Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Accesos
Accesos
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en
SciELO
Similares en
SciELO -
 Similares en Google
Similares en Google
Compartir
Revista colombiana de Gastroenterología
versión impresa ISSN 0120-9957
Rev Col Gastroenterol vol.35 no.1 Bogotá ene./mar. 2020
https://doi.org/10.22516/25007440.381
Original articles
Upper esophageal varices (Downhill varices): Case presentation and literature review
1 Unidad de Gastroenterología. Hospital Universitario Nacional. Facultad de Medicina. Departamento de Medicina Interna. Universidad Nacional de Colombia - Gastroinvest S.A.S. IDIME. Bogotá D.C., Colombia
2 Departamento de Radiología e Imágenes Diagnósticas. Hospital Universitario Nacional. Departamento de Radiología e Imágenes Diagnósticas. Facultad de Medicina. Universidad Nacional de Colombia. Bogotá, Colombia
We describe 21 cases with incidental endoscopic findings of upper esophageal varices (downhill varices) and relevant data from patients’ clinical histories and endoscopic findings. The male/female ratio was 1:1 and patients’ average age was 67.9 years. The most frequent comorbidity was chronic obstructive pulmonary disease, followed by pneumoconiosis, obesity and apnea-hypopnea syndrome. All comorbidities had associated pulmonary hypertension. The last three causes have not been previously described in the literature on upper esophageal varices. None of the patients had histories of variceal hemorrhaging.
Keywords: Upper esophageal varices; downhill varices; case description; review; pulmonary hypertension
Se describen 21 casos con hallazgo incidental de várices esofágicas superiores (Downhill varices) en endoscopia de las vías digestivas altas. Además, se detallan algunos datos relevantes de la historia clínica y de los hallazgos endoscópicos. La relación hombres/mujeres fue 1:1 y la edad promedio fue de 67,9 años. La comorbilidad más frecuente fue la enfermedad pulmonar obstructiva crónica (EPOC), seguida de las neumoconiosis, la obesidad y el síndrome de apnea-hipopnea, todas con hipertensión pulmonar (HTP) asociada. Las tres últimas causas no han sido descritas previamente en la literatura sobre várices esofágicas superiores. Ningún paciente tenía antecedente de hemorragia variceal.
Palabras clave: Várices esofágicas superiores; Downhill varices; descripción de casos; revisión; hipertensión pulmonar (HTP)
Introduction
Upper esophageal varices are rarely found endoscopically, but when have been, they have been found incidentally or as part of an examination of upper gastrointestinal bleeding. Unlike lower esophageal varices, they are secondary to disorders of venous return from the upper and middle thirds of the esophagus to the superior vena cava (VCS). For this reason they have been dubbed downhill esophageal varices in the English literature.
The most frequent cause in the initial descriptions were obstructions due to mediastinal tumors or fibrosis of the mediastinum. 1 Later, this type of cases increasing treated with intravascular devices to address thrombotic phenomena of the superior vena cava (SVC) and its tributaries. 2
This is a study of a series of cases in which upper esophageal varices were detected through upper digestive endoscopy of the tract. Their etiologies vary and are different from the classic ones mentioned above. Their clinical characteristics and associated morbidity are described, a literature review is presented, and cases are compared with those described in the literature.
Subjects and methods
This is a case series of 22 cases of 21 patients who underwent upper digestive tract endoscopy in medical centers located in Bogotá, Colombia (One patient is featured in two cases). Diagnostic videoendoscopy of the upper digestive tract was used in these cases. The study includes patients’ demographic characteristics, diagnoses, clinical characteristics (when available), and endoscopic findings documented with videos and photographs.
Results were tabulated from parametric and non-parametric measures. In addition, a bibliographic review was performed through a search of PubMed using the search terms: Downhill [All Fields] AND “varicose veins” [MeSH Terms] OR “varicose” [All Fields] AND “veins” [All Fields]) OR “varicose veins” [All Fields] OR “varices” [All Fields]). Articles found in the bibliographies of original articles on the subject were then added as well.
Case descriptions
We describe relevant cases and include clinical data and photographic documents. Then, general findings of all cases are presented in order of chronological description (Tables 1 and 2).
Table 1 Descriptions of patients with proximal esophageal varices.
