Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Accesos
Accesos
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en
SciELO
Similares en
SciELO -
 Similares en Google
Similares en Google
Compartir
Revista colombiana de Gastroenterología
versión impresa ISSN 0120-9957
Rev Col Gastroenterol vol.34 no.2 Bogotá abr./jun. 2019
https://doi.org/10.22516/25007440.392
Original articles
Transanal minimally invasive surgery (TAMIS): technique and results of initial experience
1 Cirugía Gastrointestinal y Endoscopia. Jefe de Postgrado de Cirugía General, Universidad Pontificia Bolivariana; Grupo de Gastrohepatología, Universidad de Antioquia; Grupo de investigación clínico-quirúrgica, Universidad Pontificia Bolivariana; Instituto de Cancerología-Clínica las Américas. Medellín, Colombia
2 Cirujano General y Coloproctólogo, Profesor de Cirugía, Universidad Pontificia Bolivariana. Clínica las Américas. Medellín, Colombia
3 Cirujano General y Cirujano Oncólogo, Instituto de Cancerología en la Clínica las Américas. Profesor de Cirugía, Universidad Pontificia Bolivariana. Medellín, Colombia
4 Cirujano General. Universidad CES. Medellín, Colombia
Background:
Transanal endoscopic surgery, a recently described minimally invasive approach, provides superior exposure and access to the entirety of rectal lesions and has lower risks of compromising resection margins, lower recurrence rates and lower morbidity and mortality than do conventional transanal excision and endoscopic removals.
Objectives:
The aim of this study is to describe our initial experience and with minimally invasive transanal surgery (TAMIS) and its results in terms of complete resections and complications possibly related to the procedure.
Materials and methods:
This is a series of TAMIS cases with prospective follow-ups. We analyzed the results of 27 patients who underwent the procedure at several centers in Medellín, Colombia, between January 2012 and December 2016. Twenty patients had Single Incision Laparoscopic Surgery while the GelPOINT path transanal access platform was used for the other six patients. Laparoscope optics provide support for 16 procedures while the more recently introduced flexible endoscope supported eleven procedures.
Results:
Twenty-seven TAMIS procedures were performed and evaluated. Ten patients were women (37%), and 17 were men. On average, patients were followed up for 32 months, but none less than 12 months. Average patient age was 68 years (52 to 83 years). The average tumor size was 5.3 cm (2 to 9 cm) and the average distance from the anal margin was 7 cm (5 to 9 cm). Postoperative complications occurred in six cases (22%). In one case, a rectal perforation was corrected laparoscopically during the procedure. Another perforation was corrected by the same transanal route. A rectal stenosis was managed with digital dilatation, there was one case of minor rectal bleeding, one case of urinary retention and one patient developed advanced rectal cancer with a positive microscopic margin (4%) three months after resection. There were no readmissions. There were no deaths due to the intervention. Pathology reported low grade adenomas in three cases (11%), high grade adenomas in 11 cases (41%), in-situ adenocarcinoma in six cases (22%), neuroendocrine tumors in five cases (19%), and one case each of cicatricial fibrosis (4%) and leiomyoma (4%).
Limitations:
The results cannot be extrapolated to the general population because of the limited number of interventions and performance of procedures by only two authors.
Conclusions:
Our initial experience shows TAMIS to be a minimally invasive procedure with low postoperative morbidity which is curative for benign lesions and for selected patients with early cancer.
Keywords: Rectal adenoma; early rectal cancer; minimally invasive transanal surgery TAMIS
Antecedentes:
la cirugía transanal endoscópica es un abordaje mínimamente invasivo recientemente descrito, que provee una exposición superior y permite el acceso a las lesiones del recto en toda su extensión. Además, provee un riesgo menor de compromiso de los márgenes de resección, menores tasas de recurrencia y una menor morbimortalidad en comparación con la escisión transanal convencional o las remociones endoscópicas.
Objetivos:
se pretende describir la experiencia inicial y los resultados con la cirugía transanal mínimamente invasiva (transanal minimally invasive surgery, TAMIS) en términos de resecciones completas y posibles complicaciones relacionadas con el procedimiento.
Materiales y métodos:
esta una serie de casos con un seguimiento prospectivo de los pacientes con TAMIS. Se analizaron los resultados de 27 pacientes intervenidos en varios centros de Medellín, Colombia, entre enero de 2012 y diciembre de 2016, realizados con cirugía laparoscópica monopuerto (single-port laparoscopic surgery, SILS) (21 casos) o el GelPOINT® Path (6 casos), junto con el apoyo de la óptica del laparoscopio (16 pacientes) y del endoscopio flexible (11 pacientes).
Resultados:
se realizaron 27 TAMIS en el mismo número de pacientes, 10 mujeres (37 %) y 17 hombres fueron evaluados. Se realizó un seguimiento a los pacientes durante aproximadamente 12 meses, en promedio 32 meses. La edad promedio fue de 68 años (52-83 años). El tamaño promedio del tumor fue de 5,3 cm (2-9 cm) y la distancia promedio desde el margen anal fue de 7 cm (5-9 cm) Las complicaciones posoperatorias se dieron en 6 casos (22 %) Una perforación rectal se corrigió por vía laparoscópica en el mismo acto quirúrgico y otra por la misma vía transanal. Una estenosis rectal se manejó con dilatación digital, y hubo un caso de sangrado rectal menor, uno de retención urinaria y un paciente presentó un cáncer rectal avanzado a los tres meses de la resección con margen microscópico positivo (4 %). No hubo reingresos. La mortalidad por la intervención fue nula. La patología operatoria reportó la presencia de adenoma de bajo grado en 3 casos (11 %), de alto grado en 11 (41 %), adenocarcinoma in situ en 6 (22 %), tumor neuroendocrino en 5 pacientes (18 %), 1 caso de fibrosis cicatricial (4 %) y 1 de leiomioma (4 %).
