INTRODUCTION
Patient safety is understood as "the absence of avoidable harm to a patient during the medical care process, and the reduction of the risk of unnecessary healthcare-related harm down to an acceptable minimum" 1. Deficiencies in processes designed to ensure patient safety, hereinafter referred to as "no safety," increase the risk of morbidity, mortality and disability, as well as length of stay, leading to higher health-related costs 2,3. "No safety" results in adverse outcomes which are mostly avoidable and unjust, creating what could be considered another form of inequity in health.
Since the publication in i999 of the United States Institute of Medicine Report, patient safety and harm prevention have become pivotal objectives in medical care 4. In recent years, international organizations, governments and healthcare institutions have shown a growing interest in improving patient safety both in inpatient as well as outpatient settings 5,6; this has been reflected in the promotion of state policies 7, as has been the case in Colombia 8,9.
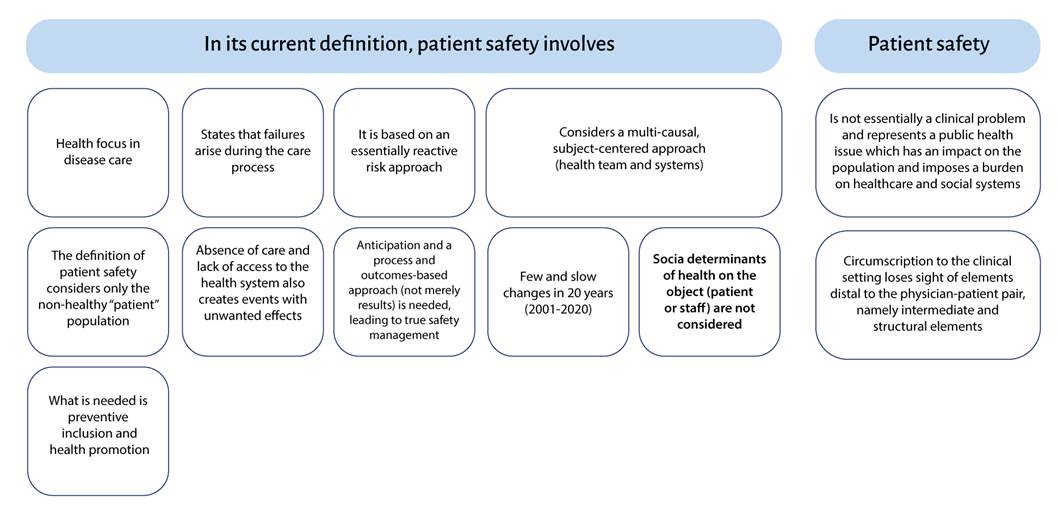
Notwithstanding, actions to improve patient safety are still circumscribed to healthcare institutions which, together with the providers, have been assigned this responsibility, with blatant absence of overarching action frameworks that consider other structural determinants such as culture, policies, economic and social characteristics, and intermediate determinants such as institutional and health system policies as additional contributors to poor health outcomes which perpetuate health inequities.
Patient safety is an essential component of quality healthcare, which is what the general population is constantly demanding worldwide. Consequently, ensuring quality healthcare should not be a matter of clinical interest only but a public health priority 6,10, so that all actions planned or implemented can have an impact at all levels - macro, meso and micro - and ensure intersectoral support to help the population remain safe when seeking and receiving healthcare.
PATIENT SAFETY AS A PUBLIC HEALTH PROBLEM
Incidence, prevalence and preventability of unwanted events derived from the absence of patient safety
In an initial attempt at describing unwanted events in patients, researchers of the Harvard Medical Practice Study defined adverse event as "harm caused by medical treatment - not the underlying disease - which results in extended length of stay, disability at the time of discharge, or both" 11. Other consequences have been incorporated into this definition, and unwanted events have been recently renamed as reportable events with unwanted effects (REUE) 12,13 in order to avoid the stigma associated with the term adverse. This designation recognizes that the ensuing harm is not exclusively attributable to medical care but may occur as a result of the absence of the indicated medical care, may require follow-up and additional treatment or hospitalization and, in more serious cases, may even lead to death.
