Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Accesos
Accesos
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en
SciELO
Similares en
SciELO -
 Similares en Google
Similares en Google
Compartir
Revista colombiana de Gastroenterología
versión impresa ISSN 0120-9957
Rev Col Gastroenterol vol.29 no.4 Bogotá oct./dic. 2014
A Case Report of Esophageal Tuberculosis
Camilo A. Manrique M. MD. (1), Diana Carolina Salinas G. MD. (2), Julián D. Martínez MD. (3), Martín A. Garzón O. MD. (4), Geovanny Hernández C. MD. (5), Natan Hormaza A. MD. (4), Jorge I. Lizarazo R. MD. (4), Juan Carlos Marulanda MD. (4), Juan Carlos Molano V. MD. (4), Mario H. Rey T. MD. (4)
(1) Second year Gastroenterology Resident at Universidad del Rosario and Hospital Universitario de La Samaritana in Bogotá, Colombia. camiloandresmanrique@gmail.com
(2) Third year Internal Medicine Resident at Universidad del Rosario in Bogotá, Colombia.
(3) Associate Professor in the Department of Medicine at the Universidad Nacional de Colombia in Bogotá D.C., Colombia.
(4) Gastroenterologist in the Gastroenterology Service at Hospital Universitario de La Samaritana, Post Graduate study in Gastroenterology at the Universidad del Rosario in Bogotá, Colombia.
(5) First year Resident in Gastroenterology at Universidad del Rosario and Hospital Universitario de La Samaritana in Bogotá, Colombia.
Received: 22-11-13 Accepted: 05-11-14
Abstract
We report the case of an immune-competent man with symptoms of upper gastrointestinal bleeding secondary to esophageal ulcers of tubercular origin. Gastrointestinal involvement from Mycobacterium tuberculosis is rare even in patients with numerous occurrences of pulmonary and extrapulmonary diseases. The most frequently affected sites are the terminal ileum and the peritoneum. Esophageal tuberculosis is exotic and is usually secondary to extension from neighboring infected organs such as the mediastinal nodes and/or the bronchi.
Clinical, endoscopic and radiological pictures of the esophageal disease often mimic malignancy. Tuberculosis treatment is the mainstay of treatment, and surgery is rarely required.
Keywords
Esophageal tuberculosis, ulcers, gastrointestinal bleeding
CASE PRESENTATION
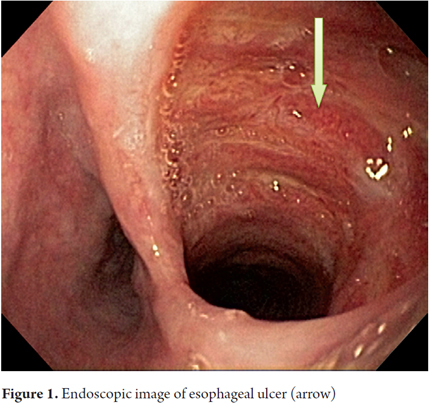
An 86-year-old farmer was admitted to the hospital after vomiting blood for the two previous days. Patient had no hemodynamic compromise. Digestive tract endoscopy showed an ulcerated lesion suggestive of malignancy in the middle third of the esophagus. The lesion was deep, had hard raised edges and measured 20 mm in diameter. Black clots of blood were found adhering to the lesion (Figure 1). No other mucosal damage was found the stomach or the duodenum. Given the patient's hemodynamic stability, it was decided to remove biopsy samples from the lesion and send them to the pathology laboratory notwithstanding the presence of blood clots.
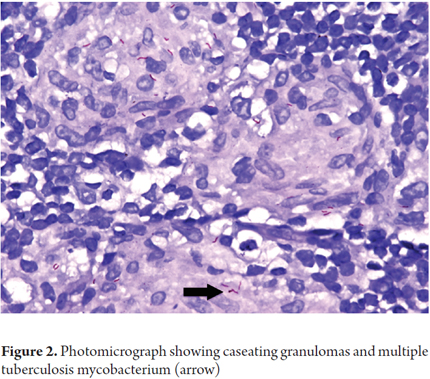
The histopathological report showed granulomatous changes of the esophagus which originated in tuberculosis. A Ziehl-Nielsen stain showed the presence of abundant acid fast bacilli (Figure 2).