Limitaciones:
los resultados no son extrapolables a la población general debido al poco número de intervenciones y la ejecución limitada a solo dos autores.
Conclusiones:
en nuestra experiencia inicial, TAMIS es un procedimiento mínimamente invasivo con una baja morbilidad posoperatoria, es curativa para lesiones benignas y para pacientes seleccionados con cáncer temprano.
Palabras clave: Adenoma rectal; cáncer rectal temprano; cirugía transanal mínimamente invasiva; TAMIS
Introduction
Screening programs, better equipment and more trained personnel have resulted in detection of a greater number of rectal lesions and, in the case of neoplasms, at earlier stages. Lesions in their stages pose the dilemma of choosing local excision or a radical procedure. The first transanal excisions using the Parks technique and retractor were laborious and limited to the distal 8 cm of the rectum. Since then microscopic, endoscopic and laparoscopic methods have modified transanal approaches. Still, many consider local excision to be sufficient for early lesions since it avoids the morbidity and mortality inherent in radical surgical procedures. 1,2
Transanal endoscopic microsurgery (TEM) is a minimally invasive technique originally conceived by Dr. Gerhard Buess in the 1980s to allow transmural resection of early rectal cancer (T1). 3 TEM reduces the rate of local recurrence below those of conventional transanal transanal excision, abdominoperineal resection (APR) and the Parks technique 4. TEM has less morbidity, shorter hospital stays, less postoperative pain during, and less patient time lost than does the Parks technique. 5
The arrival of the transanal endoscopic operation (TEO) represented a new higher level of complexity with new equipment and instruments and a new learning curve. For this reason, it has been performed mostly by a small group of experts in high-tech centers. Although they have performed a large number of procedures, even after 30 years, and despite the benefits it offers to patients with benign and malignant tumors of the rectum, TEM/TEO is not used on a large scale. 6
Since its introduction in 2009, 7 the TAMIS technique has been used with increasing frequency in Canada, the United States and Europe. 8-13 Recently, it has been presented in our country as an alternative to TEM for local resections of rectal tumors located in the middle and distal rectum. Initially, TAMIS became possible thanks to the development of the single port equipment and platforms for transanal surgery required by this technique. The use of a single transanal port device allows the use of conventional laparoscopic instruments, endoclamps and methods of advanced diverse coagulation (bipolar, harmonic, etc.).
Since its initial description, case reports and small series published about TAMIS have demonstrated that it is a technically possible and accessible alternative for most laparoscopic surgeons and has a lower initial cost than does TEM/TEO. In Latin America, the initial experiences with this method were published in Brazil by Alves et al. and Sevá-Pereira et al. although these authors included only 4 and 5 cases, respectively. 14,15
The purposes of this study are to show the initial local experience with TAMIS for lesions of the middle and lower rectum and to evaluate its feasibility, results and the safety of the intervention for at least one year following procedures.
Materials and methods
Prospective data about TAMIS treatment of patients with rectal lesions was collected from January 2012 to December 2016. Patients with diagnoses of adenomas or neuroendocrine tumors smaller than 2 cm were included, and patients with advanced rectal cancer were not included. As indicated in the National Comprehensive Cancer Network (NCCN) protocol, no routine MRI or CT scans were performed because of the conditions of T1 superficial lesions.
Two surgeons, Rodrigo Castaño and Juan Darío Puerta, performed all surgical procedures.
Mechanical intestinal preparation with enemas and prophylaxis with broad-spectrum antibiotics (second generation cephalosporins plus metronidazole) were performed prior to procedures. All surgery was performed under general anesthesia. In the first 12 procedures, patients were placed on the operating table in either lithotomy or jackknife surgical position depending whether the lesion’s location was posterior or anterior. In the last 15 cases, patients were placed in lithotomy position, regardless of the location of the lesion.
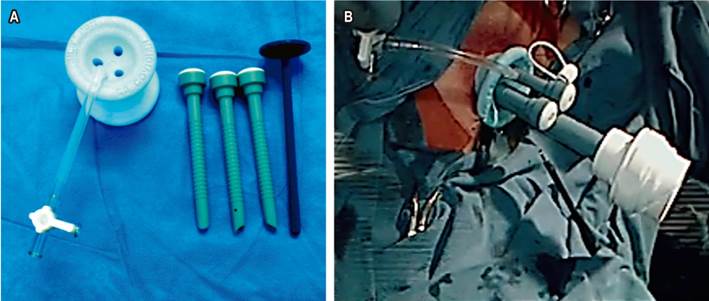
The SILS™ Port platform (Covidien-Medtronic, Minneapolis, MN) was used for the first dozen cases. It is made of a special thermoplastic elastomer which allows atraumatic adaptation of the kit to the anal canal. After properly lubricating the kit and the anal canal, the port was installed. Subsequently, a pneumoperitoneum was established with CO2 at a pressure of 12-15 mm Hg (Figure 1A and B).
