The importance of a healthy lifestyle for breast cancer prevention in women is well established in the literature 1 and almost 30% of breast cancer cases worldwide could be prevented with weight control, adequate nutrition, and physical activity 2-4. It is estimated that in Brazil 21.3% of breast cancer cases and 22% of deaths are attributable to lifestyle-related risk factors 5. The late recurrence can be associated with the lifestyle 6.
World agencies have dedicated to defining guidelines for cancer prevention and recurrence 7-9 and reinforce that women who follow these recommendations have a reduction of 13% to 60% in breast cancer risk 7. The adoption of a healthy lifestyle is the most effective line of action to prevent recurrence, especially in low- and middle-income countries 5, but it requires personal commitment and effective public policies 10.
Women with breast cancer are predisposed to dietary experiences with a focus on self-care, but treatment related effects could influence the consumption of unhealthy foods and contribute to weight gain observed in this population 11, and to the distancing from cancer prevention recommendations 7,9. As such, our aim was to assess the main patterns of adherence to the cancer prevention guidelines proposed by the 2018 World Cancer Research Fund/American Institute for Cancer Research (WCRF/AICR) by breast cancer surviving patients.
METHODS
Study Population and Data Collection
A cross-sectional study was conducted with 100 women diagnosed with clinical stage I-IV breast cancer, older than 20 years, treated at a reference centre in oncology from 2010 to 2011, who were consecutively and non-probabilistically selected. Patients with restrictive diets, those diagnosed with a neoplasm in another cancer site other than the breast, and/or those who could not answer the questionnaires were not included.
Sociodemographic and clinical data were obtained by searching the medical records of each patient and through interviews. Weight and height were measured on a platform weighing scale with attached stadiometer 12. Body mass index (BMI: kg/m2) was calculated and the patients were classified as malnourished, normal weight, overweight or obese 13,14. The elderly women were classified as thin, normal weight, and overweight 15. The waist circumference (WC) was measured at midpoint between the last rib and the iliac crest 14, considering the WC measurement ≥88cm as high risk for metabolic diseases 16.
Food consumption was investigated using the Quantitative Food Frequency Questionnaire (QFFQ), validated for northeast Brazilian women 17, consisting of 68 food items and home utensils typically used by the population, as well as a photo album showing food servings, when the instrument was applied. Then, we calculated the daily consumed amount of each food item in grams or milliliters of each item of the QFFQ.
Assessment of adherence to WCRF/AICR guidelines
We used 6 out of the 10 recommendations by WCRF/ AICR 7: having a healthy weight; having a diet rich in whole grains, vegetables, fruits and beans; limiting the consumption of fast food and other processed foods rich in fats, starches and sugars; limiting the consumption of red and processed meats; limiting the consumption of sugary drinks, and limiting the consumption of alcoholic beverages. To assess adherence to these recommendations the food items in the QFFQ instrument were grouped according to the consumption recommendations. In order to assess how much was consumed of the food mentioned in each recommendation per patient, the daily intake in grams and or milliliters of all component foods in each recommendation was added. Each food item was included in only one recommendation group, even when it had characteristics that indicated its allocation in more than one group. To define whether the patient's consumption followed the one proposed by the recommendations, the cut-off points proposed by the WCRF/ AICR Third Expert Report 2018 7 were used, considering “adherence” when consumption followed the recommended amounts, and “lack of adherence” when the consumption did not follow it.
We expanded the assessment using the WCRF/AICR 2018 Score 18, where a score is assigned to each prevention recommendation, which can vary from 0 to 1, and the maximum value indicates that there is total adherence to the recommendations and the value of 0 (zero) indicates that there is a lack of adherence. In the present study, as we chose to work with only 6 recommendations regarding food and weight management, we considered a total range of scores from 0 to 6.
Statistical Analysis
The association of sociodemographic and anthropometric variables with adherence to the WCRF/AICR recommendations was tested using Pearson's X2 test. The relationship between the total score of adherence to the recommendations and the anthropometric variables (weight, BMI and WC) was tested using Spearman's correlation coefficient.