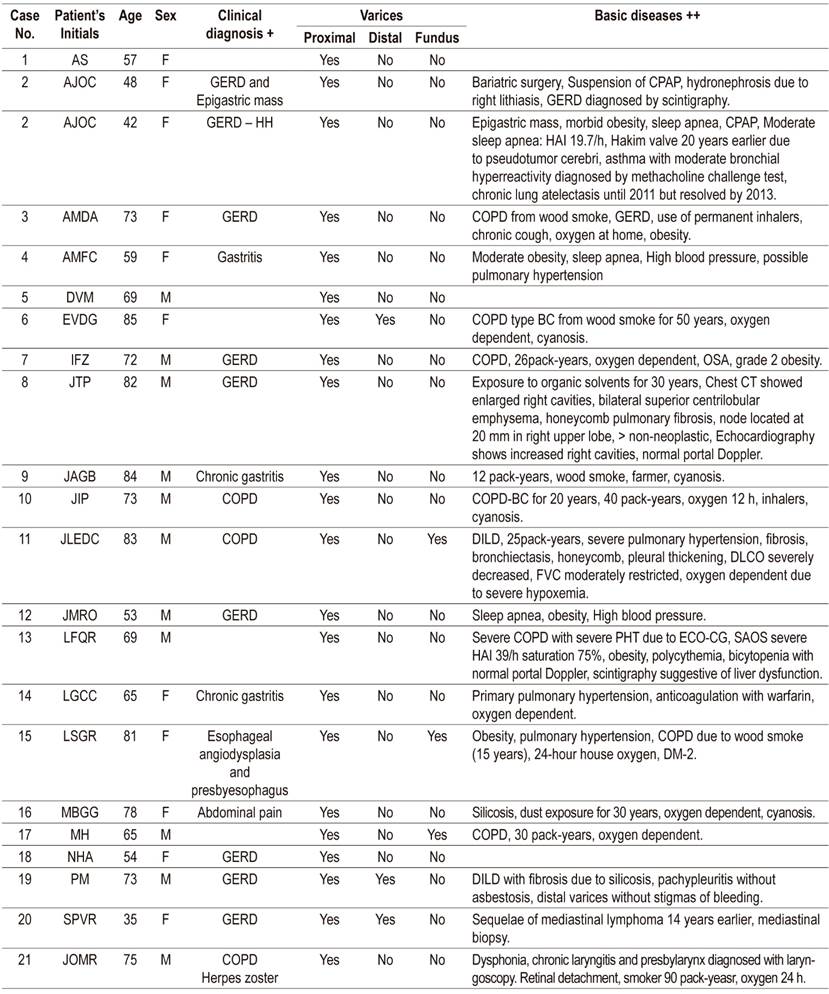
GERD: gastroesophageal reflux disease; HH: hiatal hernia; COPD: chronic obstructive pulmonary disease; CPAP: Continuous Positive Airway Pressure; OSA: obstructive sleep apnea; HAI: apnea/hypopnea index; pack-year: number of packages per year; DILD: diffuse interstitial lung disease; DM: diabetes mellitus; DLCO: Diffusing Capacity of the Lungs for Carbon Monoxide; FVC: flow-volume curve
Table 2 Summary of findings in patients with proximal esophageal varices (Downhill varices).
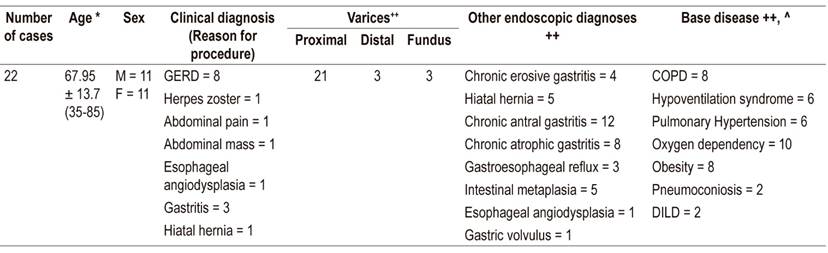
* Average age in completed years, standard deviation (range). F: Female, M: male, GERD: Gastroesophageal reflux disease, COPD: chronic obstructive pulmonary disease, DILD: diffuse interstitial lung disease.