The "no safety" burden in the world is represented in terms of REUEs, their incidence, prevalence and associated costs, as well as the ensuing consequences. Despite considering the burden only in terms of unwanted outcomes, figures show that it is a complex problem associated not only to institucional care but rather a health issue.
In its latest report (2019), the World Health Organization (WHO) reports that REUEs are currently among the top ten causes of death and disability in the world. It is now known that between 2.8% and 52.2% of patients suffer harm during their care process, and 50% to 83% of these events are preventable. A contextual evaluation of these numbers shows that there are differences depending on the place of occurrence. In low income countries, the annual REUE rate is higher than in high income countries, and up to 30% of these events have a fatal outcome. It is also known that, in high income countries, preventability is substantially higher than in developing or low income countries (83% versus 50%) 2.
As far as mortality is concerned, REUEs are among the top 15 causes of disease burden worldwide 14, with a burden that is comparable to that of diseases such as malaria or tuberculosis; and like with these conditions, REUEs are more frequent in low income countries 15.
The most frequently occurring REUEs are associated with medication errors (18.3%) 16 and incorrect or delayed diagnosis - occurring in 5% of outpatients in the United States - 50% of which are severe 15. In the inpatient context, healthcare-associated infections occur, on average, in one out of 10 hospitalized patients (12.2%) 16, surgery-associated REUEs occur in close to 27% of procedures 16, close to seven million surgical patients suffer complications every year and, of this group, 14.3% die as a result of these REUEs. Other REUEs depend on the setting in which they occur, the incidence being the highest in intensive care units 17 and emergency departments 13.
In Latin America, the burden of no patient safety is similar to the rest of the world. The prevalence of REUEs in hospitalized patients is close to 10.5%, while preventability described in the IBEAS study carried our in 5 Latin-American countries in 2011 was nearly 70%, with variations among countries (range 46.1%-68.5%).
The "no safety" burden has also been estimated for Colombia in particular, with cumulative incidences ranging between 5.8% and 52.2% (13, 17-20). Differences have been reported depending on the estimation methods and the clinical care settings: for example, in surgery (11.8%) 13 there is a two-fold increase over the incidence observed in non-surgical services (5.1%) 20, while in intensive care units, reported frequencies are up to 10 times higher (52.2%) 17.
Consolidated institutional healthcare-associated infection data are collected in Colombia since 2016. As of the first semester of 2020, these data show incidence rates of bloodstream infections of 2.13 for every 1000 central catheter days, 1.9 for symptomatic urinary tract infections for every 1000 days of urinary catheter, and 3.6 for every 1000 ventilator days for ventilator associated pneumonia 21.
REUE preventability varies between 58% 19,22 and 75% 13, and more than 30% of these REUEs are associated with medication errors. Mortality and associated disability have also been estimated at 4.16% for REUEs in surgical services 13.
All these REUE figures are meaningful to the extent that they are placed within the context of the demand for health services and effective care provision in Colombia. According to the databases of the Social Protection Integrated System (SISPRO), for the time period between January 2001 and April 2020, the demand for health services amounted to 3121592725 care instances, as reported by health management organizations (EPS) to the Ministry of Health and Social Protection 23). Therefore, the estimated occurrence of REUEs resulting from no patient safety would range between 218511491 and 312159273 during the same period, with close to 75% of these events being preventable.
Costs of no patient safety
Despite the efforts carried out in the world to reduce the burden of patient harm, it appears that the situation has not changed significantly in the past 15 years. The latest WHO report of April 2019 2 shows REUE prevalence figures similar to those recorded worldwide in the first five-years of the 21st century 24-26. Data continue to reflect a landscape of differences with low and middle income countries. The WHO data show that two-thirds of all REUEs occurred in low and middle income countries 14. More recently, data from the Institute for Health Metrics and Evaluation (IHME) suggest that the burden of disease as well as the economic impact related to REUEs for the health systems and populations of low and middle income countries are high 15.
In general, the cost of care of one REUE per patient ranges between 156 and 50,223 dollars. Differences in terms of populations, methods, perspective and type of REUE assessed account for this variability 20. In terms of resource savings for the health system, the figures reported by the WHO are also significant. In the United States, for example, cost savings for every REUE avoided in Medicare hospitals between 2010 and 2015 amounted to 28 billion dollars 2.
