Introduction
In 1877, Cohnheim described and defined paradoxical embolism as the passage of a venous thrombus into the systemic circulation via a cardiac right to left shunt, through a patent ductus, interatrial, and/or interventricular communication.1 Straddling thrombi in the foramen ovale were originally described by Nellessen in 1985, with a risk of impending paradoxical embolism and associated with several conditions including embolic stroke, platypnea-orthodeoxia syndrome, divers gas embolism, and migraine.1,2) During pregnancy, a thromboembolic physiological status develops, influenced by increased activity of coagulation factors VII, X, and VIII, in contrast with decreased fibrinolytic factors activity, mainly protein S.3
Clinical case
A 37-year-old patient with 27 weeks of pregnancy, works as a road technician, born in Bogotá (Colombia), mestizo race, weighs 65 kg and is 1.60 m tall, was discussed. Her only medical history is childhood hepatitis A (ObGy profile: G3P2C0V2) and uneventful previous term pregnancies with vaginal delivery. The patient came to the clinic because of a 15-day course of progressive dyspnea up to functional class IV/IV. Her physical examination evidenced tachycardia and pansystolic murmur grade VI/VI, radiating to baseline foci with S2 reinforcement. Positive fetal movements with 140beats/min fetal heart rate. Evidence of equimosis and asymmetry of the lower left limb.
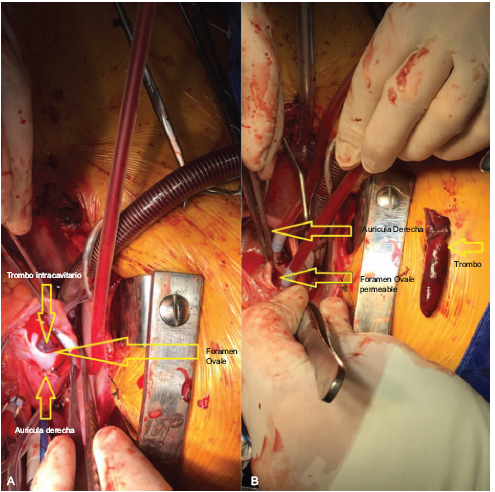
In the ER, suspicion of pulmonary thromboembolism (PTE) was confirmed with transthoracic ultrasound; the foramen ovale evidenced cylindrical echodensity 60mm long and 14 mm of diameter actively crossing the foramen ovale (straddling thrombus) with at least 30 mm of the thrombus localized in the left atrium (Table 1 and Fig. 1). Additionally, the left lower limb was asymmetric and deep venous thrombosis (DVT) of the left popliteal vein was confirmed with Doppler. Cardiovascular surgery performed a thrombecomy and closure of the foramen ovale with a surgical time of 180 minutes (min), under extracorporeal circulation of 71 and 47min clamp. Blood cardioplegia. Invasive hemodynamic monitoring and pulmonary artery catheter. Bleeding 500 mL. Temperature 34°C. Nitric oxide was initiated due to supra-systemic pulmonary hypertension (Table 2). The surgical findings included a large 50 mm long x 10 mm wide thrombus; 80% of the thrombus was lodged in the left atrium, anchored to the septum and across the foramen ovale (Fig. 2). Continuous Doppler was used for fetal monitoring. At the time of admission to the Intensive Care Unity (ICU), the patient was under assisted ventilation, vasopressors, inotropic agent, and inodilation. The fetal heart rate was 120bpm, capillary filling over 4seconds. Forty-eight hours later, the ultrasound examination confirmed the absence of fetal heart rate. After 18hours, during delivery the patient experienced 2.000mL of blood loss, the red code was activated and managed with crystalloids, 4 Red Blood Cells (RBC) units were transfused, and a Bakri uterine balloon was placed for uterine tamponade; additionally, rectal oxytocin, methylergonovine, and misoprostol 400 mg were administered. The uterine balloon was removed after 48hours. The hemodynamics and arterial blood gases evolved satisfactorily to enable the removal of the multisystem support (Table 2). The invasive ventilation strategy developed successfully for 5 days, using a controlled assisted ventilation approach, positive end expiratory pressure of 8, with high-inspired oxygen fractions (100%) during the first 24 hours, using nitric oxide.
Table 1 Transthoracic echocardiography

LV=left ventricle, RV=right ventricle, LVEF=LV ejection fraction, PSBP=pulmonary systolic blood pressure, IV=interventricular.
Source: Authors.

