INTRODUCTION
Cervical cancer is one of the main causes of death among women who die of cancer in Latin America and the Caribbean 1. It is the fourth most common type of cancer affecting women worldwide; close to 85% of cases occur in developing countries; in 2012, 35,700 women died from cervical cancer in the Americas, 80% of them in Latin America and the Caribbean 2. In Colombia, in the period between 2007 and 2011, it was estimated that there were 4,462 new cases of cervical cancer per year, for a rate of 19.3 for every 100,000 women-year. During that same period, there were 115 new cases per year in Risaralda, for a rate of 21.9 x 100,000 3. At a national level, according to the Ministry of Health and Social Protection, the percentage of patients with cervical carcinoma in situ among the total number of detected cases of cervical cancer was 63.31% in 2012, the largest proportion coming from the contributive health regime as opposed to the subsidised regime 4.
This type of cancer represents a complex sexual and reproductive health problem, with a high social and economic impact, affecting increasingly younger women 5. It is a disease of multifactorial origin in which the human papilloma virus (HPV) is a necessary cause but not sufficient in itself for development of the disease 6. Other associated factors include lifestyle of women or their partners, long-term use of oral contraceptives, immunosuppression, cigarette smoking, first pregnancy before 17 years of age, poor eating habits and a history of sexually transmitted infections such as chlamydia 5.
Despite the fact that this form of cancer may be prevented by means of early detection of preneoplastic lesions and HPV vaccination, the risk of developing the disease and dying from it continues to be high: the lack of articulation among levels and stakeholders in the system and policy setbacks, together with unfavourable social and economic conditions of some women, contribute to the progression of the preneoplastic lesions caused by the virus towards high risk neoplasm or carcinoma in situ7.
Although the Colombian Ministry of Health and Social protection emphasises the importance of early detection of precancerous lesions by means of regular cytology testing and prevention methods such as vaccination at an early age and HPV typing 7, there are still barriers among healthcare staff who overestimate the value of cervical cytology, and in the community, because of the association of HPV with sexually transmitted diseases, as stated by Wiesner et al. 8.
A close relationship has been found to exist between cervical cancer and gender inequalities and inequities as a health problem 9-10. As pointed out by Cortés, there are countless cultural and gender barriers that prevent women from having access to cytology testing as a means of prevention. Moreover, the personal stigma of having HPV infection has an adverse effect on self-esteem and on the woman's significant relationships, but not so on the man 11. Cervical cancer, like most chronic diseases, is a complex problem with many sides to it, the most explored of which has been the biological; hence the importance of delving deeper into the way in which the disease is experienced and coped with 8. Some studies conducted in Latin America have approached the problem 12-14, but few have explored the experiences of women faced with this disease. Therefore, there is a need to consider cultural differences and specific needs of women in order to achieve greater equity when it comes to access to prevention programs and early and timely detection of cervical cancer 12. People's experiences reflect their own way of understanding and living a disease 15; consequently, there is a need to give a voice to women who live with cervical cancer. Qualitative research offers the possibility of exploring the subjective perception of the disease and the life experience 16. Framed within this paradigm, this study is aimed at exploring the life experiences of women diagnosed with cervical carcinoma in situ seen at a Level II hospital in a municipality of the Department of Risaralda, Colombia.
MATERIALS AND METHODS
The study, based on a qualitative phenomenological design 17, was conducted with the participation of women with cervical carcinoma in situ diagnosed more than one year before, seen in a regional public hospital, a social state company (ESE in Spanish) that provides low and intermediate complexity services to patients in the subsidised and contributive regimes of the Colombian social security system, located in a municipality in western Risaralda, Colombia. The study was conducted between August and October 2015, using in-depth interviews 18. Sample size was defined by saturation. A consecutive convenience sampling was performed.
Procedure. After explaining the objectives of the study and the interest of the researchers regarding the topic, the participants were asked to sign an informed consent in order to document their acceptance to participate. Later, the principal physician investigator interviewed the participants in the office of the early cervical cancer detection program in the hospital, to the point of content saturation. Following cultural validation, the interviews were recorded and transcribed, and there was no need to repeat or expand any of them. Social and demographic variables measured included age, a history of sexually transmitted diseases (STDs), use of methods for protection against STDs, use of other contraceptive methods, performance of prior cytology tests, and why the cancer had been detected.
Analysis. Coding and analysis were performed using the Atlas ti 7® qualitative software, by agreement between two researchers. Open coding was used initially (preliminary codes) for the analysis, followed by an axial coding (conceptual codes) based on the study's theoretical framework. This process led to the construction of relation networks and "families" derived from matching between related codes 19.