In Colombia, the median estimated cost of REUEs in 2013 was 685.6 dollars per event. This cost in surgical and non-surgical medical services amounted to 850.4 and 533.2 dollars, respectively 20. The impact of these costs on the health system can be determined when analyzed within the perspective of REUE incidence, in accordance with the number of healthcare instances in the country.
Although the approach to "no safety" costs is based on the identification of direct costs, patient harm imposes a burden on the resources of the health system and on society as a whole. Harm to the patient and the people is directly reflected on the need for additional treatment, more diagnostic testing, hospital admissions and readmissions, prolonged length of stay and other additional requirements that compromise already scarce health resources. However, the broader financial effects of patient and people harm are not direct costs but rather persistent morbidity and lower life-long productivity of both patients as well as caregivers; consequently, financial impact flows over from health economics to the economy in general and is also reflected in lower trust in the health system and in social institutions 15.
LIMITATIONS OF THE PATIENT SAFETY DEFINITION
Patient safety is defined by the World Health Organization as "the absence of preventable harm to a patient during the medical care process and the reduction of the risk of unnecessary healthcare-related harm down to an acceptable minimum. An acceptable minimum refers to the collective notions regarding current knowledge given the available resources and the context in which the care is provided vis à vis the risk of not receiving or receiving a different treatment" 1).
This definition focuses specifically on the results of a series of risk management measures; however, in Colombia this definition does not imply only outcomes but the entire process, including actions and methods designed to prevent events that can result in unintentional harm to the patient and that occur during service provision or as a result of it, and to mitigate their effects on the patient. Patient safety "implies ongoing evaluation of risks related to medical care in order to design and implement the necessary safety barriers" 27.
Regardless of which definition is adopted, there are common elements of what patient safety includes, such as preventing the "risk of harm" or mitigating "harm" in a "patient" during the "care process". These elements circumscribe patient safety to the clinical setting in which healthcare is provided and to the patient as a subject, and establish a field of actions focused on harm prevention and mitigation.
Figure 1 illustrates the main gaps in the current definition of patient safety.
Patients as subjects of healthcare and patient safety
The narrow range of action on the patient safety target population arises from its definition. The patient, a term which is actually part of its name, is separated from other groups of people who may be interacting with the health system without being patients themselves.
The word patient implies a subject who receives care from a physician while at the same time suffers from an illness or a particular condition. This definition arises from the conception of health as the absence of disease, warranting the demand for healthcare as a consequence of the lack of health, without any consideration of other elements designed to prevent disease, improve wellbeing and promote health as a wholesome state of physical and mental wellbeing.
The connotation of the word patient is not purely an element of form but rather the result of how relations between the person demanding service - a passive recipient- and the action of the physician whose job is to recover "altered" functions are conceived. Within this purely biologistic and curative approach, disease becomes all important while other individual values such as life circumstances are dismissed.
Also, the individual way in which health and disease are conceived by environmentalist and anthropological schools also has its limitations because it circumscribes the understanding of the nature of health and disease, isolating them from the social, ethical, moral and historical processes of mankind, which play an important role in the emergence of disease. Cases in point are AIDS, tuberculosis and some other pandemics which reflect a clear restructuring of society, with changes ranging from the redistribution of population settlements to the imposition or development of new economic and social models during certain historical periods that play a role in the emergence of such diseases.
Brought to the realm of patient safety, the implicit conception of patient automatically depicts a person afflicted by a disease who demands health services and who is at the mercy of the healthcare professionals and their decisions. Therefore, any unwanted outcome or harm to the individual who seeks care will be the result of that individual's poor state of health (biological characteristics and morbidity) and of the decisions made by the healthcare team.
This perception of patient safety disregards those other factors either inherent or external to healthcare which have been shown to be determinants of the achievement of good health outcomes 28-30. This limitation plays in favor of a form of risk management centered on the person seeking care, the health team and the care process, thus favoring individualization of guilt 31,32 and placing the blame for latent flaws on individuals who are victims of more complex processes that determine many of their actions. Consequently, important elements other than the individual and care in health institutions are disregarded as a result of the limitation of considering only the patient and not the person; and if these elements were to be intervened, they could have an effect on improving safety in healthcare and preventing harm.