Case 2
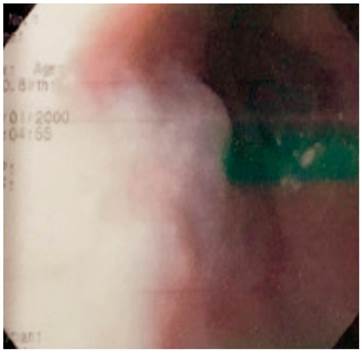
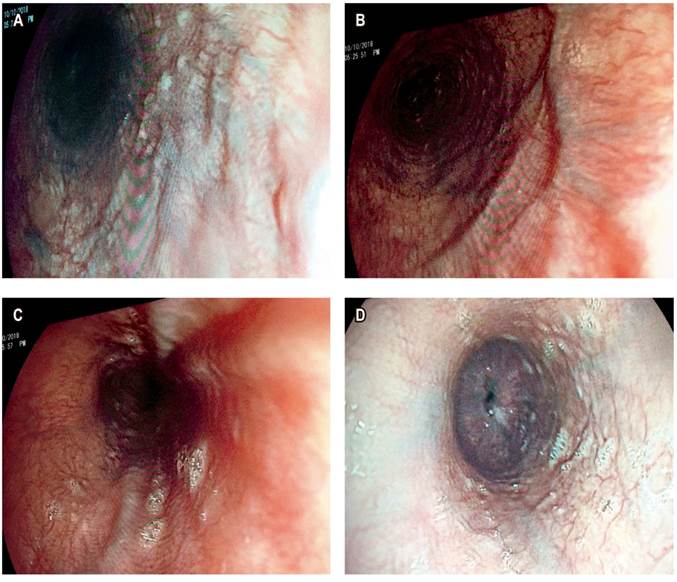
AJOC was a 48-year-old woman who was referred because of a diagnosis of gastroesophageal reflux disease (GERD). She had undergone bariatric surgery (gastric sleeve) two years earlier due to moderate obesity, suffered from severe asthma and sleep apnea. Moderate obesity-associated obstructive sleep apnea-hypopnea syndrome (OSAHS) had been partially corrected with continuous positive airway pressure (CPAP). A Hakim ventriculoatrial shunt had been placed in the patient when she was 20 years old to treat pseudotumor cerebri. In 2010, esophagogastroduodenoscopy (EGD) found an upper esophageal varice (Figure 1). Obstructive venous pathology was ruled out as the upper esophageal varice persisted without stigmas of bleeding or risk until a follow-up in 2016.
Case 3
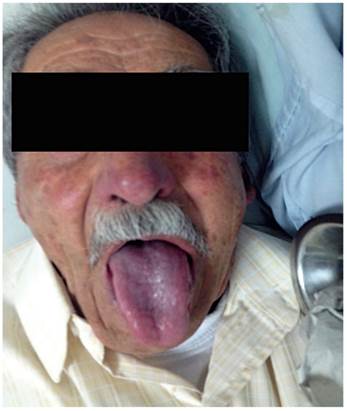
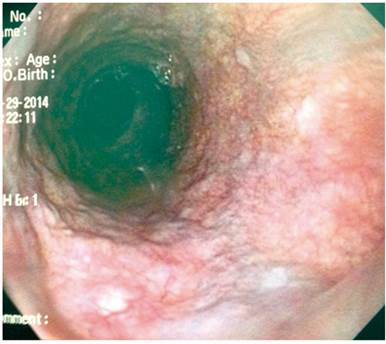
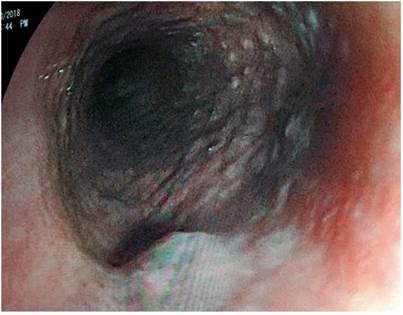
AMDA was a 73-year-old woman with a clinical diagnosis of GERD, a history of COPD from exposure to wood smoke, and a chronic user of inhalers and supplemental oxygen at home. At the time of the physical examination, she was obese, had cyanosis of the skin and mucosa, and suffered from bloating (Figure 2). An EGD found varices in the first 6 centimeters of her esophagus (Figure 3), but they were absent in the distal esophagus (Figure 4). There was no bleeding or stigmas, but she suffered from chronic superficial gastritis.
Case 8
JTP was an 82-year-old man for whom endoscopy was requested because of phlegm and symptoms of GERD. The patient had a 30 years history of exposure to organic solvents. A high definition chest CT scan found enlarged right cavities, bilateral superior centrilobular emphysema, and pulmonary honeycomb fibrosis. An echocardiogram found increased right chambers. He had pulmonary hypertension of 49 mm Hg. Portal Doppler was normal. He was using 18 h/d of oxygen, and a polysomnography showed severe apnea/hypopnea index of 35.9. He snored during 38% of his sleep time. EGD found upper esophageal varices without stigmas of bleeding (Figure 5).
Case 9
JAG was an 84-year-old man who had a 12 pack/year history of smoking and had been exposed to wood smoke in frequent fires in his job as a farmer. He suffered from dyspnea and bloating and had significant cyanosis of the skin and mucosa (Figure 6). In addition, he had chronic gastritis. An EGD found varices in the proximal 5 cm of the esophagus (Figures 7 and 8) but none in the middle and distal thirds. It also found grade B distal peptic esophagitis (Figure 9).