To analyze the identification of the patterns of adherence to the WCRF/AICR guidelines 7, the recommendation score related to the BMI, consumption of fruits and vegetables, total fiber, calories from ultra processed foods and sugary drinks was used. We used the Principal Component Factor (pCF) analysis method, followed by orthogonal varimax rotation. The adequacy of the data to the factor analysis was confirmed using the Kaiser-Meyer-Olkin (KMO) coefficient and the Bartlett sphericity test. Each principal component was interpreted based on recommendations with factor loads ≥0.3 or ≤-0.3. Inside a component, negative charges indicate an inverse association of the item and positive charges indicate a direct association. For each identified pattern, the factor scores of the assessed women were generated.
Differences between mean weight, BMI and total scores of adherence to the recommendations between patients in the highest (Q4) and in the lowest quartile (Q1) of the patterns of adherence to the recommendation were calculated using the Student’s t test. The level of significance was set at 5%. Statistical analyses were performed using Stata software, version 13 and SpSS, version 20.0. The project was approved by the Research Ethics Committee of University of Fortaleza (n. 204/10) and all procedures were in accordance with the ethical standards of the Declaration of Helsinki 19.
RESULTS
The patients’ mean age was 51 (10.1) years, with most of them being over 50 years old (53.0%), whose income was below 1 minimum wage (63.0%), living without a partner (61.2%) and with less than 9 years of study (90.5%). Most women were at stage III or IV of the disease (73.9%). According to the anthropometric data, 76.0% of the patients had excess weight (overweight/obesity), with an average BMI of 29 (4.42) kg/m2; elevated WC was identified in most women (94.4%), with an average of 99 (10.8) cm (Table 1).
Table 1 Patients’ sociodemographic and anthropometric profile and association with adherence to the 2018 WCRF/AICR recommendations
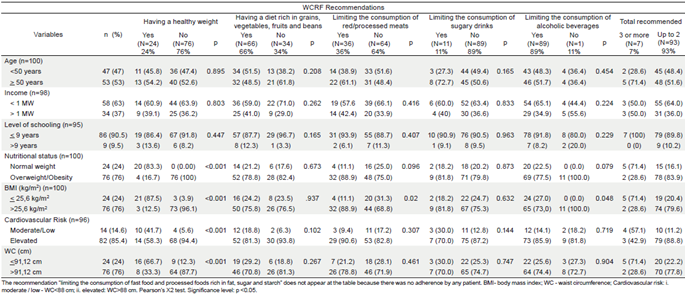
Most patients adhered to the recommendation of having a diet rich in grains, vegetables, fruits, and beans (66.0%) and limiting alcohol intake (89.0%). Only a small portion of the studied group adhered to the recommendations of having a healthy weight (26.0%), limiting the consumption of red and processed meats (36.0%), and limiting the consumption of sugary drinks (11.0%). None of the participants followed the recommendation of limiting the consumption of fast and processed foods rich in fat, sugar, and starch (Figure 1). The patients adhered to an average of 2.3 (0.92) recommendations and 93.0% adhered to 2 recommendations or fewer (Table 1).
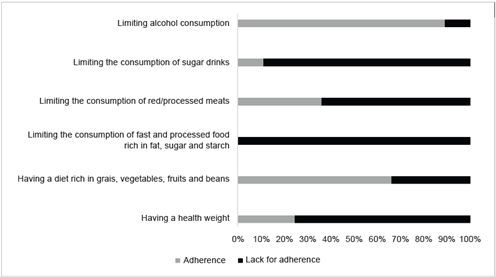
WCRF/AICR: World Cancer Research Fund/ American Institute for Cancer Research.
Figure 1 Prevalence of adherence and lack of adherence to the 2018 WCRF/AICR recommendations
Adherence to the recommendation of having a healthy weight was associated with the patients' nutritional status (p<0.001), being in the lowest BMI quartile (p<0.001), having moderate to low cardiovascular risk (p<0.001), and having WC<91.1 cm (p<0.001). Limiting the consumption of red and processed meats showed a direct association with being in the lowest BMI quartile (p=0.02). Following fewer than two recommendations was directly associated with the overweight/obesity nutritional status (p<0.0001), BMI>25.6 kg/m2 (p=0.002), high cardiovascular risk (p=0.001) and WC>91.1 cm (p=0.004). Adherence to the recommendations showed no association with age, income, and level of schooling (Table 1).
