Introduction
The anterior approach for cervical spine surgery has been in practice since the 1950s, serving various purposes such as spine stabilization in cases of spinal tumors, trauma, and osteomyelitis. The proximity of the cervical spine to the esophagus, coupled with the requirement to mobilize the esophagus, increases the risk of esophageal injury during these surgical interventions. Nevertheless, such complications are exceedingly rare, with prevalence rates reported between 0.02% and 0.25%1,2.
Case presentation
We report the case of a 60-year-old male with no significant comorbid conditions. The patient had a history of cervical trauma from a road traffic accident 12 years prior, which necessitated a C4-C5-C6 corpectomy and anterior cervical fixation using prosthetic material. Subsequently, the patient developed cervical myelopathy and symptomatic spinal stenosis. He sought medical advice for persistent dysphagia, weight loss, and dysphonia over six months. Neurosurgical evaluation led to the performance of a cervical spine radiograph, which revealed anterior displacement of the C7 fixation screw (Figure 1).

Source: Author’s File.
Figure 1 Lateral cervical spine radiography. Arthrodesis plate with proximal fixation at C3 and distal fixation at C7 (arrow), along with an intermediate and a displaced distal screw.
An esophagogastroduodenoscopy was conducted, revealing a piece of osteosynthesis material (screw) lodged in the upper third of the esophagus at the cricopharyngeal level. This foreign object was successfully removed using a foreign body forceps (Figures 2 and 3). The patient’s clinical progression was favorable, marked by the resolution of dysphagia, and no additional procedures or interventions were required.
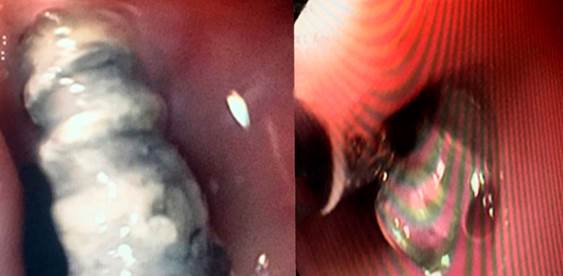
Source: Author’s File.
Figure 2 Endoscopic findings illustrating a foreign body (screw) in the proximal third of the esophagus at the level of the cricopharyngeus.
Discussion
Acute esophageal perforations associated with the anterior surgical approach to the cervical spine predominantly occur in two anatomically distinct zones of heightened risk, where excessive manipulation or retraction often plays a contributory role3,4. The initial risk zone is identified as Killian’s triangle, which is delineated by the juncture of the lower boundary of the pharyngeal constrictor muscle and the cricopharyngeal muscle; typically located at the level of C5-C6 or slightly more caudally. This area is notably vulnerable because the posterior mucosa of the esophagus lacks muscular protection, leaving only the slender buccopharyngeal fascia to separate the esophagus from the retrosternal space5. The second heightened risk area is situated laterally at the level of the thyrohyoid membrane1.
Despite the rarity of esophageal perforation following cervical spine surgical procedures, with a notably low incidence, it represents a complication with significant morbidity and mortality implications, even when identified intraoperatively; mortality rates reported stand at 20%, escalating further with delayed diagnosis and treatment2. Late esophageal perforations generally result from chronic friction leading to subsequent ischemia and necrosis2; the migration of screws tends to follow a benign trajectory, potentially even remaining asymptomatic due to their small diameter. This gradual process allows for the spontaneous repair of the induced defect6. It is not uncommon for screws to be uneventfully expelled through the gastrointestinal tract7. The majority of late migration cases are reported within the first 18 months following surgery8,9; yet, there have been instances noted several years post-operation6. Clinical manifestations range from asymptomatic presentations in delayed perforations to symptoms of dysphagia, subcutaneous emphysema, and sepsis in acute cases10.
The therapeutic arsenal for managing transmural esophageal defects via endoscopy includes the use of clips, esophageal stents, and negative pressure systems11. Esophageal stents, in particular, are favored for their established efficacy and safety, boasting success rates exceeding 80%12; their application in cervical perforations, however, is limited due to discomfort caused by the proximal end of the device protruding into the pharynx, often resulting in intolerance by the patient.
Negative pressure therapy emerges as a relatively novel approach that encourages granulation tissue formation, facilitating the obliteration of the cavity and the defect’s closure13,14. This method can be implemented as either a standalone treatment or in conjunction with radiological or surgical interventions15. Retrospective studies have highlighted its high success rate (89.4%)11 and the minimal complications associated with its application16. Similar to esophageal stents, the effectiveness of negative pressure therapy in proximal perforations may be limited by challenges in creating an airtight seal and maintaining a contained negative pressure environment. Consequently, the chosen treatment strategy should be tailored to the perforation’s clinical presentation and anatomical location, ranging from conservative or endoscopic management to surgical intervention for debridement and primary defect closure1,17.











 texto em
texto em