Case 21
JOMR was a 75-year-old man who had a history of COPD, was a 90 pack/years smoker, and was dependent on oxygen 24 h/d. He had dysphonia secondary to chronic laryngitis and presbylarynx, herpes zoster and suspicion of gastrointestinal occult neoplasia. An endoscopy found which proximal venous dilations (Figures 10 and 11).
General findings
There were 21 patients who had incidental diagnoses of proximal esophageal varices was incidental. Patients were almost equally divided by gender (11 men and 10 women) and their average age was 67.9 ± 13.7 years. Digestive endoscopy was performed primarily because of GERD (8/21), followed by chronic gastritis (3/21), and epigastric pain. An abdominal mass was found during one study (Tables 1 and 2).
Only three patients had varices in the distal third of the esophagus simultaneous with proximal esophageal varices. Another three had varices in the gastric fundus but did not have portal hypertension. Sixty percent of the patients were also diagnosed with chronic antral gastritis, 40% were found to have atrophic gastritis (and 25% were found to have hiatal hernias (Table 2).
The most common underlying disease was COPD which afflicted 40% of the cases. Six patients (29%) had pulmonary hypertension and another 10 patients (48%) probably had it given their clinical characteristics and associated diagnoses (Table 1). There were ten oxygen-dependent patients (48%), 40% of the patients had with moderate to severe obesity, 29% had sleep apnea, and 19% had diffuse interstitial lung disease.
Discussion
Epidemiology
The name downhill varices was coined by Felson in 1964 for the rare finding of upper esophageal varices. 1 Starting with three cases, Felson compiled case histories of 30 patients who had been described up to that time in the literature. The term is based on the occurrence of a reversal of venous flow in the upper esophageal veins downwards, as opposed to the upward flow in distal varices secondary to portal hypertension which are a frequent finding in endoscopy services.
A series of 2,368 cases of upper gastrointestinal bleeding reported a 0.1% incidence of upper esophageal varices (1 out of 908 patients with upper gastrointestinal bleeding). 3 Distal varices accounted for 10% to 30% of the causes of upper gastrointestinal bleeding. 4
Ayvaz et al. described 129 cases found incidentally among 25,680 endoscopies (0.5%). None were found because of bleeding. 2 Bleeding had occurred in only four of the cases described by Felson. 1. Similarly, none of the 11 subjects with proximal esophageal varices found by CT scans in a series of 36 patients developed superior vena cava syndrome (SVCS). 5
As these data indicate, the frequency of the disorder is very low. Endoscopic findings reported here are from second and third level diagnostic medical centers between January 1, 2011 and December 31, 2018. There were culled from a total of 73,896 endoscopies, so their frequency is only 2.8/10,000.
It is probable that the frequency of this disorder is higher since in the absence of clinical data some small and medium sized signs probably go unnoticed by endoscopists in the absence of digestive bleeding.
Clinical Presentation
The first descriptions found that this pathology was related to extrinsic compression of the SVC and were generally associated with mediastinal tumors which frequently have pulmonary origins or are due to lymphomas. 2,6
Nevertheless, subsequent publications about this condition described various pathologies including giant benign lymphomas, 7, mediastinal thymomas, 5,6,8 and intrathoracic goiters. 9-12 As the use of permanent intravascular devices for renal replacement therapy became frequent, secondary thrombosis of the SVC and its branches began to be described. As of now, more than one hundred cases have been reported. 5,13-26
Central catheters placed for other reasons also carry risks for development of intravascular thrombosis. Catheters are used for total parenteral nutrition (TPN), prolonged TPN in cases of short intestine, 27 chemotherapy for malignant diseases such as acute leukemia, 28 metastatic disease and other conditions. 2,29 The common denominator is SVC syndrome secondary to thrombosis of the SVC and its tributaries. This is caused by the presence of an intravascular foreign body that can include any type of foreign body such as transvenous pacemakers. 2,30
Complete vascular occlusion in the absence of mass or a device leads to the same results. This can occur in Castleman’s disease, 31 fibrosing mediastinitis, 32 Behcet’s disease, 33,34, systemic venulitis, 35 hypercoagulability due to Leiden factor V mutation, 36 autologous bone marrow transplantation with antiphospholipid syndrome, 37 and there has even been a case of congenital heart disease. 38
Of course, thrombosis of the SVC and obstruction of its branches produce the characteristic clinical syndrome in a significant number of cases and lead to diagnosis. However, in other cases the diagnosis begins with complications such as bleeding from esophageal varices and is made incidentally.