The patients scored an average of 3.6 (0.92) out of a total of 6 scores of adherence to the recommendations. Among the assessed recommendations, the one with the highest average score was limiting alcohol consumption with 0.95 (0.16) scores. The one with the lowest average was having a healthy weight, which adds the BMI score (0.21+0.20) and WC (0.04+0.11). There was an inverse correlation between the total scores of adherence to the recommendations with weight (r:-0.274; p=0.006), BMI (r:-0.371; p<0.001), and WC (r:-0.351; p<0.001).
Two main patterns of adherence to the WCRF/AICR guidelines were identified, the first being named 'grains/ fruits/fiber' and represented by adherence to having a healthy BMI to the diet rich in grains, vegetables, fruits, and beans and to the total fiber; and a second pattern was named ‘fast food/sugar’, characterized by adherence to the BMI, limiting the consumption of fast food and other processed foods high in fat, sugar and starch, and limiting the consumption of sugary drinks. The grain/fruit/fiber pattern explained 31.9% and ‘fast food/sugar’ explained 30.6% of the total variance of adherence to the recommendations. In the second pattern (fast food/sugar), we found adherence to the BMI recommendation with a stronger factor load than in the grain/fruit/fiber pattern (Table 2). Lower weight, BMI, and higher score of adherence to the recommendations were found in patients at the highest quartile, both in the grain/fruit/fiber and fast food/sugar patterns (Table 3).
Table 2 Patterns of adherence to the 2018 WCRF/AICR recommendations and factorial loads
| Adherence scores | Patterns of adherence to the recommendations and factorial loads | |
|---|---|---|
| Grains/fruits/fiber | Fast food/sugar | |
| BMI score | 0.3317 | 0.4672 |
| Vegetable score | 0.8601 | 0.079 |
| Fiber score | 0.8547 | -0.1947 |
| Fast food score | -0.1191 | 0.8016 |
| Sugar score | -0.0428 | 0.7927 |
| Proportional variance (%) | 31.93 | 30.67 |
| Accumulated variance (%) | 31.93 | 62.59 |
| KMO Coefficient | 0.527 | |
BMI: Body Mass Index; KMO: Kaiser-Meyer-Olkin Coefficient.
Table 3 Characteristics of weight, BMI and adherence score according to the quartile categories of the adherence patterns to the 2018 WCRF/AICR recommendations
| Grains/fruits/fiber | Fast food/sugar | |||||
|---|---|---|---|---|---|---|
| Q1 | Q4 | p | Q1 | Q4 | p | |
| Weight | 66.91 (9.5) | 59.5 (8.2) | 0.005 | 73.84(13.1) | 62.07 (9.4) | 0.001 |
| BMI (kg/m2) | 29.04 (3.8) | 25.82 (2.8) | 0.001 | 31.53(4.24) | 26.59(3.21) | <0.001 |
| Total scores | 3,33 (0.69) | 4.07 (1.04) | 0.005 | 4.56 (0.75) | 2.67 (0.42) | 0.001 |
BMI: body mass index. Q1. 1st quartile of adherence to patterns; Q4: 4th quartile of adherence to patterns. Student’s t test for analysis of difference of means. Significance at P<0.05.
DISCUSSION
The present study investigated adherence to the 2018 WCRF/AICR cancer prevention guidelines by Brazilian women with breast cancer and it showed that 93.0% of them follow two or fewer guidelines. We identified two main patterns of adherence to the guidelines, related to ‘grains/fruits/fiber’ and ‘fast food/sugar’, which had an impact on the patients' weight and BMI. Women at the highest quartile of the patterns had lower weight and BMI. These findings suggest that, among the assessed women, adherence to cancer prevention guidelines was insufficient, and those with greater adherence showed better weight management and BMI.
Although they have already been diagnosed with the disease and are in a favorable moment for the adoption of healthier behaviors related to self-care 20, the participants of the present study did not show this improvement in their choices through adherence to prevention guidelines 21,22.
It is important to use the third WCRF report 7, because it presents new recommendations considering servings consumed, time and type of physical activity, consuming a diet rich in whole grains, vegetables, fruits and beans, and limiting the consumption of fast food and other processed foods rich in fats, starches and sugars. This last recommendation needs to be highlighted since research indicates a higher consumption of these foods and its relationship with the increase in overweight and obesity, in addition to cancer and other chronic diseases 23,24.