Risk of REUEs beyond the healthcare process
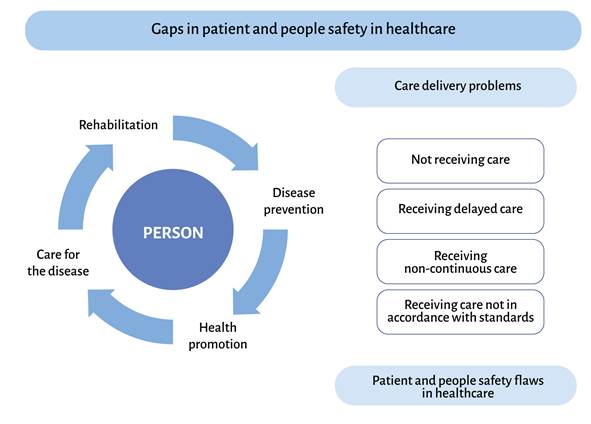
The original definition of patient safety circumscribes the occurrence of REUEs to the process of receiving care. However, it is known that care is not effectively provided to all the population that demands health services and, therefore, the absence of care or untimely care can also result in harm to the people.
In Colombia, access to health services was estimated at 75.5% of all the people needing those services in 2012 33. Even within the framework of nearly 97% insurance coverage in a State where health is a fundamental right 34, ensuring effective access to essential health services continues to be a challenge. Access barriers are not inherent only to institutions (providers and insurers) in which bureaucratic hurdles and imposed restrictions limit service provision due to funding schemes based mainly on capitation payments 35. Economic, geographic (distance to care sites), limited availability of service centers and specialized medical personnel and their territorial distribution - which appears not to follow the distribution of the health needs of the general population - are other types of barriers.
To date, there are no studies confirming the proportion of REUEs associated with failure to receive care; however, some behaviors adopted by the general population to improve symptoms in view of the lack of care and which may translate into a risk of harm have been tracked. The 2012 National Quality of Life Survey (ENCV) showed that close to 77% of all Colombians needing medical care attended a health institution or saw an independent medical practitioner or specialist; notwithstanding, of 23% of the people who did not attend a health center or see an independent physician, 64.2% used home remedies or self-medicated themselves, while 22% went to a druggist or a pharmacist , and 11% did nothing to solve the problem 36. All this can increase the risk of medication errors, fosters inadequate prescription practices by non-competent or non-authorized personnel, and can delay diagnosis and timely care, with the resulting harmful effect for the individual and indirect impact on health services due to the higher resulting cost of caring for worsened conditions 37.
This is the kind of landscape that calls for reflection on the "no safety" problem, not only among patients who receive care, but among the entire population prone to require health services at any time, whether they are ill or not. According to the WHO, health services are all those activities and products that a healthcare provider can offer to a general community 38, including prevention, promotion, treatment, rehabilitation and palliative care. Thinking of healthcare as something that applies only to a disease condition and not as a way to advance health prevention and promotion is a reductionist view of health which, on occasions, takes precedence in the management of the resources of the health system.
LIMITATIONS OF PATIENT SAFETY IN ITS ACTION SETTINGS
In general terms, estimation of the "no safety" burden has focused on healthcare-associated REUEs, assigning to healthcare teams an "etiologic" role. However, it is essential to consider other aspects such as care characteristics, institutions, policies, health services, teams and patient-related factors, all of which may contribute to the occurrence of REUEs. To the extent that systems create barriers that reduce risk based on the appropriate recognition of these factors, the occurrence of harm 24,39 as well as the risk of occurrence can be reduced, moving management systems towards proactive prevention-oriented strategies. In this regard, it is essential to highlight the key role of multifactorial and multi-system analyses of REUEs 12 as part of patient safety, given that they represent an opportunity of improvement for appropriate risk management 39.
This approach recognizes several levels at which failures may occur, leading to person harm or to a situation which represents a risk of harm. This approach, known as systems approach, recognizes the existence of active flaws usually consisting of errors made during the care process by first-line human resources, as is the case with medication errors. It also recognizes latent flaws inherent to organizations, service administration, health technologies, organizational culture and administrative decisions. Other levels at which flaws are latent and affect those who receive care as well as those who do not exist outside the institutions and include public policies and the characteristics of the healthcare systems, which may have repercussions on working conditions and service provision, thus promoting errors during care.