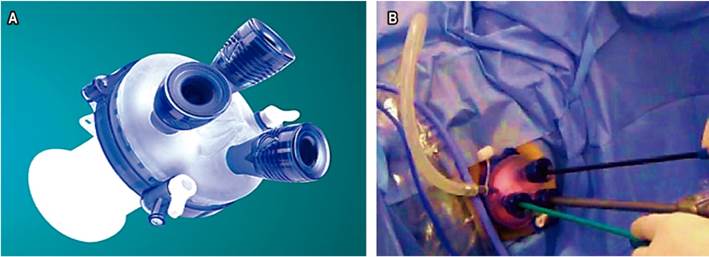
The GelPOINT® Path was used for the last 6 cases. Recently introduced by Applied Medical (Rancho Santa Margarita, CA), it is specifically designed for performance of TAMIS. Its placement mechanics are similar to those of the SILS ™ Port platform (Figure 2A and B).
A 10 mm laparoscopic camera with a 30º angle was used in most cases, but in 10 cases an upper endoscope was used because of the ease of washing the lens and the possibility of aspirating the smoke resulting from dissection. In addition to the 10 mm optics port, two other 5 mm ports were used for manipulation of laparoscopic instruments such as tweezers, electrocautery spatula, hooks and scissors.
Dissection begins by marking the periphery of the lesion, leaving a margin of at least 2 to 3 mm outside the edge of the lesion (Figure 3A). Next, a cut is made to expose the submucosa and the lower margin of the lesion is lifted (Figure 3B). Then, electrosurgery (Figure 3C) is used to perform total thickness resection (Figure 3D), aiming to obtain lesion free, 0.5 cm deep, lateral margins. In 21 cases, wound closure (Figure 3E) was performed through a continuous primary suturing using V-Loc ™ (Covidien) or STRATAFIX™ (Ethicon) absorbable barbed sutures (Figure 3F).
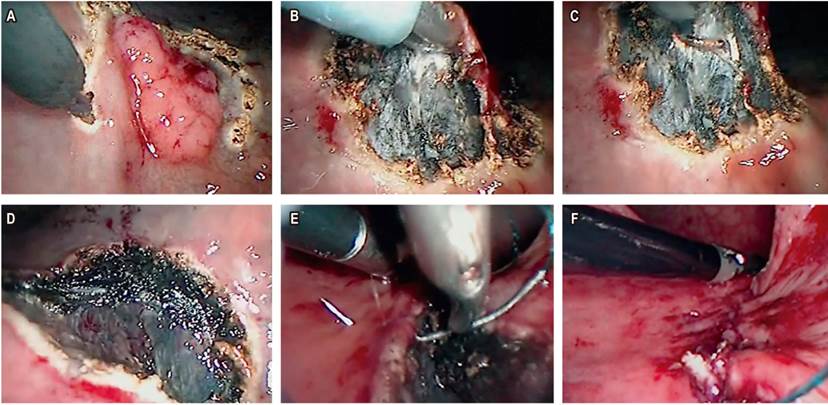
Figure 3 Sequence of events in the marking and resection of the total thickness of the rectal lesion. A. Marking the periphery of the lesion. B. Lifting lower margin. C. Transmural dissection of lesion. D. Complete excision of lesion. E. Suturing resection margins. F. Suture line with absorbable material.
Initially, all patients were hospitalized for one day. Those with more recent interventions and with small lesions were discharged the same day (except for patients with perforations whose hospital stay was 3 and 4 days). All immediate and late complications were recorded. All patients underwent rigorous follow-up at two, six and 36 weeks. When there was a diagnosis of cancer including invasive carcinoma according to NCCN guidelines, patients were referred to cancer management. Each of these patients underwent total colonoscopies, evaluation of carcinoembryonic antigen (CEA) levels, an abdominal-pelvic MRI, and a CT chest scan.
The principal aims in each case were to evaluate the procedure’s feasibility, the quality of the resected ion, and the patient’s oncological prognosis. The feasibility of the procedure is defined as resection by TAMIS without recourse to a different transanal approach to complete the procedure. Good quality of resected segment is determined by the absence of fragmentation or a negative margin, defined as ≥1 mm of the tumor margin. Secondary objectives were to determine the clinical prognosis and perioperative morbidity and mortality, classified according to the Clavien-Dindo system.
Results
TAMIS was performed successfully on 27 patients: 21 with SILS™ Port and six with GelPOINT® Path (22%). The lithotomy position was used in 24 cases, and the jackknife position was used in three cases (12%). Of the total patients, 10 were women (37%). The average age was 68 years (52-83 years) (Table 1).