In Brazil, to the best of our knowledge, there have been no publications that evaluated women with breast cancer using the guidelines of the third report of the WCRF/ aICR 7, the adherence scores, and the evaluation using patterns that show adherence to different recommendations, combined according to the population’s behavior. A recent study with prostate cancer patients 25 has shown a lack of adherence to most of the WCRF/AICR recommendations. Despite its importance for assessing this lack of adherence by cancer survivors and strengthening the discussion about the need for a healthy lifestyle after the diagnosis, the study evaluates adherence to each recommendation independently without exploring the combination of recommendations and without considering the adherence score.
In patients with breast cancer 26,27 the risk of the disease was inversely proportional to the total scores, but this association did not appear when the guidelines were assessed individually, indicating that the combination of recommendations, or a pattern of recommendations, better reflects their lifestyle and its impact on the risk of the disease or its recurrence. In our study, the use of assessment by patterns of adherence allows a look at the combination of behaviors related to the patients' lifestyle, which converges with reality, given that the lifestyle demonstrates different behaviors, which compromise the health status when combined.
We verified that the fast food/sugar adherence pattern had a greater impact on the BMI score, and this suggests that the consumption of ultra processed and ready-to-eat foods may have a greater influence on the weight and, consequently, contribute to the long-term recurrence of the disease. Among breast cancer patients, the consumption of ultra processed products is responsible for 27.1% of the total calories ingested 28, which is above the average of that observed in the Brazilian adult population (19.5%) 29. Ultra processed foods contribute to weight gain due to their high caloric density, excessive amount of sugar, and fat in their composition and their palatability 29-31.
The grain/fruit/fiber pattern explains most of the total variability of adherence scores to the guidelines (31.9%), suggesting that patients consume more of these foods, which may occur because they represent a healthy eating pattern 11. However, its impact on the BMI is lower than that of the fast food/sugar pattern, suggesting that the consumption of healthy foods without adequate guidance can increase calorie intake and contribute to weight gain 11.
Regardless of the adherence pattern, being in the highest quartile of the two patterns implies lower weight and BMI. Elevated BMI and adiposity are well established in the literature as risk factors for breast cancer and its recurrence 21,22,32-34. The high BMI and the 10% increase in weight gain, 2 years after the diagnosis, are associated with a greater chance of breast cancer recurrence 34. Additionally, women with breast cancer who have excess weight, high BMI, WC, and body fat percentage (%), and do not adhere to the recommendation of having a healthy weight 35.
Obesity is a risk factor for breast cancer and body fat has an important relationship with the survival of patients with this disease 36. It is known that obesity is characterized by a chronic, low-intensity inflammation status, enhancing biological pathways that may explain the association between high adiposity and cancer recurrence 34.
Reaching this weight and BMI management requires adherence to the other guidelines regarding food consumption and physical activity, but the combination of two or three recommendations already allows positive impacts on this management. Nevertheless, it is essential to highlight those changes in lifestyle can be complex, especially when accompanied by the treatment side effects and emotional changes related to the diagnosis. Female survivors of breast cancer may be willing to build a new perspective of their lifestyle and contribute to their own treatment through appropriate food choices 20,32. Some limitations of our study need to be considered, such as the cross-sectional design that does not allow us to assess the causality between adherence to the guide- lines and disease development or its recurrence. Also, we did not assess the level of physical activity and this is an important recommendation for disease prevention and recurrence, given that physical activity is associated with a 27% reduction in the risk of mortality in female survivors of breast cancer 32.
Nevertheless, the study adds an important contribution to the literature by using the latest WCRF/AICR report, as well as the adherence scores proposed for researchers in the area, considering not only those who adhere or do not adhere, but deepening the analysis on the effect of this adherence, combining different recommendations, and finding behavior patterns related to this adherence based on the factor analysis by the principal components. We also emphasize that the use of the WCRF/AICR prevention guidelines must be included in the reality of low and middle-income countries as a way of preventing disease recurrence, minimizing costs with cancer treatment, and reducing mortality.














