Introduction
Tuberculosis (TB) is an infectious disease caused by My cobacterium tuberculosis which primarily affects the lungs and is one of the 10 main causes of mortality worldwide. An estimated 1.4 million people died from TB in 2019, although it is one of the curable and preventable infectious diseases 1-3. In developing countries, the incidence of TB has risen significantly, due to the growing number of patients with human immunodeficiency virus (HIV) coinfection, as well as the increased use of immunosuppressive therapy in the context of different diseases 4,5.
Intestinal tuberculosis (ITB) is one of the most frequent causes of extrapulmonary TB, with almost 90% of cases located in the ileocecal region 6. The gastrointestinal signs and symptoms vary and are vague, mimicking different types of inflammatory bowel disease (IBD), malignancies or gastrointestinal infections. Normally, the location of ITB is not well described, and therefore it is difficult to determine the incidence of the disease, as most patients with ITB are asymptomatic 5,7. The objective of this paper is to present the clinical signs and symptoms and endoscopy findings of a patient with ulcerative colitis secondary to tuberculosis and describe how we arrived at the diagnosis of this disease.
Clinical case
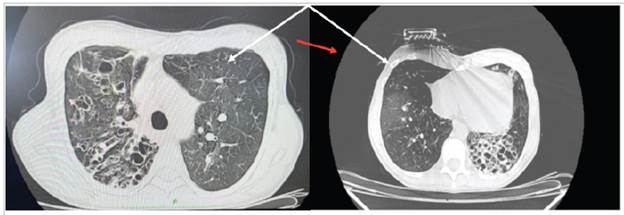
We present the case of a 42-year-old man with a three-month history of colicky abdominal pain in the right iliac fossa with a 6/10 intensity, associated with nausea, episodes of vomiting and a sensation of an intraabdominal mass. At the same time, he reported a 3 kg weight loss, and denied fever or other symptoms associated with the clinical picture. He had a history of rheumatoid arthritis since 2002, initially treated with methotrexate, prednisolone and calcium, and then for a year with etanercept. He had no history of allergies and reported a surgical history of phacoemulsification in 2010 and clavicular osteosynthesis in 2015. On physical exam, he was tachycardic (HR 104 bpm, RR 19 Bpm, T 36.8°C, O2 sat 97%, weight 55 kg, height 160 cm). He had no scleral jaundice, a moist oral mucosa, normal chest expan sion and well-ventilated lungs. The abdomen was soft and painful on palpation of the right iliac fossa, with no signs of peritoneal irritation, and no palpable masses at that time. Blood chemistries were drawn which were within normal ranges (albumin 4.2 gr, negative carcinoembryonic antigen, negative alpha-fetoprotein, creatinine 0.6 mg/dL, complete blood count: leucocytes 8,000, 60% neutrophils, Hgb 11.5 g/dL, Hct 34.5%, platelets 180,000, BUN 20 mg/dL). An abdominal ultrasound reported concentric wall thickening of the ileocecal valve; a subsequent colonoscopy showed a tumor-like lesion in the ascending colon, with the etiology to be determined by biopsy (Figure 1, A, B). Following this, the hematoxylin and eosin-stained pathology showed granulomas in the colonic mucosa, and special Ziehl Neelsen staining showed Mycobacterium tuberculosis granulomas, with a final diagnosis of active chronic granulomatous ul cerative colitis due to Mycobacterium tuberculosis (Figure 2: A, B, C).
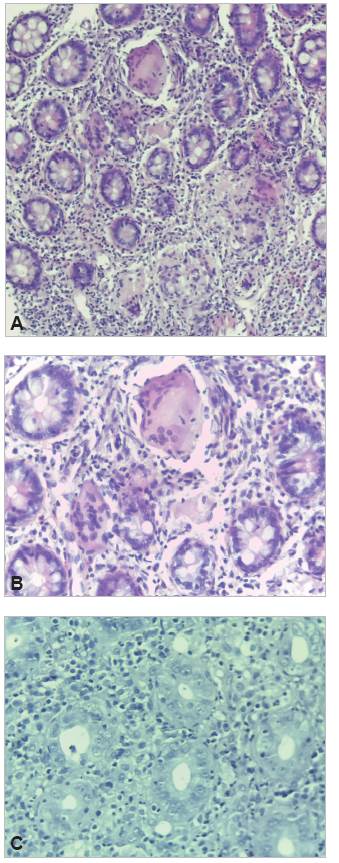
Figure 2 (A) hematoxylin and eosin (HE) granulomas in the colonic mucosa. (B). HE multinucleated giant cells in the colonic mucosa. (C). Ziehl Neelsen (ZN) staining in the colonic mucosa.
The patient was treated for tuberculosis with isoniazid, pyrazinamide, rifampicin, and ethambutol for six months. He progressed well after this.
Discussion
Mycobacterium tuberculosis infection in the gastroin testinal tract is a rare manifestation of extrapulmonary tuberculosis, with a predilection for the ileocecal region, in an average of 44-93% of cases, as the mycobacteria have a fatty capsule that is indigestible and prevents its early release in the gastrointestinal tract, which is why this infection is uncommon in the proximal zones 7. The mycobacteria have a special affinity for lymphatic tissue, with the ileocecal valve being the most important since it contains numerous lymphatic chains. As the tuberculoma grows, the intestinal wall thickens and forms small papillary invaginations in the mucosa 5. Extrapulmonary TB occurs in 20-25% of cases, according to Ramírez et al.'s report 8, and the prevalence of ITB lies between 3 and 5%. Our patient had one of the risk factors for ITB, which was the use of anti TNF, although HIV infections, corticosteroids, malignancies, diabetes mellitus and chronic kidney failure are also described, according to Perise et al.'s findings 9. Regarding the local epidemiology, the data are unclear as far as the prevalence of the disease and the mortality of extrapulmonary TB presentations, as ITB often cannot be diagnosed promptly 7,10.
The clinical signs and symptoms are nonspecific and the time ranges from 1 to 12 months; symptoms include abdominal pain, fever and fatigue. Weight loss and nocturnal diaphoresis are important symptoms of TB; a study by Zhao et al. reported that the most common manifestations were ascites and nocturnal diaphoresis, while Makharia et al. re ported chronic diarrhea, blood in the stool, perineal disease and manifestations outside of the digestive tract 11,12.
In light of the above, the diagnosis focuses on clinical suspicion and its associated risk factors, including taking a history, diagnostic imaging and histopathology, after ruling out more frequent diseases like Crohn's disease, ulcerative colitis, and lymphoma, among others. This was done ap propriately in the reported patient, as a biopsy was taken of the ascending colon mucosa via colonoscopy 13. The treatment for ITB is the same as for pulmonary tuberculosis, with a duration of six months 13. Follow up and response to treatment tends to be confirmed with decreased symptoms after two weeks of antitubercular treatment and resolution of the lesions found on endoscopy three months after begin ning treatment 9,14.
We described a case of tuberculosis in the ascending colon, a rare clinical manifestation, which is why other types of diseases with a higher diagnostic probability were ruled out. Considering the weight loss, abdominal mass and history of immunosuppressant treatment, samples had to be taken for pathology to determine the proper medical therapy. In light of the vague symptoms and suspected ab dominal mass, with initially unclear results, he required a biopsy via colonoscopy and histopathological diagnosis of chronic colitis due to Mycobacterium tuberculosis, which improved after antitubercular treatment. This clinical case will contribute valuable information and important clinical points for daily medical practice for ITB diagnosis and treat ment, as a careful study and a proper step by step process is needed to rule out ITB.











 texto en
texto en