Mechanisms other than obstruction of the SVC or its branches can also lead to formation of superior esophageal varices. They include moderate to severe increases in central venous pressure due to pulmonary hypertension, double rheumatic mitral injuries, severe tricuspid regurgitation, 4 severe aortic stenosis with systolic hypertension of the right ventricle, severe pulmonary hypertension, 39 pulmonary hypertension and moderate tricuspid regurgitation, 2,3 and severe COPD. 2
Thus, our case series contributes additional important causes to the world’s literature. Only one of the patients studied here presented an obstruction to venous return. It was caused by mediastinal fibrosis and was a sequel to mediastinal lymphoma in adolescence (case 20) (Table 1).
Also, only one of the patients studied here had had a vascular device installed. The patient in case 2 had a Hakim valve installed when she was 20 years old. This patient did not present a vascular obstruction but did have a pathology that caused pulmonary hypertension, moderate obesity and moderate obesity-associated OSAHS. These conditions improved as a consequence of bariatric surgery, but the proximal varice persisted and was observed six years after its initial diagnosis and two years after the surgical procedure.
In our series, most of the patients were older adults (15/21: 71%), and men and women in this group were equally affected. Fifty-seven percent had lung diseases, and of these COPD was the most important. Only four such cases had been previously described in the literature. 2
Pneumoconiosis (mainly silicosis), pneumonitis due to organic solvents and DILD had not previously been reported as causes proximal varices, but they accounted for 19% of the cases in this series. All of these diseases compromise the lung parenchyma and cause permanent disorders of pulmonary circulation, progressive pulmonary hypertension, chronic cor pulmonale, and consequent permanent elevation of central venous pressure.
Obesity and obesity-associated OSAHS are two other previously unreported causes of proximal varices that are triggers of non-obstructive pulmonary hypertension. They were present in 38% and 29% of our cases, respectively. Only 29% of our cases had clinical diagnoses of pulmonary hypertension. Half of these were oxygen-dependent and the clinical appearance of two others included cyanosis, polycythemia, and bloating which suggested the disease (Figures 2 and 6). In addition, they probably also required supplemental oxygen.
Varices were incidental findings in all cases, and bleeding was not found in any of these cases (and had not been observed previously). These results are similar to those described in the 129 cases of Ayvaz et al. 2 as well as those reported by Siegel for 11 patients. 5
One of the limitations of our series is that no imaging studies were performed so that we could not systematically rule out the concomitant presence of mediastinal masses or vascular obstruction, except in case 2. Despite this, the patients did not clinically present SVCS or other symptoms that could cause suspicion of tumors or vascular lesions. Only one patient had been prophylactically anticoagulated due to primary pulmonary hypertension (case 14). Since this is a descriptive study of cases, we can only postulate causal associations.
Pathophysiology
The esophageal veins, the azygos, hemiazygos, and accessory hemiazygos veins, drain the SVC. In case of obstruction of the SVC distal to the entrance of the azygos, venous drainage of the upper extremities is performed from the inferior thyroid and mediastinal collateral veins to the hemiazygos, and from the azygos to the portal vein with cephalocaudal (downhill) flow. If the left gastric vein is crossed, varices occur throughout the esophagus.
When the obstruction of the SVC is above the entrance of the azygos to the proximal SVC or the brachiocephalic trunks or their branches, their collateral flow is also cephalocaudal and goes through the internal mammary, vertebral and deep collateral veins of the azygos as well as of the superior esophageal veins. In this way, the flow finds the path of the azygos towards the SVC distal to the obstruction and causes dilation only of the proximal and middle esophageal veins. 16
These varices do not frequently hemorrhage because they are not usually large and are located in the submucosa. 1-3,5 Consequently, they are less exposed to the trauma and peptic erosion that occur in lower esophageal varices with cephalad (uphill) blood flow given their subepithelial locations. 4 In addition, these lower esophageal varices are thrombocytopenia and coagulation disorders and are frequently found in patients with portal hypertension.
Treatment
Treatment of this pathology should always focus on its cause and can include surgical excision of mediastinal neoplasia, 11 surgical excision of intrathoracic goiter, 9-11 or surgical correction of heart disease. 38 Treatment generally creates conditions leading to the disappearance of varicose veins. Immunosuppressive therapy is used for Behcet’s disease and systemic venulitis, 33,34,35 and anticoagulation treatment is used for coagulation disorders. 8,36,37 Similarly, chemotherapy or radiation therapy are indicated for of tumors. 2,7,28,29
These varices are most frequently found incidentally without any prior history of bleeding as shown by the largest published series by Ayvaz et al. which had 129 patients as well as the series of 11 patients by Siegel. 2,11 In Felson’s series, only four of 30 patients had bleeding varices. 1 Conservative management of lower esophageal varices is usually indicated, but study of the triggering cause is required and should determine treatment.