Table 1 Characteristics of patients and lesions
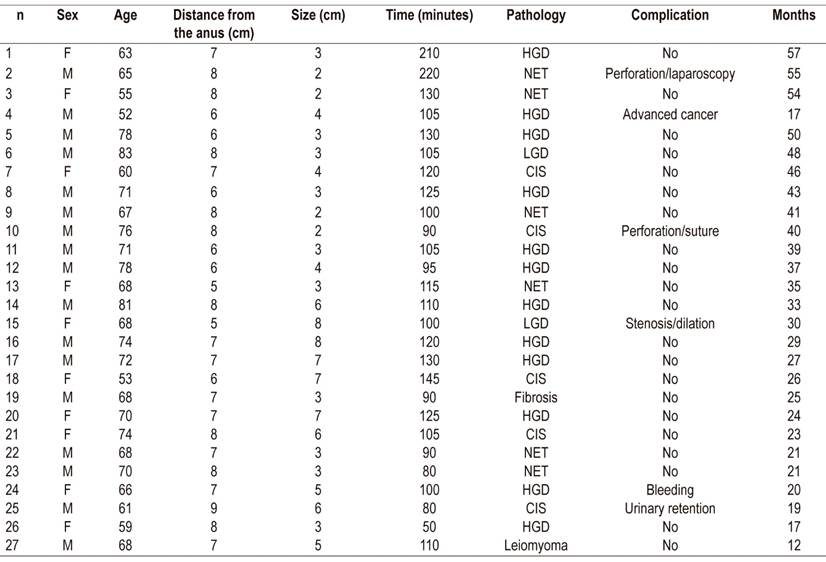
CIS: carcinoma in situ; HGD: high grade dysplasia; LGD: low grade dysplasia; NET: neuroendocrine tumor.
The distance from the lower limit of the lesion to the anal margin determined by preoperative rigid rectoscopy was 7.1 5-9 cm. The average surgical time was 115 (50-220) minutes. The average size of the lesions was 5.3 2-9 cm. Resection of total thickness was achieved in all cases, and only two segments were fragmented (2 fragments).
The operative pathology reports showed low grade adenomas in three patients (11%), high grade adenomas in 11 patients (41%), pT1N0 adenocarcinomas in situ in six (22%) cases, neuroendocrine tumors in five patients (18%), one case of local fibrosis (4%), and one case of leiomyoma (4%).
All tumors, except one (4%), were resected with negative microscopic resection margins. The extension studies of the patient in question showed extensive local, regional and distant compromises from interval colorectal cancer (I-CRC). Eighteen 18 months earlier, a colonoscopy’s results were negative for a tumor in the rectum.
Wounds were not closed in five cases (18%). These patients evolved without major developments similar to those whose wounds were closed. There was bleeding from only one of the wounds that was left open without suturing.
Two rectal perforations (8%) occurred: one in the second patient of the series, and the other in the 10th patient of the series. The first was corrected laparoscopically. The second perforation, which accessed the peritoneal cavity, was corrected by transanal suturing. There were no subsequent adverse events in the evolution of these patients.
Postoperative bleeding occurred and there were no infectious complications. No patient had to be reoperated. There was no mortality associated with the technique. The average duration of hospitalization was 1.1 days. The patients had no recurrence of lesions during average follow-up time of 33 months.
Discussion
By the middle of the first decade of this century, minimally invasive surgery pointed to an innovation: natural orifice transluminal endoscopic surgery (NOTES). 16 This route reduces traumatic access through the abdominal wall and looked like it might make it possible to dispense with it completely. This led to the appearance of multi-port laparoscopic access through the navel in so-called single-port surgery. 17 This stimulated the development and implementation of TAMIS, the concept, technique and initial prognosis of which was reported by Atallah et al. 7 It has since been validated by several authors from different medical centers. 18,19
Management of benign and malignant rectal tumors depends on a healthy balance between curative intent and preservation of functionality. TAMIS is a new platform for local resection of benign rectal lesions with malignant potential as well as well selected malignant lesions. Initial encouraging results have led significant increases in its use. 13 In this study, we report the first 27 cases of TAMIS performed for the treatment of premalignant or malignant rectal lesions. In all cases, it was possible to completely resect the rectal lesion without significant morbidity. This is true despite two perforations which entered the peritoneal cavity, but both were quickly corrected: the first by laparoscopy, and the second by direct suturing.
Transanal surgery was first performed with the Parks technique and had more recently been performed with the microscopic approach. Nevertheless, a number of authors consider TEM/TEO to have a significant degree of technical difficulty. 6 Fifteen years since the advent of this technique, the number of procedures performed by Buess had not exceeded 500. (20) Among the reasons for its limited use by expert surgeons were the initial investment associated with equipment acquisition, the need for special training, and the small sample of patients who benefit from the method. In contrast, only four years after the introduction of TAMIS, there are already reports of it being performed from 16 countries. 1
The evidence shows that, for selected patients with adenocarcinoma pT1N0, local resection with endoscopic microsurgery has rates of recurrence and survival similar to radical resections. In 2012, Lezoche et al. demonstrated that, in patients with cT2N0 rectal adenocarcinomas who received neoadjuvant treatment, an endoscopic microsurgery resection could be performed with results similar to those of total mesorectal resection in terms of recurrence and survival. 21 The indications for TAMIS are the same as those for TEM/TEO.
