as flat, equivalent to type 2 (6.3%)16.
Our study did not observe acute cholangitis as a complication, an adverse event reported in other studies with rates between 0.6% and 1.75%9,13,15. We found a statistically significant association between papilla type and fistulotomy-like precutting as a rescue technique in case of failed conventional cannulation, and it was more frequent in types 4 (33.33%) and 3 (30%). The cannulation success rate, including fistulotomy, was 100%, similar to that of Wen et al, who chose the precut according to the morphologic characteristics of the papilla and the entry into the pancreatic duct. They recommend the fistulotomy for a protruding papilla (type 3)13. Different studies found a 100% cannulation success rate for fistulotomy-type precut18,21.
Conclusions
The duodenal papilla morphology can be classified using the system proposed by Haraldsson et al. The duodenal papilla type is associated with post-ERCP perforation. Type 2 papilla has higher rates of pancreatitis and post-ERCP perforation than other types.
The type of papilla is associated with advanced cannulation techniques such as pre-cutting, and types 3 and 4 are more likely to be used. Although, due to the low number of type 4 papillae affecting statistical analysis, these results should be taken with caution.











 texto en
texto en 