In the event of gastrointestinal bleeding, the treatment of choice is band ligation for as long as technically possible. 4,10,14,22-24,27 Sclerotherapy can also be used, especially when location in the upper esophageal sphincter (UES) makes band ligation impossible or when ligation is not available. (18, 21) Some cases require combined treatments. 41
Band ligation is preferred whenever possible since there have been descriptions of serious complications such as infarction of the spinal cord due to thrombosis of the vertebral collateral veins and fatal pulmonary embolism due to the material used in sclerotherapy. 40,42
Conclusions
Upper esophageal varices rarely cause upper gastrointestinal bleeding. Most commonly, they affect older adults without any gender predilection. In this series of cases, they were related to etiologies that had not previously been described in the literature such as obesity, obesity-associated OSAHS, and DILD (due to pneumoconiosis or pneumonitis caused by exposure to organic solvents).
Other frequent causes were COPD and pulmonary hypertension. In all cases, varices were incidental findings. This makes this series unique when compared to those in the indexed literature. The most frequent recurrent causes reported in the literature have been obstruction of the SVC due to a mediastinal tumor and thrombosis of the SVC associated with intravascular devices and hypercoagulable states.
REFERENCES
1. Felson B, Lessure AP. “Downhill” Varices of the Esophagus. Dis Chest. 1964;46:740-6. https://doi.org/10.1378/chest.46.6.740 [ Links ]
2. Ayvaz MA, Rakici H, Allescher HD. Are Downhill Varices an Overlooked Entity of Upper Gastrointestinal Bleedings? Gastroenterol Res Pract. 2018;2018:7638496. https://doi.org/10.1155/2018/7638496 [ Links ]
3. Areia M, Romãozinho JM, Ferreira M, Amaro P, Freitas D. “Downhill” varices. A rare cause of esophageal hemorrhage. Rev Esp Enferm Dig. 2006;98(5):359-61. https://doi.org/10.4321/S1130-01082006000500006 [ Links ]
4. Harwani YP, Kumar A, Chaudhary A, Kumar M, Choudeswari PR, Kankanala VV, et al. Combined uphill and downhill varices as a consequence of rheumatic heart disease: a unique presentation. J Clin Exp Hepatol. 2014;4(1):63-65. https://doi.org/10.1016/j.jceh.2013.10.003 [ Links ]
5. Siegel Y, Schallert E, Kuker R. Downhill esophageal varices: a prevalent complication of superior vena cava obstruction from benign and malignant causes. J Comput Assist Tomogr. 2015;39(2):149-52. https://doi.org/10.1097/RCT.0000000000000183 [ Links ]
6. Subramaniam R, Madanagopalan N, Krishnan KT, Padmanabhan C. A case of anaplastic bronchogenic carcinoma with “downhill varices” of the esophagus. Dis Chest . 1967;51(5):545-9. https://doi.org/10.1378/chest.51.5.545 [ Links ]
7. Shirakusa T, Iwasaki A, Okazaki M. Downhill esophageal varices caused by benign giant lymphoma. Case report and review of downhill varices cases in Japan. Scand J Thorac Cardiovasc Surg. 1988;22(2):135-8. https://doi.org/10.3109/14017438809105944 [ Links ]
8. Inoue Y, Sakai S, Aoki T. Downhill oesophageal varices resulting from superior vena cava graft occlusion after resection of a thymoma. Interact Cardiovasc Thorac Surg. 2013;17(3):598-600. https://doi.org/10.1093/icvts/ivt212 [ Links ]
9. Bédard EL, Deslauriers J. Bleeding “downhill” varices: a rare complication of intrathoracic goiter. Ann Thorac Surg. 2006;81(1):358-60. https://doi.org/10.1016/j.athoracsur.2004.08.020 [ Links ]
10. Ibis M, Ucar E, Ertugrul I, Boyvat F, Basar O, Ataseven H, et al. Inferior thyroid artery embolization for downhill varices caused by a goiter. Gastrointest Endosc. 2007;65(3):543-5. https://doi.org/10.1016/j.gie.2006.10.005 [ Links ]
11. van der Veldt AA, Hadithi M, Paul MA, van den Berg FG, Mulder CJ, Craanen ME. An unusual cause of hematemesis: Goiter. World J Gastroenterol. 2006;12(33):5412-5415. https://doi.org/10.3748/wjg.v12.i33.5412 [ Links ]