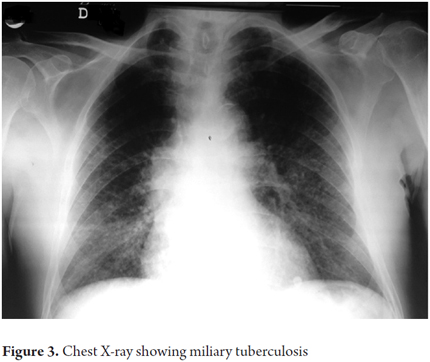
Both the patient and his relatives stated that he had no coexisting respiratory symptoms. A chest x-ray was compatible with miliary tuberculosis (Figure 3). An ELISA test for HIV was negative.
COMMENTS
Worldwide, tuberculosis (TB) is a major public health problem in developing countries as well as in industrialized countries. About a third of the world's population (two billion people) are infected with mycobacterium tuberculosis. Although its incidence has declined since its epidemiological peak in 2003, the numbers remain alarmingly high. In 2010, the World Health Organization estimated that globally 1.4 million people die every year as a result of TB and that there are 8.8 million new cases every year (1).
The causes of the increase in new cases throughout the world are considered to be an association with HIV infection which has been documented in 1 out of every 14 new TB, and growing resistance of the bacillus to antibiotics (1).
Extrapulmonary tuberculosis accounts for 22% of all TB cases, more than half of which occur in patients who are coinfected with HIV (1).
Among patients who do not have HIV, the most frequent locations and types of extrapulmonary involvement are in the lymph nodes (35%), pleura (20%), bones and joints (10%), gastrointestinal tract (9%), miliary tuberculosis (8%), tubercular meningitis (5%) and peritoneal tuberculosis (3%) (2-4).
Esophageal tuberculosis is an exotic entity can be either primary or secondary (5). While there is very little evidence for the primary form, the secondary form is also very unusual though it occurs more often. It occurs by extension from contiguous mediastinal structures affected by TB involved as lymph nodes, bronchia and pleura. Transmission can occur through the swallowing of infected sputum. Lymphangitic and hematogenous dissemination from a pulmonary focus have also been reported as causes of esophageal infection (5).
The esophagus has defense mechanisms that reduce susceptibility to infectious processes. These include esophageal motility, the lower esophageal sphincter, and the covering of squamous epithelium which is bly resistant to infections. That these mechanisms enable effective clearance of tubercular bacilli is demonstrated by autopsy findings from 18,049 TB patients among whom esophageal involvement was observed in only 0.14% to 0.15% of the cases (3). Involvement of the esophagus in TB ranks eighth behind involvement of other extrapulmonary organs.
Symptoms of esophageal tuberculosis vary and are not specific. They include abdominal pain, diarrhea, vomiting, anorexia, constipation, weight loss, and gastrointestinal bleeding. Symptoms are mainly determined by the depth of the compromise of the infected organ. Depth of compromise extends from inflammation of the mucosa to deep ulcers forming exophytic lesions to stenosis. Stenosis occurs primarily in the middle third of the organ and is the main factor in differential diagnosis with squamous cell carcinoma (4).
More than 90% of patients with esophageal TB present dysphagia presents resulting from mucosal ulceration caused by exophytic endoluminal lesions, fistulae, or extrinsic compression due to mediastinal or cervical lymphadenopathy. The middle third of the esophagus is the site that is most frequently affected by the spread of infection from carinal lymphadenopathy which is frequently found in the pulmonary form of the disease. Other complications include the formation of diverticula formation and trachea-esophageal fistulas (3,6).
Several studies have identified risk factors for extrapulmonary involvement including concomitant medical conditions such as neoplasms, corticosteroid therapy, connective tissue diseases, alcoholism, kidney failure, diabetes and pregnancy. Case series have also shown that black men are more susceptible the disease progressing to dissemination (2, 8).