Until the last decade, the TEM and TEO platforms were the only ways to perform an endoscopic transanal resection. However, TEM and TEO are not available in many hospitals, and TAMIS has emerged as an advanced alternative with greater cost-effectiveness and with results that could be better than those of TEM/TEO in the future. This has already allowed for performance of minimally invasive treatment of rectal tumors at more medical centers. 2 In the United States, the cost of the ports required for the TAMIS platform is between $500.00 and $650.00, equivalent to the cost of materials used for CO2 insufflation with a TEM platform. 10
Room preparation for the procedure is quick, and it offers a 360 degree view rather than 220 degree view inside the rectal lumen. Moreover, conventional laparoscopic instruments are used. These advantages of TAMIS over TEM/TEO. In addition, patient placement is versatile and patients can be placed in the lithotomy position in all cases of TAMIS, which is an additional advantage.
Finally, TAMIS’ port diameter is only 30mm, 10 mm smaller than the TEM/TEO port. Due to TAMIS’ port design, dilation is safe and non-traumatic. In contrast, the TEM port is rigid, and it has been associated with anorectal dysfunction in prospective studies. Dysfunction has included reduction in resting pressure and decreases in voluntary contraction found at six week follow-up examinations. It is possible that sphincters dilate less during TAMIS than during TEM/TEO. 22 In 2014, Schiphorst et al. evaluated the functioning of the anal sphincter before and after performing TAMIS and found no manometric alterations. In addition, they found improvement in the fecal incontinence severity indexes of 37 patients who had undergone surgery thus demonstrating improvement in anorectal function after TAMIS. Of the 17 patients who had incontinence before surgery, fifteen improved, one remained the same, and the other worsened. 23
One of the main technical difficulties of TAMIS is occasional instability of insufflation which can lead to intermittent collapse of the rectal lumen thus hindering surgery. This event can be resolved, to a greater or lesser degree, by increasing pressure to 15-20 mm Hg, by greater relaxation, or by repositioning the port. As with TEM/TEO, another difficulty is related to release of smoke from electrocautery. The SILS ™ Port system’s 3 ports are all used by optical devices and surgical instruments, but the GelPOINT® Path has a special port expressly for smoke removal.
With respect to the technique’s limitations, one has established the importance of a support endoscope support to facilitate smoke aspiration, to allow lens washing, and to add pressure to maintain insufflation. With the retroversion, visual control of the proximal limit of the lesion and passage of the instruments through the working channel is facilitated. This has shown encouraging results in terms of the execution time and minor complications. 24,25 More recent descriptions combine submucosal endoscopic dissection with TAMIS to treat lesions of the lower rectum that compromise the dentate line. 26,27
Once the lesion has been removed, the dilemma of whether or not to close the rectal wound is raised. Some publications have described infectious complications such as abscesses after the closure of the wound. 28 A metaanalysis published in 2017 by Menahem et al. showed that there are no differences in terms of infection and reinterventions between patients whose wounds have been closed and those whose wounds have remained open. Another metaanalysis published by Lee et al. in 2018 suggests a higher incidence of clinically significant hemorrhaging in patients with open wounds (9% vs. 3%, p = 0.045). 29,30 In our study, wounds of 21 patients (81%) were closed. The tendency is to leave wider wounds open, and we only left the largest wounds open. They evolved with stenoses which were successfully managed with digital dilations.
In this study, positive margins were only observed on one resected specimen. This patient’s evolution was unexpected with extensive liver, lung and local and regional metastases from interval colorectal cancer. Pathological analysis showed tissue removed was fibrotic in only one case. In two cases, the specimen had fragmented, but the margins were not compromised, and there were no effects on patient evolution.
Increasing, reports of TAMIS with multiple disposable ports designed for single-port surgery are being published although this is still under evaluation.
Several issues need clarification including the viability of endoscopic transanal access for upper rectal procedures since the TAMIS platform does not include surgical rectoscopy. Its addition could theoretically provide stability to the surgical procedure at these sites.
In two cases, perforations that entered the peritoneal cavity occurred during surgery. The first was corrected with the support of laparoscopy performed by the authors while the second wound was properly closed using TAMIS. The data reveal that perforations of the rectum do not compromise the clinical or oncological prognoses of these patients. 31,32 Perforation of the rectum during removal of the complete thickness increases surgery time and causes minimal abdominal trauma but does not increase morbidity.
A study of 254 TAMIS procedures published in 2018 found that overall rate of positive margins (resection R1) was 7%, with an indication of malignancy of 57%. In TEM, an R1 rate of 10% is accepted, and in transanal resection the accepted rate is 26%. The authors conclude that TAMIS is a complex procedure that requires a minimum of 14 to 24 cases to achieve an acceptable R1 resection rate, shorter duration of surgery, and improvement in the diameters of resected lesions. 33
One of the limitations of these studies, including ours, is absence of quality of life evaluations. Fecal continence was not evaluated, although there are questionnaires such as the Fecal Incontinence Severity Index and the EuroQolEQ-5D. The latter has shown a better quality of life after TAMIS, presumably secondary to tumor removal. 34 The aforementioned questionnaires are easy for patients to use, are excellent tools for assessing anorectal function over time, 20 and can be incorporated into routine clinical follow-up in our center. Another limitation of these studies is the bias inherent in retrospective analyses due to lack of data in medical records. In contrast, our clinical and surgical data were complete since the data was collected prospectively. Sometimes, pathological records do not contain tumor dimensions, but margin analyses were well described. Finally, it is important to keep in mind that TAMIS is an evolving surgical technique and that samples in the published series are small so surgical results are subject to variations from center to center (Table 2).
