Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Accesos
Accesos
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en
SciELO
Similares en
SciELO -
 Similares en Google
Similares en Google
Compartir
Revista colombiana de Gastroenterología
versión impresa ISSN 0120-9957
Rev Col Gastroenterol vol.34 no.3 Bogotá jul./set. 2019
https://doi.org/10.22516/25007440.217
Case report
A case report of eosinophilic esophagitis
1Especialista de 1.er grado en Anatomía Patológica e Instructor, Hospital Provincial Docente Manuel Ascunce Domenech, Camagüey, Cuba
2Especialista de 2.do grado en Medicina Interna y Profesor Titular, Hospital Provincial Docente Manuel Ascunce Domenech, Camagüey, Cuba
3Especialista de 2.do grado en Medicina Interna y Profesor Auxiliar, Hospital Provincial Docente Manuel Ascunce Domenech, Camagüey, Cuba
4Especialista de 1.er grado en Medicina Interna e Instructor, Hospital Provincial Docente Manuel Ascunce Domenech, Camagüey, Cuba
5Especialista de 1.er grado en Anatomía Patológica e Instructora, Hospital Provincial Docente Manuel Ascunce Domenech, Camagüey, Cuba
Objective:
We present the first case of eosinophilic esophagitis (EE) reported in our country in fifty-three years.
Clinical Case:
The patient was 28-year-old white woman with a personal history of atopy, allergic rhinitis, dermatitis and occasional diarrhea and asthma. She had relatives with bronchial asthma and had been admitted to hospitals several times previously. According to the patient, these alterations began at age 17, and she had seen several specialists since that time. Ten months prior to this admission, increasingly severe dysphagia accompanied by chest and abdominal pain, heartburn and weight loss began. Upon physical examination, wheezing was evident in both lung fields. The complete analytical study and imaging tests were all normal. Endoscopy and esophageal biopsy showed elements compatible with eosinophilic esophagitis. Excellent results were obtained from treatment with oral steroids, montelukast and proton pump inhibitors.
Conclusions:
EE is still poorly understood. It is more common in children and young white men, and there is usually a marked atopic component. In adulthood it is manifested by dysphagia and impaction of food. To diagnose EE there must be symptoms of esophageal dysfunction, more than 15 eosinophils per field, lack of response to proton pump inhibitors and exclusion of gastroesophageal reflux. Depending on the case, patients may require multidisciplinary treatment by gastroenterologists, allergists, immunologists and nutritionists.
Keywords: Eosinophilic esophagitis
Objetivo:
presentar un caso infrecuente de un paciente con esofagitis eosinofílica, el cual constituye el primer caso reportado en nuestro país en 53 años.
Caso clínico:
paciente de 28 años, género femenino, de raza blanca, con antecedentes personales de atopia, rinitis alérgica, dermatitis, diarreas ocasionales y asma, por la cual ha estado ingresada en varias ocasiones; además presenta antecedentes familiares de asma bronquial. Refiere que estas alteraciones comenzaron a los 17 años, y desde allí fue asistida por varios especialistas. Hace 10 meses presentó disfagia, la cual fue en aumento, dolor torácico y abdominal, pirosis y pérdida de peso. En el examen físico presentó sibilancias diseminadas en ambos campos pulmonares. El estudio analítico completo y los exámenes imagenológicos resultaron normales. La endoscopia y la biopsia esofágica mostraron los elementos compatibles con esofagitis eosinofílica. El tratamiento se realizó con esteroides orales, monteleukast e inhibidores de la bomba de protones, que mostraron resultados excelentes.
Conclusiones:
la esofagitis eosinofílica es una enfermedad de la que todavía existe un gran desconocimiento. Es más común en niños, hombres jóvenes de raza blanca, y la cual, por lo regular, tiene un componente atópico marcado. En la adultez se manifiesta por disfagia e impactación de los alimentos. Para el diagnóstico de una esofagitis eosinofílica tiene que haber síntomas de disfunción esofágica, más de 15 eosinófilos por campo, falta de respuesta a los inhibidores de la bomba de protones y exclusión del reflujo gastroesofágico. Dependiendo de cada caso, el paciente debe ser tratado de forma multidisciplinaria por gastroenterólogos, alergólogos, inmunólogos y nutriólogos.