REUE risks derived from untimely care
The risk of unwanted outcomes in people who demand health services increases also as a result of untimely or delayed access to care. The consequences for people who have to wait in order to receive needed care can be devastating, as delayed treatment can lead to worsening of preexisting or acute conditions that may result in a worse health outcome or the need for potentially more complex procedures 40-43.
Some disease conditions create greater compromise when their treatment is delayed, as is the case with cancer. There is evidence about the effects of delaying treatment in patients with early head and neck cancer in which tumor control is compromised if treatment is initiated more than 40 days after the patient is initially assessed by a radiation oncologist. Furthermore, tumor progression is associated to a large extent with waiting time as well as with poor outcomes 44. In other types of cancer such as lung, a relationship has been shown to exist between delayed care and poor health outcomes, where "even a delay of a few months between diagnosis and treatment significantly influences the consequences of cancer" 45.
In other situations such as hip replacement, long waiting time for surgery may result in greater deterioration and worse outcomes after treatment 46,47. In spine surgery, longer delays can also lead to worse outcomes, including a lower probability of improvements in physical function and pain 48. Waiting for a long time to undergo cataract surgery is also associated with negative effects, including impaired quality of life, a higher risk of falls and accidents, and a higher risk of greater visual loss after treatment 49.
The scenario can be life-threatening. A study conducted in Canada has shown that between 25,456 and 63,090 (mean of 44,273) Canadian women may have died as a result of longer waiting time during the time period between 1993 and 2009 40.
Prolonged waiting can also affect mental health due to longer exposure to pain and discomfort, anxiety at not knowing what to expect from the health condition, dependence on a caregiver - undermining the individual's autonomy and dignity - isolation, and even strained personal relations. Other potentially serious consequences which reduce longevity include diminished health in general, chronic addiction to analgesics and narcotics, and a greater risk of depression while waiting to receive care 37. These consequences are disastrous for health, which is understood as a state of physical and mental wellbeing, as well as the ability to adapt and cope with social, physical and emotional challenges.
In the Colombian setting, there is no knowledge of what the health system's ability to respond with timely access to care represents in terms of harm and mortality among the population that demands healthcare services; however, it is clear that there are delays in accessing general services (3 to 5 days on average after asking for an appointment) as well as specialized care (11 days to a maximum of 15 on average). There is also evidence of inadequate management of the risk of complications derived from the high rate of cancellations of elective and non-elective surgical procedures due to causes attributable to the institution (1.5% in 2019) 50.
REUE risk due to gaps in disease prevention
No patient safety is also due to failings in disease prevention processes, particularly in those cases in which there are highly effective mechanisms to ensure health, as is the case with immunization. In Colombia, despite the availability of biologics, there are departments where the goals of immunization in the pediatric population are not met (at least 95% of the children under 4 years of age). Specifically, for example, there is a coverage gap in MMR vaccination in children under 1 year of age, found to be under 90% in 2019 for 5 of the 32 departments of the country: Vaupés (89.96%), Santander (89.3%), Nariño (88.5%), Córdoba (88.59%) and Chocó (86.15%) 51. Suboptimal coverage plays in favor of unwanted events and the emergence of disease, not as a result of care but of inadequate planning of disease prevention activities, especially when differential approaches are needed in view of access barriers.
In other settings, lack of vaccination may result in fatal consequences, as is the case with neonatal tetanus, a disease which is 100% preventable but continues to be reported in Colombia (2 cases in 2018, 1 case in 2019 and 2 cases in the first part of 2020) 52.
Another effect of "no safety" stemming from deficiencies in prevention is reflected in incident cases of congenital syphilis, a condition that can be prevented by means of maternal treatment during pregnancy. The cumulative incidence of this condition in Colombia was 1.54 for every 1000 live births in 2018, with the national average in 2021 being 2.03 cases for every 1000 live births. However, there are stark differences among regions, with departments showing figures above the national average, as is the case in Arauca and Casanare, with 3.78 and 1.7 cases for every 1000 live births, respectively 53.