Table 2 Comparisons between results of this study and series with more than 20 patients
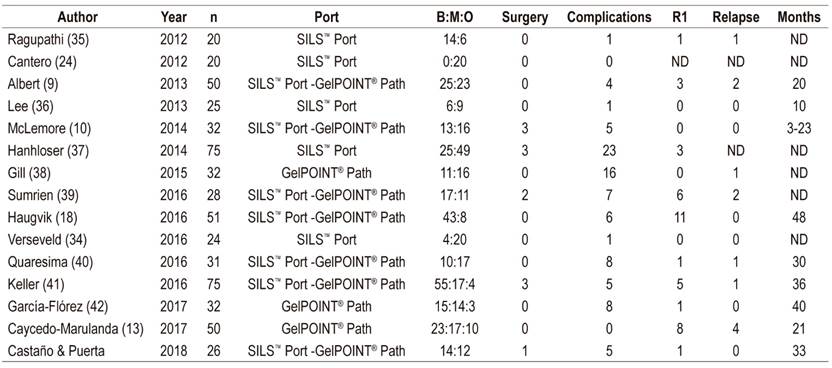
B:M:O: benign, malignant, others; R1: positive margin; ND: no data.
One limitation of this study is its retrospective nature, which can induce some selection biases and affect the veracity of conclusions. Another is the fact that it concentrates on procedures performed by two of the authors at a referral institution. Consequently, this experience cannot be generalized to all surgeons. Also, average follow-up time was less than three years. This is a short time although most relapses have occurred in the first two years and are related to tumor biology rather than the quality of resection. 43 It is not clear if the absence of relapses in our series is due to the short follow-up time. Functional results were not evaluated, however, the results are encouraging with respect to absence of compromised anorectal function related to the procedure. Frequently, this function improved with removal of the rectal lesion.
In conclusion, consistent with current evidence supporting TAMIS as a viable alternative to radical excision of the rectum and showing that it produces less morbidity with faster recovery times and possible cost savings, our figures suggest that TAMIS is safe, effective and reproducible. In addition, we anticipate increasing use of this technique for more complex colorectal surgeries in our center, and we emphasize the value of histological evaluation of the resected segments.
Acknowledgements
This study was carried out with the support of the sustainability project of the vice chancellor’s office of research of the university of antioquia
REFERENCES
1. Martin-Perez B, Andrade-Ribeiro GD, Hunter L, Atallah S. A systematic review of transanal minimally invasive surgery (TAMIS) from 2010 to 2013. Tech Coloproctol. 2014 Sep;18(9):775-88. https://doi.org/10.1007/s10151-014-1148-6 [ Links ]
2. deBeche-Adams T, Hassan I, Haggerty S, Stefanidis D. Transanal Minimally Invasive Surgery (TAMIS): a clinical spotlight review. Surg Endosc. 2017 Oct;31(10):3791-3800. https://doi.org/10.1007/s00464-017-5636-4 [ Links ]
3. Buess G. Review: transanal endoscopic microsurgery (TEM). J R Coll Surg Edinb. 1993 Aug;38(4):239-45. [ Links ]
4. de Graaf EJ, Burger JW, van Ijsseldijk AL, Tetteroo GW, Dawson I, Hop WC. Transanal endoscopic microsurgery is superior to transanal excision of rectal adenomas. Colorectal Dis. 2011 Jul;13(7):762-7. https://doi.org/10.1111/j.1463-1318.2010.02269.x [ Links ]
5. Moore JS, Cataldo PA, Osler T, Hyman NH. Transanal endoscopic microsurgery is more effective than traditional transanal excision for resection of rectal masses. Dis Colon Rectum. 2008 Jul;51(7):1026-30; discussion 1030-1. https://doi.org/10.1007/s10350-008-9337-x [ Links ]
6. Larach SW. Microcirugía transanal (TEM) y cirugía transanal mínimamente invasiva (TAMIS). Cirugía española. 2012;90(7):418-20. https://doi.org/10.1016/j.ciresp.2012.04.004 [ Links ]
7. Atallah S, Albert M, Larach S. Transanal minimally invasive surgery: a giant leap forward. Surg Endosc . 2010 Sep;24(9):2200-5. https://doi.org/10.1007/s00464-010-0927-z [ Links ]
8. Lim SB, Seo SI, Lee JL, Kwak JY, Jang TY, Kim CW, et al. Feasibility of transanal minimally invasive surgery for mid-rectal lesions. Surg Endosc . 2012 Nov;26(11):3127-32. https://doi.org/10.1007/s00464-012-2303-7 [ Links ]
9. Albert MR, Atallah SB, deBeche-Adams TC, Izfar S, Larach SW. Transanal minimally invasive surgery (TAMIS) for local excision of benign neoplasms and early-stage rectal cancer: efficacy and outcomes in the first 50 patients. Dis Colon Rectum . 2013 Mar;56(3):301-7. https://doi.org/10.1097/DCR.0b013e31827ca313 [ Links ]
10. McLemore EC, Weston LA, Coker AM, Jacobsen GR, Talamini MA, Horgan S, et al. Transanal minimally invasive surgery for benign and malignant rectal neoplasia. Am J Surg. 2014 Sep;208(3):372-81. https://doi.org/10.1016/j.amjsurg.2014.01.006 [ Links ]
11. Slack T, Wong S, Muhlmann M. Transanal minimally invasive surgery: an initial experience. ANZ J Surg. 2014 Mar;84(3):177-80. https://doi.org/10.1111/j.1445-2197.2012.06320.x [ Links ]