Source: Authors.
Figure 1 Transthoracic ultrasound. (A) Parasternal view. (B) Four chamber view. Right atrium (AD), left atrium (AI), right ventricle (VD), left ventricle (VI), aortic valve (VAo), patent foramen ovale (yellow arrow), trombus (red arrow).
Table 2 Hemodynamic profile, arterial-venous blood gas and vasopressor support
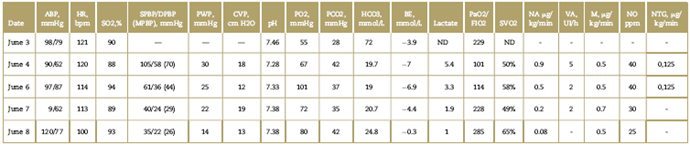
BP=blood pressure, HR=heart rate, PVC=central venous pressure, SO2=arterial oxygen saturation, SABP=systolic arterial blood pressure, DPBP= diastolic pulmonary blood pressure, MPBP=mean pulmonary blood pressure, PWP=pulmonary wedge pressure, BE=Base excess, SVO2=venous oxygen saturation) noradrenaline=NA, vasopressin=VA, milrinone=M, Nitroglycerin=NTG, nitric oxide=NO, parts per million=ppm, NA=not available
Source: Authors.
Source: Authors.
Figure 2 Intracavitary thrombus. (A) The foramen ovale is depicted with the intracavitary thrombus (right atrial view). (B) Depiction of he intracavitary thrombus and the foramen ovale.
The cardiac failure management was optimized reducing the ventricular response with carvedilol, cardio-selective betablocker, enalapril, angiotensin-converting enzyme inhibitor, and spironolactone, with a view to blocking the renin-angiotensin-aldosterone axis (neurohumoral block). Anticoagulation with low molecular weight heparin. Subsequently, the patient developed congestive and erythematous breasts, temperature of 39°C with no leukocytosis and was interpreted as mastitis and treated with meropenem. Positive blood cultures for Citrobacter freundii (cyclic AMP inducer). The patient was discharged after favorable clinical evolution.
Discussion
The foramen ovale is an interatrial communication during the fetal period allowing for the passage of oxygenated blood from the placenta into the systemic circulation. A patent foramen ovale persists in 25% of the adult population.2 Impending paradoxical embolism is a very rare condition. Few case reports or observational studies can be found in the last 5 years, and the only systematic review available in the literature includes 174 patients.4-7) We found a total of 6 cases in Ibero-America.8-13 The occurrence of patent foramen ovale during pregnancy and puerperium is very rare.8 The differential diagnosis includes vegetations and myxomas.2 Clinically, the condition presents with dyspnea, chest pain, and syncope. Paradoxical embolism is rare, with a 91% prevalence of pulmonary and 55% systemic involvement.2,4 Five factors must be present for the condition to develop: (1) an embolic source (DVT and/or PTE); (2) abnormal right and left circulation communication; (3) angyographic or pathological evidence of embolism; (4) a pressure change that favors the right to left shunt; and (5) the arterial embolism shall not originate in the left circulation of the heart. The previously listed conditions represent a final diagnosis and comprise the triad described by Dahl Iberson in 1930, that is, an embolic source, the nature of the source has to be venous, and the presence of shunt.9,14) The mortality rate is 18%, and 66% of the patients die in the first 24hours.4 The main causes of death are cardiogenic shock and/or right ventricular failure, followed by stroke. DVT was the source of the embolism in 22% of the cases, with at least 1 risk factor identified in 35% of the patients, including primary hypercoagulability, malignancy, recent postoperative period, immobility of the patient due to fractures, inadequate antithrombotic prophylaxis. The diagnosis was done via transthoracic and transesophageal echocardiography, computerized tomography, magnetic resonance, in 57%, 40%, 2.9%, and 0.6%, respectively.15
With regards to therapy, there are 3 options: heart surgery, thrombolysis, and/or anticoagulation. The last 2 are more prevalent in posterior embolism at the start of therapy as compared with surgery; furthermore, the latter presents lower probability of systemic embolism and death, versus anticoagulation alone, in addition to shunt closure. Thrombolysis could be the initial therapeutic approach in case of severe PTE, with or without intracardiac thrombi; the association with systemic embolism is of 23.5%5,15-17
Conclusions
The association between patent foramen ovale and impending paradoxical embolism is infrequent. Its presentation during pregnancy is even rarer, but its impact among the young and healthy population presents with a high morbidity and mortality for both the mother and the child, leading to a social and economic impact resulting from the considerable costs of care.
The existing evidence about treatment to date is weak, though surgical management is apparently favored over thrombolysis or anticoagulation, in addition to the benefit of a definite surgical solution to the patent foramen ovale.
Ethical responsibilities
Protection of people and animals. The authors declare that no human or animal experiments were conducted for this research.
Confidentiality of the data. The authors declare that they have adhered to their institutional protocols regarding the publication of patient information.
Right to privacy and informed consent. The authors have obtained the informed consent of patients and/or subjects mentioned in the article. The consent forms are in custody of the correspondent author.











 texto en
texto en 