Findings from esophageal endoscopy and x-rays may vary, but they can include exophytic lesions that occupy the lumen of the organ, deep ulcerated lesions of great extent, traction diverticula and fistulas of the tracheobronchial tree. A CAT scan of the chest allows evaluation of other thoracic structures including the pleura, lungs, and vertebrae to determine the presence of mediastinal lymph nodes. Endoscopic ultrasound is a test that is gaining ground for the diagnosis of TB infection since it can provide very precise information about mediastinal lymph compromise and compromises of other adjacent organs in addition to allowing for fine needle aspiration biopsies (10).
The definitive diagnosis of esophageal TB infection must be made through isolation of bacilli in an appropriate culture medium, finding the presence of caseating granulomas and acid-fast bacilli in biopsies of samples from lesions, and detection of bacillary genomic fragments through PCR. This technique has 80% sensitivity and 100% specificity for the diagnosis of extrapulmonary tuberculosis (3, 7, 11).
TB treatment should begin as soon as the diagnosis is confirmed. Given the proper response to treatment, symptomatic improvement and resolution of dysphagia should occur within two months.
The recommended tetra-conjugated drug therapy consists of isoniazid, rifampin, pyrazinamide and ethambutol for two months followed by isoniazid and rifampin for an additional four months. This is similar to that used in the treatment of pulmonary tuberculosis with success rates of around 90%. For selected patients, dilation of esophageal strictures and stenting for the management of fistulas are required. Surgery is only very rarely required (4, 5).
REFERENCES
1. Global tuberculosis control: WHO report 2011. World Health Organization 2011. [ Links ]
2. Garcia JF, Alvarez HD, Lorenzo MV, Callejo A, Fernandez A, Sesma P. Extrapulmonary tuberculosis: epidemiology and risk factors. Enferm Infecc Microbiol Clin 2011; 29(7): 502-509. [ Links ]
3. Sharma S, Mohan A. Extrapulmonary tuberculosis. Indian J Med Res 2004; 20: 316-353. [ Links ]
4. Jain SK, Jain S, Jain M, Yaduvashi A. Esophageal tuberculosis: is it so rare? Report of 12 cases and review of the literature. Am J Gastroenterol 2002; 97: 287-91. [ Links ]
5. Sala A, Leibovich N, Souto G, Sabatini C, Brodersen C, Segal E. Tuberculosis esofágica: presentación de un caso y revisión de la literatura. Acta Gastroenterol Latinoam 2011; 41: 47-51. [ Links ]
6. Rathinam S, Kanagavel M, Sundaravadanan B, Santhosam R, Chandramohan S. Dysphagia due to tuberculosis. European Journal of Cardio-thoracic Surgery 2006; 30: 833-836. [ Links ]
7. Gómez C, Garrido A, Sansó J, Torres E. Tuberculosis esofágica en paciente inmunocompetente. Gastroenterol Hepatol 2003; 26(10): 643-5. [ Links ]
8. Fiske C, Griffin M, Erin H, Warkentin J, Lisa K, Arbogast K, Sterling T. Black race, sex, and extrapulmonary tuberculosis risk: an observational study. BMC Infectious Diseases 2010; 10: 16. [ Links ]
9. Fitzgerald D, Sterling T, Haas D. Mycobacterium tuberculosis, extrapulmonary Tuberculosis. Mandell G, Benett J, Dolin R. Mandell, Douglas, and Bennett´s Principles and Practice of Infectious Diseases. Cap 250. 7ma Ed. Elsevier; 2010. p. 3129-3163. [ Links ]
10. Hadlich E, Galperium B, Rizzon C. Esphageal ulcers caused by reactivation of ganglionary tuberculosis – a case report. Braz J infect Dis 2007; 11(2): 293-296. [ Links ]
11. Bresky G, Silva N, Madariaga J. Esofagitis tuberculosa en un paciente HIV positivo. Rev Med Chile 2007; 135: 1323-1326. [ Links ]











 texto en
texto en