12. Maglio R, Muzi GM, Massimo MM, Masoni L. Transanal minimally invasive surgery (TAMIS): new treatment for early rectal cancer and large rectal polyps-experience of an Italian center. Am Surg. 2015 Mar;81(3):273-7 [ Links ]
13. Caycedo-Marulanda A, Jiang HY, Kohtakangas EL. Transanal minimally invasive surgery for benign large rectal polyps and early malignant rectal cancers: experience and outcomes from the first Canadian centre to adopt the technique. Can J Surg. 2017 Dec;60(6):416-423. https://doi.org/10.1503/cjs.002417 [ Links ]
14. Alves EF, Costa PFO, Guerra JC. Transanal minimally invasive surgery with single-port (TAMIS) for the management of rectal neoplasms: a pilot study. J Coloproctol. 2012;32(4):402-6. https://doi.org/10.1590/S2237-93632012000400007 [ Links ]
15. Sevá-Pereira G, Trombeta VL, Capochim Romagnolo LG. Transanal minimally invasive surgery (TAMIS) using a new disposable device: our initial experience. Tech Coloproctol . 2014 Apr;18(4):393-7. https://doi.org/10.1007/s10151-013-1036-5 [ Links ]
16. Kalloo AN, Singh VK, Jagannath SB, Niiyama H, Hill SL, Vaughn CA, et al. Flexible transgastric peritoneoscopy: a novel approach to diagnostic and therapeutic interventions in the peritoneal cavity. Gastrointest Endosc. 2004 Jul;60(1):114-7. https://doi.org/10.1016/S0016-5107(04)01309-4 [ Links ]
17. Canes D, Desai MM, Aron M, Haber GP, Goel RK, Stein RJ, et al. Transumbilical single-port surgery: evolution and current status. Eur Urol. 2008 Nov;54(5):1020-9. https://doi.org/10.1016/j.eururo.2008.07.009 [ Links ]
18. Haugvik SP, Groven S, Bondi J, Vågan T, Brynhildsvoll SO, Olsen OC. A critical appraisal of transanal minimally invasive surgery (TAMIS) in the treatment of rectal adenoma: a 4-year experience with 51 cases. Scand J Gastroenterol. 2016 Jul;51(7):855-9. https://doi.org/10.3109/00365521.2016.1157891 [ Links ]
19. Keller DS, Haas EM. Transanal Minimally Invasive Surgery: State of the Art. J Gastrointest Surg. 2016 Feb;20(2):463-9. https://doi.org/10.1007/s11605-015-3036-4 [ Links ]
20. Mentges B, Buess G, Effinger G, Manncke K, Becker HD. Indications and results of local treatment of rectal cancer. Br J Surg. 1997 Mar;84(3):348-51. https://doi.org/10.1046/j.1365-2168.1997.02556.x [ Links ]
21. Lezoche E, Baldarelli M, Lezoche G, Paganini AM, Gesuita R, Guerrieri M. Randomized clinical trial of endoluminal locoregional resection versus laparoscopic total mesorectal excision for T2 rectal cancer after neoadjuvant therapy. Br J Surg. 2012 Sep;99(9):1211-8. https://doi.org/10.1002/bjs.8821 [ Links ]
22. Kennedy ML, Lubowski DZ, King DW. Transanal endoscopic microsurgery excision: is anorectal function compromised? Dis Colon Rectum . 2002 May;45(5):601-4. https://doi.org/10.1007/s10350-004-6252-7 [ Links ]
23. Schiphorst AH, Langenhoff BS, Maring J, Pronk A, Zimmerman DD. Transanal minimally invasive surgery: initial experience and short-term functional results. Dis Colon Rectum . 2014 Aug;57(8):927-32. https://doi.org/10.1097/DCR.0000000000000170 [ Links ]
24. Cantero R, Salgado G. Transanal access for rectal tumors: the simultaneous use of a flexible endoscope and SILS. Tech Coloproctol . 2014 Mar;18(3):301-2. https://doi.org/10.1007/s10151-012-0916-4 [ Links ]
25. McLemore EC, Coker A, Jacobsen G, Talamini MA, Horgan S. eTAMIS: endoscopic visualization for transanal minimally invasive surgery. Surg Endosc . 2013 May;27(5):1842-5. https://doi.org/10.1007/s00464-012-2652-2 [ Links ]
26. Fang SH, Ngamruengphong S. Combined endoscopic submucosal dissection and transanal minimally invasive surgery for resection of large refractory rectal polyp. Endoscopy. 2018 May;50(5):548-549. https://doi.org/10.1055/s-0044-101020 [ Links ]
27. James DRC, Goodbrand S, Sivathondan P, Cunningham C, Hompes R. Hybrid transanal resection of a near-circumferential large, low rectal polyp - a video vignette. Colorectal Dis . 2018 May;20(5):454. https://doi.org/10.1111/codi.14050 [ Links ]