12. Mönkemüller K, Poppen D, Feldmann K, Ulbricht LJ. Downhill varices resulting from giant intrathoracic goiter. Endoscopy. 2010;42 Suppl 2:E40. https://doi.org/10.1055/s-0029-1215290 [ Links ]
13. Pop A, Cutler AF. Bleeding downhill esophageal varices: a complication of upper extremity hemodialysis access. Gastrointest Endosc. 1998;47(3):299-303. https://doi.org/10.1016/S0016-5107(98)70331-1 [ Links ]
14. Hussein FA, Mawla N, Befeler AS, Martin KJ, Lentine KL. Formation of downhill esophageal varices as a rare but serious complication of hemodialysis access: a case report and comprehensive literature review. Clin Exp Nephrol. 2008;12(5):407-415. https://doi.org/10.1007/s10157-008-0055-4 [ Links ]
15. Froilán C, Adán L, Suárez JM, Gómez S, Hernández L, Plaza R, et al. Therapeutic approach to “downhill” varices bleeding. Gastrointest Endosc. 2008;68(5):1010-2. https://doi.org/10.1016/j.gie.2008.02.041 [ Links ]
16. Blam ME, Kobrin S, Siegelman ES, Scotiniotis IA. “Downhill” esophageal varices as an iatrogenic complication of upper extremity hemodialysis access. Am J Gastroenterol. 2002;97(1):216-8. https://doi.org/10.1016/S0002-9270(01)03979-X [ Links ]
17. Gessel L, Alcorn J. Variants of varices: is it all “downhill” from here? Dig Dis Sci. 2015;60(2):316-9. https://doi.org/10.1007/s10620-014-3501-z [ Links ]
18. Gebreselassie A, Awan A, Yaqoob H, Laiyemo A. Superior Vena Cava Obstruction: A Rare Cause of Recurrent Esophageal Variceal Bleeding. Cureus. 2018;10(2):e2226. https://doi.org/10.7759/cureus.2226 [ Links ]
19. Gopaluni S, Warwicker P. Superior vena cava obstruction presenting with epistaxis, haemoptysis and gastro-intestinal haemorrhage in two men receiving haemodialysis with central venous catheters: two case reports. J Med Case Rep. 2009;3:6180. https://doi.org/10.1186/1752-1947-3-6180 [ Links ]
20. Muthyala U, Philipneri MD, Hussein FA, Lentine KL. Recognition of downhill esophageal varices in hemodialysis patients requires a high index of clinical suspicion. Clin Exp Nephrol . 2009;13(6):677-8. https://doi.org/10.1007/s10157-009-0204-4 [ Links ]
21. Ontanilla Clavijo G, Trigo Salado C, Rojas Mercedes N, Caballero Gómez JA, Rincón Gatica A, Alcívar-Vasquez JM, et al. Downhill varices: an uncommon cause of upper gastrointestinal bleeding. Rev Esp Enferm Dig . 2016;108(7):440-442. https://doi.org/10.17235/reed.2016.3697/2015 [ Links ]
22. Pillai U, Roopkiranjot K, Lakshminarayan N, Balabhadrapatruni K, Gebregeorgis W, Kissner P. Downhill varices secondary to HeRO graft-related SVC syndrome. Semin Dial. 2013;26(5):E47-9. https://doi.org/10.1111/sdi.12078 [ Links ]
23. Raghavapuram S, George N, Girotra M, Siddique S, Tharian B. Downhill esophageal varices: unusual cause of hematemesis. VideoGIE. 2017;2(9):231-232. https://doi.org/10.1016/j.vgie.2017.02.005 [ Links ]
24. Berkowitz JC, Bhusal S, Desai D, Cerulli MA, Inamdar S. Downhill Esophageal Varices Associated With Central Venous Catheter-Related Thrombosis Managed With Endoscopic and Surgical Therapy. ACG Case Rep J. 2016;3(4):e102. https://doi.org/10.14309/crj.2016.75 [ Links ]
25. Loudin M, Anderson S, Schlansky B. Bleeding ‘downhill’ esophageal varices associated with benign superior vena cava obstruction: case report and literature review. BMC Gastroenterol. 2016;16(1):134. https://doi.org/10.1186/s12876-016-0548-7 [ Links ]
26. Nayudu SK, Dev A, Kanneganti K. “Downhill” Esophageal Varices due to Dialysis Catheter-Induced Superior Vena Caval Occlusion: A Rare Cause of Upper Gastrointestinal Bleeding. Case Rep Gastrointest Med. 2013;2013:830796. https://doi.org/10.1155/2013/830796 [ Links ]
27. Lim EJ, Stella DL, Russell DM. Torrential upper gastrointestinal bleeding from ‘downhill’ oesophageal varices complicating long term central venous access for total parenteral nutrition. Frontline Gastroenterol. 2010;1(2):118-120. https://doi.org/10.1136/fg.2010.001354 [ Links ]