Ethical considerations. The protocol was approved by the institutional ethics committee, and was considered low risk 20: the topics discussed were recognised as sensitive. Participants were given the assurance of confidentiality. Pseudonyms were used in order to protect the identity of the interviewees.
RESULTS
Overall, 10 women were interviewed applying the selection criteria, up to the point of data saturation. None of the patients refused to be interviewed. The interviews were conducted in private and lasted an average of 90 minutes.
Social and demographic characteristics of the participants. Ages ranged between 19 and 36 years, with a median of 23. At the time of diagnosis, 7 out of 10 participants were in a relationship, and they had a median of 2 children. One of them did not have children.
Case characterisations. Based on the answers to the questions on specific considerations regarding sexual and reproductive health, it was determined that cervical carcinoma in situ was detected mainly by means of cervical cytology, which was mostly performed at the request of the women themselves; only four of the participants reported some form of discomfort such as pain or genital lesions as the reason for consulting a physician. Another conclusion from the analysis was that dual protection with the use of condoms before the diagnosis was either absent or intermittent, as shown in Table 1.
Table 1 Characterisation of in situ cervical cancer in relation with sexual health and prevention practices in Risaralda, Colombia, 2016
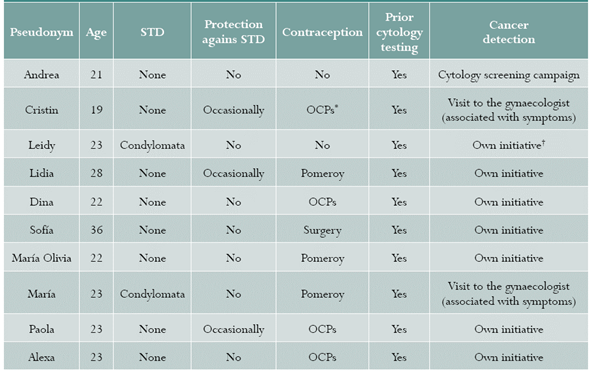
Source: authors.
* Oral contraceptives.
† Own initiative: patients decided to ask for cytologic testing for different reasons.
What was the experience like at the time of diagnosis: "the news"
In their narratives regarding their experiences at the time they were informed of their diagnosis, the women interviewed reported that the first moment brought with it a high emotional burden, in particular because they believed that the disease was fatal. Not one of the participants was expecting a diagnosis of cancer. Based on what they said, the news of the diagnosis left them devastated, uncertain, fearful and depressed. In some instances, there were negative feelings against their partners. Cristin, who was 19 when she was diagnosed, says the following: "I became very depressed, but, nonetheless, tried to find a solution; I asked what human papilloma was about [...] They removed what was dead in me. My menses smelled like death. You think you are going to die. I felt an emptiness in my vagina, as if there was something missing. I became aware of the fact that a piece of me was missing".
Knowledge regarding cervical cancer
The absence of pain or bleeding was a reason for the participants not to consider the possibility of having cancer. In her narrative, Andrea said: "They would tell me but I would reply, 'Nothing hurts and if I had cancer I should have been in pain or have been bleeding'; I did not feel any thing, but I had cancer." The partial knowledge that the participants had regarding cervical cancer, as well as the collective imagery that surfaced in some of the cases, make us consider the need to rethink the way in which knowledge can be brought to the patients in this area of health. Alexa, 23 at the time of diagnosis, suggests in her statement that there needs to be more clarity in order to gain greater understanding: "I only know what I am told, that they are diseases, that they happen, that they are sexually transmitted, that there are ways to prevent them."
Relationship with the partner
Some studies have suggested that traditional gender roles give rise to a passive attitude of women in their relationships as is evidenced by their acquiescence to the sexual demands of their partners, with no room for negotiation regarding the use of protection, for example condoms, against STDs 18. In the case of the women who participated in the study, it was frequently observed that, from their perspective, sexual protection is up to their partners only, tacitly accepting extramarital relations by their partners. This can be gleaned from the story told by María Oliva, diagnosed at 22 years of age: "I always tell him, 'make sure you take care because, in the end, it is me who suffers the consequences'." Like in María Oliva's case, several participants associate cervical cancer with the irresponsible sexual behaviour of their partners and they feel betrayed. Lina, 23, said the following: "I got this cancer from my partner, he gave it to me [...] I did not want to have intercourse with him, I was afraid because I thought it would make it worse, I was very cold to him [...] I gave him my best years because I went to live with him when I was fifteen.