Palabras clave: Esofagitis eosinofílica
Introduction
Eosinophilic esophagitis is the result of inflammation of the esophagus due to eosinophils, a type of leukocyte involved in immunity against certain infections , especially of parasites, and in many allergic diseases such as bronchial asthma. 1 Although it is a rare disease, the frequency of eosinophilic esophagitis is increasing in many developed countries for reasons that remain unclear although it is known that all types of allergies now occur more frequently than in past generations. 2 In addition, there have been studies of other pathologies that have eosinophilic infiltration such as infectious esophagitis, Crohn’s disease, hypereosinophilic syndrome, adverse drug reactions and connective tissue disease. 1 Various terms have been used to refer to this entity, but the most commonly accepted term is eosinophilic esophagitis. 3 The first case, an adult with a history of atopy who presented esophageal spasms, was reported in the literature by Dobbins et al. in 1977.
Eosinophilic esophagitis’ impact is global since cases have been described on every continent except Africa. 5 It is estimated that its prevalence currently varies between 0.4% and 1.0% in adult patients and between 0.04% and 0.09% in children with an annual incidence of 1:100,000 in adults and 1:10,000 in children. Affected adults are most often young men between 20 and 50 years of age (average age of 38 years). The male to female ratio of cases is 3:1, but reported symptoms are similar for both sexes. 5
The objective of this study is to present the first case of a patient with eosinophilic esophagitis in Colombia in 53 years.
Clinical case
The patient was a 28 year old white woman who worked as a teacher, did not smoker, and had a family history of allergy and asthma. She said that she had suffered from allergic rhinitis, recurrent atopic dermatitis, occasional diarrhea and bronchial asthma from the age 17 and had been hospitalized several times. She had been examined by the pulmonology, immunology and allergy services. A skin prick test had shown sensitivity for lacticin, bread, beans, rice and tomatoes. An allergen-specific immunoglobulin E (IgE) test found elevated levels for these foods, so allergists treated her with multiple antihistamines and a diet. She improved for several months, but at 10 months she began to experience progressively increasing dysphagia, heartburn, chest pain and epigastric abdominal pain for which reason she came to the hospital.
Physical Examination
The patient was depressed but not in poor general condition. She was hydrated, her skin and mucous membranes were normally colored, her hair and nails were normal, and she had no peripheral lymphadenopathy, edema or skin lesions. Her respiratory rate was 16 breaths per minute (rpm). She had a mild vesicular murmur with scattered wheezing in both lung fields, and her heartbeats were rhythmic and without murmurs. Her blood pressure was 110∕70 mm Hg.
Her abdomen was soft and depressible to touch and without pain. There were no signs of visceromegaly. The rest of the physical examination, including the gynecological exam, found no alterations. The fundi of her eyes were normal.
Tests
All biochemical and hematological studies were within normal limits and her chest, esophageal, stomach and duodenal x-rays and her electrocardiogram were normal. No abnormalities were found with abdominal and gynecological ultrasound or a CT scan.
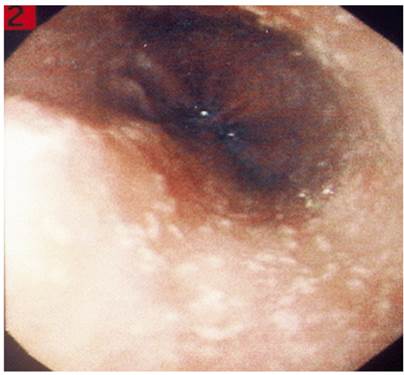
Esophagogastroduodenoscopy found focal stenosis, superficial punctate papules with evident inflammation, and circumferential rings (feline esophagus) with abundant punctate exudates. Her stomach and duodenum were normal.
Histological study showed inflammation with numerous intraepithelial eosinophils with extensive granulation plus microabcesses on the surface (Figures 1, 2, 3 y 4). The intraepithelial eosinophils were most numerous in the upper half of the epithelium. The histological study of the stomach and duodenum was normal.
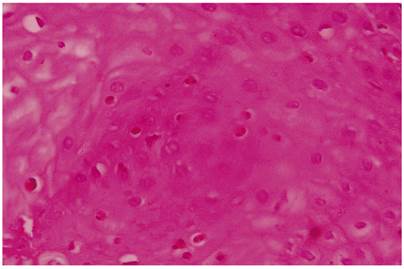
Figure 2 Photomicrograph showing the epithelium of the esophageal mucous with diffuse distribution eosinophils. H ∕ E 20 x.
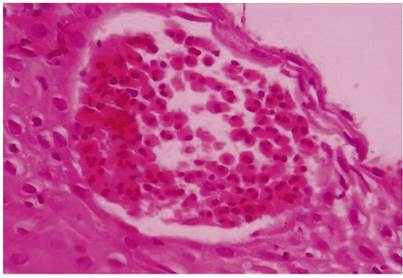
Figure 3 Histological field of whitish punctate papules. Note the formation of an eosinophilic abscess in the upper third of the epithelium. H ∕ E 40 x.
