Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Accesos
Accesos
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en
SciELO
Similares en
SciELO -
 Similares en Google
Similares en Google
Compartir
Revista colombiana de Gastroenterología
versión impresa ISSN 0120-9957
Rev Col Gastroenterol vol.28 no.1 Bogotá ene./mar. 2013
Gastric varices: a challenge for endoscopic management
Wilmer J. Calderón N., MD. (1), Julián D. Martínez M. MD. (2), Daysi Rivera H. MD. (3), Renzo Pinto C. MD. (3), Marín A. Garzón O. MD. (3), Jorge I. Lizarazo R. MD. (3), Juan C. Marulanda G. MD. (3), Juan C. Molano V. MD. (3), Mario H. Rey T. MD. (3), Camilo Manrique M. MD. (3)
(1) Resident in Internal Medicine at the Hospital de La Samaritana and the Universidad de la Sabana
(2) Associate Professor at the Universidad Nacional de Colombia
(3) Gastroenterology Unit at the Hospital Universitario de La Samaritana
Received: 16-08-12 Accepted: 18-12-12
Abstract
Upper digestive tract bleeding due to gastric varices, although less common than bleeding secondary to esophageal varices, is one of the causes of high mortality in cirrhotic patients. Although band ligation is the optimal treatment for esophageal varices, its use for gastric varices is still hotly debated.
We report the case of an elderly woman with a history of hepatic cirrhosis secondary to nonalcoholic steatohepatitis (NASH) and obesity who was admitted to the hospital with upper digestive tract bleeding. An esophagogastroduodenoscopy showed an actively bleeding subcardial varice in the gastric fundus. The decision was made to manage the bleeding with rubber band ligation. The outcome was successful outcome, and the varice had disappeared in subsequent check-ups.
Key words
Gastric varices, bleeding, rubber band ligation.
CLINICAL CASE SUMMARY
A 71 year old woman was admitted after one day of abdominal pain, weakness and fainting. She had experienced hematemesis on two occasions and melena on 7 occasions. She reported a similar episode 3 months earlier at which time she had been hospitalized and had required a blood transfusion. Upon admission patient was found to be pale. Her blood pressure was 90/60 mmHg, she had tachycardia (110 pulses/minute) and her glucose level was 430mg/dl. Patient was dehydrated and a rectal examination showed melena.
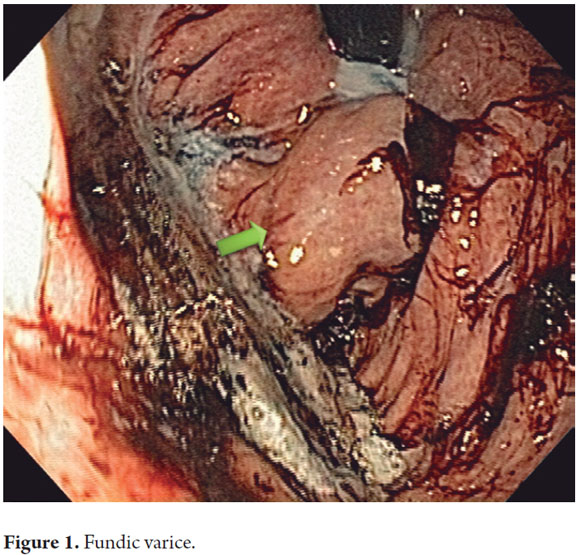
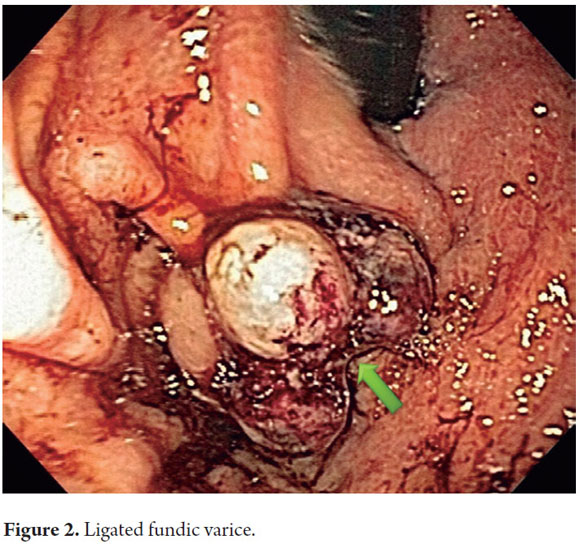
The patient had a background of diabetes mellitus type II which had been treated with diet and NPH insulin. She also had hepatic cirrhosis and grade II esophageal varices which had been diagnosed outside of our institution and were being treated with propranolol and spironolactone. It was decided to change management of patient to intravenous rehydration with saline solution to which was added terlipressin, an insulin infusion due to diabetes mellitus decompensation and a transfusion of 2 units of packed red blood cells. An emergency esophagogastroduodenoscopy was ordered. It found two bluish esophageal varices occupying less than 10% of the open esophageal diameter, but without any signs of bleeding. A prominent GOV 2 subcardial varice was found in the stomach with a blood stain on its surface (Figure 1). This varice was bound with a rubber band (Figure 2). Treatment with 1mg of terlipressin every 4 hours was continued for 5 days. Blood levels were monitored following 10.1 g/dl blood transfusion. After her metabolic acidosis resolved and her hyperglycemia was compensated, the patient improved and was discharged on her seventh day following admittance.