I wondered, what am I doing here? I have lost my youth with him."
Support and support networks
The stigma created by the association between promiscuous relations and cervical cancer prevents women from resorting to the different social networks for support. Some of them end up coping with the diagnosis on their own out of fear or shame, lest their reality becomes known. This is how Alexa described her circumstances: "I felt ashamed that others would find out because, since you get that when you are not careful, I avoid discussing it; it is something for the home, I felt empty; I only told my mother."
DISCUSSION
This qualitative study shows the experiences reported by women with cervical carcinoma in situ at the time of learning about their diagnosis. They report not having expected such a result; they have no clear understanding about their disease and, consequently, they feel affected and believe that their lives are chan- ged in many ways. On the other hand, they believe that their partners are to blame and asymmetrical couple relationships come to the surface, pointing to the fact that women do not take active responsibility for their sexual protection. Finally, women have few support networks because of the stigma of what it means to live with cervical cancer.
The median age of 23 years at the time of di- agnosis in the participants suggests, as Gómez and Lagoueyte point out, that cervical cancer affects increasingly younger women in child-bearing age 21. For the women interviewed in the study, cervical cancer has given rise to life changes that are difficult to cope with, in particular in terms of their bodies, and their sex, love and social lives. As mentioned by Barroilhet and Forjaz 22, the personal meaning of cervical cancer is usually of harm or loss, although it may also become a challenge when there is a possibility of controlling or changing the situation created by the disease. According to Díaz 23,
gynaecological cancer is not merely a disorganised proliferation affecting some parts of the female body. Apart from physiological changes, the woman has to face the associated organic and psychological consequences of the disease and its treatments, and all this brings about a significant change in the relationship with her own body, her partner and the experience of her sexuality.
On the other hand, understanding the disease is important because how people perceive the idea of cervical cancer has to do with the way they experience their relationships with their partners and the way they live their sexual practices; it also has to do with the forms of prevention and care of the disease that are actually validated by the human group to which they belong. Social factors and power relations and, therefore, gender relations, are relevant and are part of the considerations that come into play in the health/disease concept 9.
Faced with a diagnosis of cervical cancer, the participants had to cope with a reality that puts them in an extremely complex situation: besides believing that their partners are probably to blame for their health problem, they have to live with a disease that carries with it a huge social burden because of the stigma of association with promiscuity. This results in a paucity of support networks because of shame and fear of rejection. Social and cultural studies on cervical cancer and HPV show how women with this diagnosis feel stigmatised in their sexuality and isolate themselves from social contact 24. The stigma that weighs on diseases such as cervical cancer reinforces the fatalistic perception about the condition, as well as gender subordination 25.
Taboos still exist that have a negative impact on timely detection of cervical cancer 26; the absence of pain or bleeding prevented the interviewees from suspecting the disease. Therefore, it is important to recognise that this type of cancer is more than mere symptoms and hence the need to educate and insist on periodic cytology testing as a means for early detection of the disease.
The lack of a discourse regarding rights and the difficulty for the participants to take charge of their bodies and health are made evident. Given that they blame their partners for giving them the HPV, they show no active role in facing this reality. Consequently, a gender approach is found to be important.
The results of the study must be read in the light of the phenomenological method and its strength lies in the ability to delve deeply into the experiences of a group of women with cervical cancer, offering an important framework for building strategies towards the adequate approach to the problem affecting this group of people. The weakness of the study, associated with the method used, has to do with the fact that the data obtained can only be generalised to the specific group studied.
CONCLUSIONS
In order to tackle the incidence of cervical cancer from a holistic perspective, it is important to implement comprehensive sexual education, taking into consideration the cultural and social dynamics of sexual practices, and involving males in prevention against the virus by creating awareness 9. It is imperative to work towards empowering women so that they can exercise autonomy regarding their sexual and reproductive life, and take personal responsibility, including self-care, in relation to HPV.
From the perspective of sexual health, there is a need to work on developing communication and information strategies consistent with the needs of individuals and groups in order to foster a better understanding of cervical cancer, its prevention and detection. This includes the need to overcome myths and taboos such as the association of the disease with pain and bleeding. Finally, it is important to conduct further in-depth research studies regarding women's perception of HPV infection and its prevention in order to have additional social and cultural perspectives to enable interventions aimed at changing paradigms that perpetuate the expansion of the disease.











 texto em
texto em 