Consequently, although the occurrence of REUEs has been defined historically as associated mainly with medical care, where patient safety actions are placed, some failings which trigger the emergence of those events are associated with the lack of care, that is to say, when services, diagnosis or treatments are delayed or simply not provided. For this reason, from a Public Health perspective, patient safety could be defined as the set of structural elements, processes, tools and methodologies based on scientifically proven evidence that should be in place to prevent the occurrence of harm in populations or communities of patients or of healthy individuals during their interaction with the health systems, all this as a result of the implementation of health policies and programs and not only of the care process, as it is currently understood.
Figure 2 shows a proposed frame of reference to approach healthcare safety flaws during care delivery.
CURRENT ACTION STRATEGIES AND THE NEED FOR MULTI- AND INTERSECTORAL PUBLIC HEALTH INTERVENTION APPROACHES
After the publication of the document To err is human in 1999 54, and as a result of other antecedents such as malpractice lawsuits 55, suspected malpractice in healthcare institutions 56,57, confusion due to the risk of polypharmacy especially in the elderly 58, and bafflement as to who should be liable for events resulting in severe consequences for the patients, international policies led by the WHO with the aim of improving quality of care and patient safety began to emerge 5,59,60.
Apart from these initiatives, countries, particularly high income countries, began to create partnerships and programs, as well as public policies designed to prioritize and improve patient safety 61,62. These government actions coming from different parts of the world coincided on the need to set up incident reporting systems as part of their strategies, promote patient safety culture with a systematic approach, and involve patients, caregivers and citizens as a whole in the process of improving safety. All this is appraised more as Public Health actions and identified with the objectives of the latter, which are designed to mobilize community partnerships to identify and solve health problems, develop policies and plans to support individual and community health efforts, create links between the people and their personal health services, ensure provision of medical care when unavailable, and ensure the availability of human resources with the necessary competencies in personal medical care.
Colombia is another example of how patient safety begins to cross the narrow boundary between clinical work and Public Health. The patient safety policy emerged as such in 2008 8, mandated by the Ministry of Social Protection. The policy sets forth guidelines for its implementation, recognizes objectives that transcend the clinical setting, such as the coordination of different players to ensure improvements in quality of care and education of patients and families regarding knowledge and management of factors that can potentially influence the safety of the care processes to which they are subjected.
Despite this timid encroachment on Public Health, the Colombian policy cuts across a single system, that of health and quality management, apart from following the epidemiological model of multi-causality and the systems approach which guides proposed actions to improve patient safety in this country. This policy leaves out elements already mentioned which are relevant to the implementation of actions to improve patient safety: recognition of risks which are not exclusive of the care process and contributing factors which go beyond clinical settings. Neither does the political and implementation framework consider contextual or complexity of care differences between inpatient and outpatient care, or the degree of complexity of first, second or tertiary level institutions, urban versus rural areas, or cognitive biases in patients and other players of the health system. Consequently, its implementation could deepen inequities in terms of safety and unwanted health outcomes.
The notion of patient safety as a clinical matter, though entrenched in the minds of risk managers, has significant consequences for the way in which improvement and risk prevention actions are planned and conceived, given the little importance attached to determinants of the health process which are not to be found in the clinical setting but which are important to consider if the best results in terms of patient and population safety are to be achieved.
Health services often fail in terms of access, quality and quantity, especially for some sectors of the population. Regional differences in health and healthcare have been described in the literature for more than 30 years, and occur regardless of the prevailing political or economic system. Health inequity exists when those differences are unnecessary, avoidable, arbitrary and unfair 63.
There has been a transition in the way in which risk and patient safety management is approached, with an evident responsibility shift from health professions which have the knowledge, experience, clinical autonomy, self-regulation 64 or a lack thereof, to the recognition of a system with its characteristics and organizational components within a broader landscape. However, despite this transition, numerous relevant elements still remain outside this consideration. These include social, economic, political and racial differences which are also determinants of health outcomes and can be at the origin of unwanted health outcomes, creating blatant inequities.