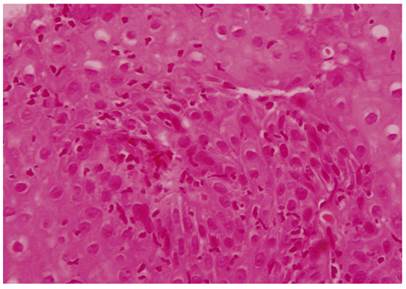
Figure 4 Histology shows distribution of eosinophilic cells is deeper and less regular toward the middle and lower third of the esophagus. H / E 40 x.
A soft diet of purees, broths, and soups, that eliminated all foods that had triggered her crises was initiated. Omeprazole, montelukast and prednisone were administered for eight weeks. Her response was favorable, and a follow-up esophagogastroduodenoscopy was normal.
Discussion
Under normal conditions, there are no eosinophils in the esophagus, so their presence is considered pathological. Until a few years ago, eosinophils in the esophageal mucosa was considered a marker of reflux. 1 In recent years, a large number of patients with symptoms of esophageal dysfunction and large eosinophilic infiltrations of the esophagus who do not respond to anti-reflux measures but have normal esophageal pH have been described. This combination corresponds to eosinophilic esophagitis. 3 Noel et al. conducted a study of 103 patients, 0 to 19 years of age, who had eosinophilic esophagitis. It reported a predominance of the male gender (71%). Half of them had histories of atopy, and 70% of them had family histories of atopy. Our patient had a personal and family history of atopy. Personal histories of atopy are found in 60% of cases while family histories are found in 20% to 40% of cases. 6 The pathophysiology of eosinophilic esophagitis includes atopy, eotaxin-3, and interleukins. Some foods and aeroallergens are indicated in atopy while eotaxin-3 implies a genetic component and interleukins are mediators of inflammation. Gastroesophageal reflux is a component that is under discussion. 3 It has been noted that the presence of eosinophils in the esophagus is pathological and prone to chronicity, but the cause of eosinophilic infiltration of the esophagus is currently ignored. 1 Manifestations vary greatly from patient to patient according to their ages. Some patients’ symptoms are constant while other patients’ symptoms appear intermittently or seasonally. 2 Dysphagia and food impaction occur more frequently in adults, followed by symptoms of gastroesophageal reflux, chest pain and abdominal pain. 1-3 A study by Desai et al. has found that eosinophilic esophagitis was responsible for 50% of esophageal food impacts in outpatient visits. 7 A significant delay in the diagnosis of the disease in the adult population is noted, with an average of 4.5 years from the onset of symptoms until the time of diagnosis. 1 In our case, the delay was even longer. In 50% to 80% of both adult and pediatric patients, one or more of the following atopic conditions occur: asthma, sinusitis, dermal lesions, food allergies and/or eczema. 1,3,5 They are often observed with seasonal changes as was the case with our patient, taking into account her genetic background. Complications include esophageal structural abnormalities, Boerhaave syndrome and nutritional deficiencies. 8
The diagnosis is confirmed with endoscopy and biopsy when there are more than 15 eosinophils observed per field similar to findings for our patient. 1,2 The most common endoscopic findings are esophageal grooves, esophageal rings, whitish granulations, esophageal strictures, whitish plaques associated with eosinophilic microabscesses, and areas of high density of eosinophil infiltrate. 2 Thirty percent of endoscopies may appear normal, but care should be taken due to the fragility of the mucosa. Five biopsies including one from the stomach and one from the duodenum are recommended in order to rule out other entities. 2 This was done in the case presented here.
Treatment of eosinophilic esophagitis is controversial, so no optimal therapy or even expected goals have been defined. 1,5,7. Liacouras et al. observed that the combination of steroids and diet significantly improved symptoms and histological findings, as in the case of our patient. 9 Teltelbaum et al. 10 and Konikoff et al. 11 recommend using steroids systemically or topically for four to six weeks. 10,11 We administered steroids orally for eight weeks, and we progressively decreased them over six months.
The diet eliminates all solid foods and replaces them with appropriate nutritional formulas that avoid foods identified as allergens. 1,2,3,6-10. Due to the relationship between eosinophilic esophagitis and gastroesophageal reflux, the use of proton pump inhibitors has been considered as primary or adjuvant treatment, and we administered them in this case. The current recommendation is that proton pump inhibitors should not be considered primary therapy. 3 Leukotrienes are chemoattractants of eosinophils, and they have been postulated as another therapeutic option for improving symptoms. Nevertheless, since they do not improve histology, these medications are not recommended for eosinophilic esophagitis. 12
More recently, therapies that act against specific substances identified within the inflammatory cascade have been proposed. These include mepolizumab, a humanized monoclonal antibody that blocks interleukin 5 (IL-5). 13 We used steroids together with a proton pump inhibitor and a leukotriene antagonist and obtained favorable results.