DISCUSSION
Patients with portal hypertension from any cause have gastric varices less frequently than esophageal varices. Gastric varices are found in between 5% and 33% of these cases (1). The incidence of bleeding secondary to rupture of gastric varices is approximately 25% within two years of diagnosis, and mortality rates range between 25% and 55%. Fundic varices bleed less frequently than those in other locations (2-4).
Risk factors that clearly increase the predisposition to bleeding from gastric varices are known and include size of the varice and the presence of stains or red dots on the surface of the varice. Varices larger than 10mm have a greater risk than those medium varices of between 5mm and 10 mm, and medium varices have greater risks than small varices of less than 5mm. The severity of hepatic dysfunction measured with the Child-Pugh scale is directly related to greater probability of hemorrhaging (4, 5).
Gastric varices are classified according to their relation with esophageal varices and to their location in the stomach (2, 3). Gastro-esophageal varices (GOV) are extensions of esophageal varices which are subclassified as Types 1 and 2.
- Type 1 (GOV 1), are those that extend throughout the lower curvature. They occur most frequently and treatment may be similar to that for esophageal varices.
- Type 2 (GOV 2) are those varices that extend throughout the gastric fundus. They are generally larger and twisting.
Isolated gastric varices (IGV) occur in the absence of esophageal varices and are subdivided into Type 1 and Type 2. Type 1 (IGV 1) are located in the gastric fundus and are generally twisting and complex. Type 2 (IGV 2) are found in the corpus and antrum, or at the pre pyloric level.
Stress on the gastric wall, called transmural pressure, is what determines whether or not ruptures occur. For this reason small increments in portal pressure can precipitate rupture (6). As with any bleeding, hypovolemic shock must be avoided through appropriate rehydration with intravenous liquids, blood transfusions and vasopressors if required to maintain adequate hemodynamic control.
Management of bleeding gastric varices constitutes a challenge for medical personal since there are no controlled clinical studies available in the literature with enough evidence to show the best method of treatment.
The management of Type 1 gastro-esophageal varices (GOV 1) which are extensions of esophageal varices should use a therapeutic approach similar to that for esophageal varices (rubber band ligation, sclerotherapy) (7).
For GOV 2, IGV 1, and IGV types of gastric varices, several reports have compared endoscopic techniques including intra-varice sclerotherapy with ethanolamine oleate, rubber band ligation, and intraluminal obturation with adhesive materials such as N-butyl cyanoacrylate, isobutyl2-cyanoacrylate or thrombin. Therapy with adhesive materials is the most effective for initial control of bleeding and has also demonstrated lower rates of rebleeding (6).
Some randomized studies that compare obturation of varices with N-butyl-cyanoacrylate with rubber band ligation for patients with bleeding gastric varices have shown that similar control of bleeding in both groups, but rebleeding occurred less often among patients treated with N-butyl-cyanoacrylate than among those treated with band ligation (23% vs. 47%) during 1.8 years of monitoring (8,9).
In the absence of adhesive agents or experience using them, a transjugular intrahepatic portosystemic shunt (TIPS) must be considered as the first option since it has been shown to control bleeding in 90% of patients for whom other techniques have failed (10).
Balloon retrograde transvenous obliteration (BRTO) is a technique which is used in Japan with satisfactory results. It consists of sclerotherapy of varices by means of a balloon catheter using fluoroscopic vision (11, 12).
Balloon tamponade is used as a temporary measure at the most severe moment of bleeding. If it fails the varice must be treated endoscopically or with a transjugular intrahepatic portosystemic shunt (TIPS).
TIPS are recommended in cases of bleeding fundic gastric varices which have not been controlled with a combination of pharmacological or endoscopic treatment. Nevertheless, they have high surgical risks. Evidence level B, class I (10, 13, 14).