28. Yeung AK, Guilcher GM, deBruyn JC. Conservative Management of Downhill Esophageal Varices Secondary to Central Line-related Thrombosis After Hematopoietic Stem Cell Transplant. J Pediatr Hematol Oncol. 2015;37(7):e424-6. https://doi.org/10.1097/MPH.0000000000000373 [ Links ]
29. Yasar B, Abut E. A case of mediastinal fibrosis due to radiotherapy and ‘downhill’ esophageal varices: a rare cause of upper gastrointestinal bleeding. Clin J Gastroenterol. 2015;8(2):73-6. https://doi.org/10.1007/s12328-015-0555-1 [ Links ]
30. Basar N, Cagli K, Basar O, Sen N, Gurel OM, Akpinar I, et al. Upper-extremity deep vein thrombosis and downhill esophageal varices caused by long-term pacemaker implantation. Tex Heart Inst J. 2010;37(6):714-716. [ Links ]
31. Serin E, Ozer B, Gümürdülü Y, Yildirim T, Barutçu O, Boyacioglu S. A case of Castleman’s disease with “downhill” varices in the absence of superior vena cava obstruction. Endoscopy . 2002;34(2):160-2. https://doi.org/10.1055/s-2002-19840 [ Links ]
32. Basaranoglu M, Ozdemir S, Celik AF, Senturk H, Akin P. A case of fibrosing mediastinitis with obstruction of superior vena cava and downhill esophageal varices: a rare cause of upper gastrointestinal hemorrhage. J Clin Gastroenterol. 1999;28(3):268-70. https://doi.org/10.1097/00004836-199904000-00021 [ Links ]
33. Orikasa H, Ejiri Y, Suzuki S, Ishikawa H, Miyata M, Obara K, et al. A case of Behçet’s disease with occlusion of both caval veins and “downhill” esophageal varices. J Gastroenterol. 1994;29(4):506-10. https://doi.org/10.1007/BF02361251 [ Links ]
34. Ennaifer R, B’chir Hamzaoui S, Larbi T, Romdhane H, Abdallah M, Bel Hadj N, et al. Downhill oesophageal variceal bleeding: A rare complication in Behçet’s disease-related superior vena cava syndrome. Arab J Gastroenterol. 2015;16(1):36-8. https://doi.org/10.1016/j.ajg.2015.02.003 [ Links ]
35. Maton PN, Allison DJ, Chadwick VS. “Downhill” esophageal varices and occlusion of superior and inferior vena cavas due to a systemic venulitis. J Clin Gastroenterol. 1985;7(4):331-7. https://doi.org/10.1097/00004836-198508000-00013 [ Links ]
36. Gómez-Aldana AJ, Gómez-Zuleta. Varices esofágicas en Downhill secundarias a trombosis de vena cava superior por déficit de factor V. Rev Gastroenterol Mex. 2017;82(2):179-180. https://doi.org/10.1016/j.rgmx.2016.04.007 [ Links ]
37. Vorlop E, Zaidman J, Moss SF. Clinical challenges and images in GI. Downhill esophageal varices secondary to superior vena cava occlusion. Gastroenterology. 2008;135(6):1863, 2158. https://doi.org/10.1053/j.gastro.2008.10.069 [ Links ]
38. Malloy L, Jensen M, Bishop W, Divekar A. “Downhill” esophageal varices in congenital heart disease. J Pediatr Gastroenterol Nutr. 2013;56(2):e9-11. https://doi.org/10.1097/MPG.0b013e31824b5fff [ Links ]
39. Gholam S, Ghazala S, Pokhrel B, Desai AP. A Rare Case of Downhill Esophageal Varices in the Absence of Superior Vena Cava Obstruction. Am J Gastroenterol. 2017;112(3):413. https://doi.org/10.1038/ajg.2016.489 [ Links ]
40. Heller SL, Meyer JR, Russell EJ. Spinal cord venous infarction following endoscopic sclerotherapy for esophageal varices. Neurology. 1996;47(4):1081-5. https://doi.org/10.1212/WNL.47.4.1081 [ Links ]
41. Nguyen LP, Sriratanaviriyakul N, Sandrock C. A Rare but Reversible Cause of Hematemesis: “Downhill” Esophageal Varices. Case Rep Crit Care. 2016;2016:2370109. https://doi.org/10.1155/2016/2370109 [ Links ]
42. Tsokos M, Bartel A, Schoel R, Rabenhorst G, Schwerk WB. Fatal pulmonary embolism after endoscopic embolization of downhill esophageal varix. Dtsch Med Wochenschr. 1998;123(22):691-5. https://doi.org/10.1055/s-2007-1024039 [ Links ]
Received: March 11, 2019; Accepted: July 29, 2019











 texto en
texto en