Conclusions
Eosinophilic esophagitis consists of inflammation of the esophagus that is characterized by a large numbers of eosinophils in histological studies. It is an allergic disorder whose frequency is increasing in the population because knowledge about it has improved. Its pathophysiology is not known with certainty, and there is no definitive treatment. The diagnosis is confirmed with endoscopy including five biopsy samples including one from the stomach and one from the duodenum. Differential diagnosis should consider more frequent diseases that feature eosinophilic infiltration of the esophagus.
Referencias
1. Furuta GT, Liacouras CA, Collins MH, Gupta SK, Justinich C, Putnam PE, et al. Eosinophilic esophagitis in children and adults: a systematic review and consensus recommendations for diagnosis and treatment. Gastroenterology. 2007 Oct;133(4):1342-63. https://doi.org/10.1053/j.gastro.2007.08.017. [ Links ]
2. González G, Torres J, Molina R, Harris P. Esofagitis eosinofílica en niños: características clínicas y endoscópicas. RevMed Chile 2009;137:666-671. https://doi.org/10.4067/S0034-98872009000500010. [ Links ]
3. Beltrán C, García R, Espino A, Silva C. Esofagitis eosinofilica: una enfermedad emergente. Rev Otorrinolaringol Cir Cabeza y cuello. 2009;69:287-298. https://doi.org/10.4067/S0718-48162009000300013. [ Links ]
4. Dobbins JW, Sheahan DG, Behar J. Eosinophilic gastroenteritis with esophageal involvement. Gastroenterology. 1977 Jun;72(6):1312-6. [ Links ]
5. Buckmeier BK, Rothenberg ME, Collins NH. The incidence and prevalence of eosinophilicesophagitis. J AllergyclinInmunol 2008; 121(2 Suppl 1):S71. https://doi.org/10.1016/j.jaci.2007.12.281. [ Links ]
6. Noel RJ, Putnam PE, Rothenberg ME. Eosinophilic esophagitis. N Engl J Med. 2004 Aug 26;351(9):940-1. https://doi.org/10.1056/NEJM200408263510924. [ Links ]
7. Desai TK, Stecevic V, Chang CH, Goldstein NS, Badizadegan K, Furuta GT. Association of eosinophilic inflammation with esophageal food impaction in adults. Gastrointest Endosc. 2005 Jun;61(7):795-801. https://doi.org/10.1016/s0016-5107(05)00313-5. [ Links ]
8. Gupte AR, Draganov PV. Eosinophilic esophagitis. World J Gastroenterol. 2009 Jan 7;15(1):17-24. https://doi.org/10.3748/wjg.15.17. [ Links ]
9. Liacouras CA, Wenner WJ, Brown K, Ruchelli E. Primary eosinophilic esophagitis in children: successful treatment with oral corticosteroids. J Pediatr Gastroenterol Nutr. 1998 Apr;26(4):380-5. https://doi.org/10.1097/00005176-199804000-00004. [ Links ]
10. Teitelbaum JE, Fox VL, Twarog FJ, Nurko S, Antonioli D, Gleich G, et al. Eosinophilic esophagitis in children: immunopathological analysis and response to fluticasone propionate. Gastroenterology. 2002 May;122(5):1216-25. https://doi.org/10.1053/gast.2002.32998. [ Links ]
11. Konikoff MR, Noel RJ, Blanchard C, Kirby C, Jameson SC, Buckmeier BK, et al. A randomized, double-blind, placebo-controlled trial of fluticasone propionate for pediatric eosinophilic esophagitis. Gastroenterology. 2006 Nov;131(5):1381-91. https://doi.org/10.1053/j.gastro.2006.08.033. [ Links ]
12. Ferré-Ybarz L, Nevot Falcó S, Plaza-Martín AM. Eosinophilic oesophagitis: clinical manifestations and treatment options. The role of the allergologist. Allergol Immunopathol (Madr). 2008 Nov-Dec;36(6):358-65. https://doi.org/10.1016/S0301-0546(08)75869-5. [ Links ]
13. Stein ML, Collins MH, Villanueva JM, Kushner JP, Putnam PE, Buckmeier BK, Filipovich AH, Assa’ad AH, Rothenberg ME. Anti-IL-5 (mepolizumab) therapy for eosinophilic esophagitis. J Allergy Clin Immunol. 2006 Dec;118(6):1312-9. https://doi.org/10.1016/j.jaci.2006.09.007. [ Links ]
Received: February 22, 2018; Accepted: April 23, 2018











 texto en
texto en