Equity in healthcare can be defined in terms of access and use of the health system according to individual needs, as well as in terms of the quality of care offered to all the sectors of the population as a requirement to ensure people and patient safety. Equity in healthcare does not only refer to individual state of health, but to all other social determinants that affect the state of health in itself and which determine the interaction between people and services, as is the case of access, adequacy and quality of care as fundamental pillars of patient safety.
Recent publications in the literature suggest that negative outcomes in patient safety and the occurrence of adverse events are associated with sex and gender, racial, ethnic, educational and socioeconomic inequalities 65-67. Moreover, the characteristics of the health systems, the private or public nature of healthcare provision and the characteristics of the health institutions are associated with the incidence of REUEs, in particular preventable REUEs 68,69. Despite this recent recognition, these elements are not reflected, at least explicitly, in state policies around patient safety, hence the absence of components in their statements aimed at closing inequity gaps in risk management and, consequently, in safety outcomes.
In view of all of the above, it is clear that patient safety is not essentially a clinical matter but a public health problem with significant impact in terms of morbidity and mortality for the general population, and a high burden for social and health systems stemming from costs and disability. It is also evident that a definition which is circumscribed to the clinical setting loses sight of intermediate and structural elements that go beyond the practitioner-patient level and which act as facilitators of harm to people who demand health services and who may or may not gain access to them.
Safety in health is not inherent to the patient but to the individual who interacts with the health system, is engrained in a context that cannot be overlooked and is vulnerable to social determinants which influence outcomes. An unbiased perspective of the implementation of patient and people safety practice ought to include these elements. This requires a look into the adequacy of the definition of patient safety put forward by the WHO and other international patient safety organizations which believe that it is a direct consequence of the relationship between a patient and a medical team, excluding the non-diseased person who, as mentioned, is at continuous risk of harm or unwanted outcomes.
Moreover, existing action strategies appear not to encompass all the aspects that define patient and person safety in Public Health and need to explore other multi and trans-disciplinary approaches that are suitable for dealing with all the complexity of people harm during their interaction with the health services. Also needed are strategies that can become true policies with inter and multisectoral support and give rise to regulatory, physical and financial resources to guarantee patient and people safety.
These characteristics are not considered by the existing patient safety policy, mainly as a result of the paradigm that considers subjects with events, the medical team and their relations with the system as the object of patient safety study, the system being circumscribed only to inpatient or outpatient care; this overlooks unwanted events occurring in the population not as a result of care but of its absence or restriction, and which are a consequence of how the health system and health policies are designed in the country.
It is also worth noting that although work on improving safety outcomes and reducing REUEs has been going on for more than 15 years, effects have been slow and not as significant as expected. These findings impose the need to ask whether the epidemiological approach is capable of explaining an recognizing all risks and causes of REUEs or whether it is time to consider other paradigms such as that of social determinants which have been shown to act as modifiers of health outcomes and drivers of inequity. Additionally, a clear gap is recognized to exist in terms of how these determinants relate to unwanted outcomes and patient and people safety in Colombia.
There is room to work on this in public health, understanding the complexities of relations among determinants of harm outside the physical setting where care takes place, through work with the communities and incorporation of knowledge from other disciplines covering insurance, access and health outcomes. Moreover, there is a need to consider the evaluation of strategies designed to improve the impact that the lack of effective patient and people safety measures and REUEs have on the general population and in particular on people differentially affected by social determinants of health, namely, race, gender, ethnicity and type of health insurance, among others.
Finally, there is a need to question the sufficiency of the epistemological, praxeological and ontological approach underpinning patient safety practice and fields of action. It is time to start thinking about patient and people safety from the Public Health perspective, not only to characterize the problem but also to propose programs and policies that leave the comfort of managing risk at an inpatient and outpatient level and begin to measure and characterize the consequences that programs, plans and characteristics of the health system are having on the population, and make headway in the development of solutions.
If it is the role of Public Health to promote the development of policies and plans that support individual and community health efforts, connect the people with the necessary personal health services, and assess the effectiveness, accessibility and quality of personal and population health services, monitor health status to identify health issues in the community, diagnose and research health problems and hazards in the community and research new knowledge and innovative solutions for health problems, then there are reasons enough to consider patient and people safety as a Public Health objective which should not be left exclusively to the clinical realm, as stated above.











 texto en
texto en