28. Clermonts SH, Zimmerman DD. Closure of the rectal defect after transanal minimally invasive surgery: a word of caution. Colorectal Dis . 2015 Jul;17(7):642-3. https://doi.org/10.1111/codi.12990 [ Links ]
29. Lee L, Althoff A, Edwards K, Albert MR, Atallah SB, Hunter IA, et al. Outcomes of Closed Versus Open Defects After Local Excision of Rectal Neoplasms: A Multi-institutional Matched Analysis. Dis Colon Rectum . 2018 Feb;61(2):172-178. https://doi.org/10.1097/DCR.0000000000000962 [ Links ]
30. Menahem B, Alves A, Morello R, Lubrano J. Should the rectal defect be closed following transanal local excision of rectal tumors? A systematic review and meta-analysis. Tech Coloproctol . 2017 Dec;21(12):929-936. https://doi.org/10.1007/s10151-017-1714-9 [ Links ]
31. Baatrup G, Borschitz T, Cunningham C, Qvist N. Perforation into the peritoneal cavity during transanal endoscopic microsurgery for rectal cancer is not associated with major complications or oncological compromise. Surg Endosc . 2009 Dec;23(12):2680-3. https://doi.org/10.1007/s00464-008-0281-6 [ Links ]
32. Gavagan JA, Whiteford MH, Swanstrom LL. Full-thickness intraperitoneal excision by transanal endoscopic microsurgery does not increase short-term complications. Am J Surg. 2004 May;187(5):630-4. https://doi.org/10.1016/j.amjsurg.2004.01.004 [ Links ]
33. Lee L, Kelly J, Nassif GJ, Keller D, Debeche-Adams TC, Mancuso PA, et al. Establishing the learning curve of transanal minimally invasive surgery for local excision of rectal neoplasms. Surg Endosc . 2018 Mar;32(3):1368-1376. https://doi.org/10.1007/s00464-017-5817-1 [ Links ]
34. Verseveld M, Barendse RM, Gosselink MP, Verhoef C, de Graaf EJ, Doornebosch PG. Transanal minimally invasive surgery: impact on quality of life and functional outcome. Surg Endosc . 2016 Mar;30(3):1184-7. https://doi.org/10.1007/s00464-015-4326-3 [ Links ]
35. Ragupathi M, Vande Maele D, Nieto J, Pickron TB, Haas EM. Transanal endoscopic video-assisted (TEVA) excision. Surg Endosc . 2012 Dec;26(12):3528-35. https://doi.org/10.1007/s00464-012-2399-9 [ Links ]
36. Lee TG, Lee SJ. Transanal single-port microsurgery for rectal tumors: minimal invasive surgery under spinal anesthesia. Surg Endosc . 2014 Jan;28(1):271-80. https://doi.org/10.1007/s00464-013-3184-0 [ Links ]
37. Hahnloser D, Cantero R, Salgado G, Dindo D, Rega D, Delrio P. Transanal minimal invasive surgery for rectal lesions: should the defect be closed? Colorectal Dis . 2015 May;17(5):397-402. https://doi.org/10.1111/codi.12866 [ Links ]
38. Gill S, Stetler JL, Patel A, Shaffer VO, Srinivasan J, Staley C, et al. Transanal Minimally Invasive Surgery (TAMIS): Standardizing a Reproducible Procedure. J Gastrointest Surg. 2015 Aug;19(8):1528-36. https://doi.org/10.1007/s11605-015-2858-4 [ Links ]
39. Sumrien H, Dadnam C, Hewitt J, McCarthy K. Feasibility of Transanal Minimally Invasive Surgery (TAMIS) for Rectal Tumours and Its Impact on Quality of Life - The Bristol Series. Anticancer Res. 2016 Apr;36(4):2005-9 [ Links ]
40. Quaresima S, Balla A, Franceschilli L, La Torre M, Iafrate C, Shalaby M, et al. Transanal Minimally Invasive Surgery for Rectal Lesions. JSLS. 2016 Jul-Sep;20(3):e2016.00032. https://doi.org/10.4293/JSLS.2016.00032 [ Links ]
41. Keller DS, Tahilramani RN, Flores-Gonzalez JR, Mahmood A, Haas EM. Transanal Minimally Invasive Surgery: Review of Indications and Outcomes from 75 Consecutive Patients. J Am Coll Surg. 2016 May;222(5):814-22. https://doi.org/10.1016/j.jamcollsurg.2016.02.003 [ Links ]
42. García-Flórez LJ, Otero-Díez JL, Encinas-Muñiz AI, Sánchez-Domínguez L. Indications and Outcomes From 32 Consecutive Patients for the Treatment of Rectal Lesions by Transanal Minimally Invasive Surgery. Surg Innov. 2017 Aug;24(4):336-342. https://doi.org/10.1177/1553350617700803 [ Links ]
43. Bach SP, Hill J, Monson JR, Simson JN, Lane L, Merrie A, et al. A predictive model for local recurrence after transanal endoscopic microsurgery for rectal cancer. Br J Surg. 2009 Mar;96(3):280-90. https://doi.org/10.1002/bjs.6456 [ Links ]
Received: July 24, 2018; Accepted: May 10, 2019











 texto en
texto en