Intra-varice thrombin injections are used infrequently. Studies show hemostasis in up to 94% of cases with low rates of rebleeding (15). This treatment is currently not included in the guidelines as ideal and therefore is recommended only as an alternative treatment.
The American Society of Gastrointestinal Endoscopy (ASGE) and the American Association for the Study of Liver Disease recommend the use of obliteration of varices with adhesive agents such as cyanoacrylate. They recommend TIPS as an alternate option for patients with high digestive tract hemorrhages due to gastric varices. Evidence level B, class I.
Analogues of vasopressin (terlipressin) and somatostatin (octreotide) show the same effectiveness for treating gastric varices as they do for treating esophageal varices since in both cases they decrease portal and collateral pressure (19). It should be clarified that this treatment is complementary to endoscopic treatment. Our patient was treated with terlipressin and ligation. This type of management is more accessible in our environment than are other treatments, and has good results.
1. Trudeau W, Prindiville T. Endoscopic injection sclerosis in bleeding gastric varices. Gastrointest Endosc 1986; 32: 264-268. [ Links ]
2. Sarin SK, Sachdev G, Nanda R, Misra SP, Broor SL. Endoscopic sclerotherapy in the treatment of gastric varices. Br J Surg 1988; 75: 747-750. [ Links ]
3. Sarin SK, Lahoti D, Saxena SP, Murthy NS, Makwana UK. Prevalence, classification and natural history of gastric varices: a long-term follow-up study in 568 portal hypertension patients. Hepatology 1992; 16: 1343-1349. [ Links ]
4. Kim T, Shijo H, Kokawa H, Tokumitsu H, Kubara K, Ota K, et al. Risk factors for hemorrhage from gastric fundal varices. Hepatology 1997; 25: 307-312. [ Links ]
5. Brocchi E, Caletti G, Brambilla G, Mantia LL, Lupinacci G, Pisano G, et al. North Italian Endoscopic Club for the Study and Treatment of Esophageal Varices. Prediction of the first variceal hemorrhage in patients with cirrhosis of the liver and esophageal varices. A prospective multicenter study. N Engl J Med 1988; 319: 983-989. [ Links ]
6. Young-suk L. Practical approach to endoscopic management for bleeding gastric varices. Korean J Radiol 2012; 13(S1): S40-S44. [ Links ]
7. Sarin SK, Jain AK, Jain M, Gupta R. A randomized controlled trial of cyanoacrylate versus alcohol injection in patients with isolated fundic varices. Am J Gastroenterol 2002; 97: 1010-1015. [ Links ]
8. Augustin S, González A, Genescà J. Acute esophageal variceal bleeding: Current strategies and new perspectives. World J Hepatol 2010; 2(7): 261-274 [ Links ]
9. Lo GH, Lai KH, Cheng JS, Chen MH, Chiang HT. A prospective, randomized trial of butyl cyanoacrylate injection versus band ligation in the management of bleeding gastric varices. Hepatology 2001; 33: 1060-1064. [ Links ]
10. Garcia-Tsao G, Sanyal AJ, Grace ND, Carey W. Prevention and management of gastroesophageal varices and variceal hemorrhage in cirrhosis. Hepatology 2007; 46: 922-938 [ Links ]
11. Hiraga N, Aikata H, Takaki S, Kodama H, Shirakawa H, Imamura M, et al. The long-term outcome of patients with bleeding gastric varices after balloon-occluded retrograde transvenous obliteration. J Gastroenterol 2007; 2: 663-672. [ Links ]
12. Ninoi T, Nishida N, Kaminou T, Sakai Y, Kitayama T, Hamuro M, et al. Balloon-occluded retrograde transvenous obliteration of gastric varices with gastro renal shunt: long-term follow-up in 78 patients. Am J Roentgenol 2005; 184: 1340-6. [ Links ]
13. Qureshi W, Adler DG, Davila R, Egan J, Hirota W, Leighton J, et al. ASGE Guideline: the role of endoscopy in the management of variceal hemorrhage, updated July 2005. Gastrointest Endosc 2005; 62: 651-655. [ Links ]
14. de Franchis R, Baveno V Faculty. Revising consensus in portal hypertension: report of the Baveno V consensus workshop on methodology of diagnosis and therapy in portal hypertension. J Hepatol 2010; 53: 762-768. [ Links ]
15. Przemioslo R, McNair A, Williams R. Thrombin is effective in arresting bleeding from gastric variceal hemorrhage. Dig Dis Sci 1999; 44: 778. [ Links ]











 texto en
texto en