Introduction
Urticaria is a disease which primarily affects the skin, causing welts and/or angioedema 1. Patients commonly refer to these lesions as "hives," "reddening," "nettle rash," and "swelling." Based on how long it lasts, it is divided into acute and chronic urticaria (less than or more than six weeks, respectively), although the lesions are clinically similar. Acute urticaria affects one out of three people at some point in their lives; it has multiple causes and tends to be self-limiting. Chronic urticaria affects approximately one out of 100 people 1,2. Despite being less frequent than acute urticaria, it has a greater impact on the patients' quality of life and that of their families. Between 40 and 70% of patients with chronic urticaria believe their disease is secondary to a food or medication and decide to implement restrictions, which in more than 95% of cases are unnecessary. These restrictions are often supported by their attending physicians, with no clear proof of causality, worsening their quality of life 3,4. For example, they may avoid the consumption of several foods or medications even when the events persist after discontinuing the suspected substance.
Various guidelines are currently available with evidence-based recommendations for diagnosing and treating patients with urticaria 1,5-8. These guidelines have proven useful and help achieve optimal clinical control of the disease, improving the patients' quality of life and avoiding unnecessary restrictions 9. However, they are written from an allergy and dermatology specialist's perspective, and some recommendations are not accessible to primary care physicians who, in most cases, are the first to treat patients with urticaria. For urticaria, primary care physicians include general practice, family medicine, internal medicine, emergency medicine and pediatrics. In 20% of cases, the first medical consult is in the emergency room, due to respiratory symptoms or to how dramatic the skin lesions can be, affecting the face or a large body surface within a few seconds 10. It is common for many primary care physicians to refer to dermatologists and/or allergists even before determining the diagnosis or type of urticaria or having evaluated the clinical response to first line treatment.
When patients initially consult for urticaria, they should be reassured and offered highly effective and easily accessible treatments. The goals of this first visit are to:
Make the correct diagnosis.
Estimate the severity of the condition.
Begin first line treatment and avoid unnecessary restrictions.
Order the pertinent follow-up tests.
Determine if specialized treatment is needed.
All of these objectives can be handled by primary care physicians, allowing the patients timely treatment and the lowest impact of the disease on their daily lives. In addition, an appropriate approach to urticaria by primary care physicians helps reduce emergency room visits and direct patients needing specialized care to urticaria specialists, which benefits the healthcare system. In this consensus, based on international recommendations 1,5-7, several medical associations (Asociación Colombiana de Alergia, Asma e Inmunología [Colombian Association of Allergies, Asthma and Immunology] (ACAAI); Asociación Colombiana de Dermatología [Colombian Association of Dermatology] (ASOCOLDERMA); Sociedad Colombiana de Médicos Generales [Colombian Society of General Practitioners] (SOCOMEG), Asociación Colombiana de Medicina Interna [Colombian Association of Internal Medicine] (ACMI), Sociedad Colombiana de Medicina Familiar [Colombian Society of Family Medicine] (SOCMEF), Sociedad Colombiana de Pediatría [Colombian Society of Pediatrics] (SCP), and Asociación Colombiana de Emergencias Médicas [Colombian Association of Medical Emergencies] (ACEM)) have sought to draft a practical and simple document to help primary care physicians accomplish the objectives described.
Methodology
The panel of experts was composed of urticaria specialists (allergists and dermatologists) and primary care physicians (general practice, family medicine, emergency medicine, internal medicine and pediatrics). The following outcomes were considered important for the patients: control of symptoms like pruritis, welts, and angioedema; familial/social impact; quality of life; job and school performance and/or absenteeism; and serious side effects due to treatment. We defined the following parameters for the consensus:
• Objective: to construct a consensus to provide clear, practical and simple guidelines for the diagnosis and management of urticaria to primary care physicians, in line with the international guidelines on the disease.
• Consensus users: the main target is all people who participate in treating urticaria, especially primary care physicians: general practitioners, family physicians, emergency physicians, internists and pediatricians. The consensus recommendations can be useful for decision-making in academic or administrative institutions such as scientific associations, universities, the ministry of health, insurance agencies, hospitals and/or healthcare centers.
Target population: patients with urticaria.
Point of use: outpatient care, inpatient care, emergency room.
Aspects covered: the diagnosis and clinical management of urticaria.
Aspects not covered: specialist management, management of the differential diagnosis.
Underlying source of information: this document is based on several international guidelines on urticaria, especially the European guideline, as its recommendations include an evaluation of the evidence 1,5-7,11.
Panel composition: the panel was made up of allergists, dermatologists, pediatricians, general practitioners, family physicians, internists, emergency physicians, immunologists and epidemiologists who participated in developing the document.
The consensus included six steps and the Delphi methodology was used for panel decisions 12:
1. Drafting of the initial manuscript
Members of the Urticaria Centers of Reference and Excellence (UCARE) network belonging to ACAAI and ASOCOLDERMA drafted a manuscript which considered the underlying concepts of diagnosis and management in the international guidelines on urticaria.
2. Creation of the panel of experts
All scientific societies involved in the primary care of patients with urticaria were invited. Each scientific society selected two representatives.
3. Initial discussion of the manuscript
The initial document was shared with the rest of the panel, and, through meetings, agreements were reached on the topics that should be included or withdrawn from the document. Each topic is presented as a clinical question, and the answer to each question will be based on the international guidelines or, if necessary, on a review of the literature by the team of epidemiologists. The discussion identified potential barriers for primary care physicians to implement the guideline recommendations and possible solutions to these barriers. A maximum of three rounds of voting were conducted, seeking 90% agreement. If a consensus was not reached, the controversial points were discussed and the majority recommendation was recorded, reporting the percentage of approval.
4. Assignment of the strength of the recommendation and feasibility
The strength of the evidence was based on the GRADE system proposed in the international guidelines used as a reference. For this consensus, we only included recommendations with a strong recommendation. The feasibility of the recommendation being adopted by primary care physicians was defined by the panel's opinion (1, 5-7).
5. National external validation
To evaluate the clarity of the concepts and their applicability, the manuscript was presented to physicians from the various participating societies who were not on the panel. The recommendations they gave were once again discussed by the members of the panel and included in the manuscript.
6. International external validation
In a second phase not covered in this manuscript, considering the healthcare system differences between countries, the manuscript will be presented to various Latin American allergists and dermatologists to evaluate the transportability of the document to other countries.
Table 1 Characteristics of urticaria and angioedema.
RESULTS
HOW IS URTICARIA DIAGNOSED?
Currently, the diagnosis of urticaria is eminently clinical (Table 1). Urticaria is a condition characterized by the formation of welts and/or angioedema, accompanied by pruritis (Table 1). Acute and chronic urticaria are differentiated by their duration of less than or more than six weeks, respectively (Figure 1). Therefore, the first thing we must ask a patient with urticaria is:
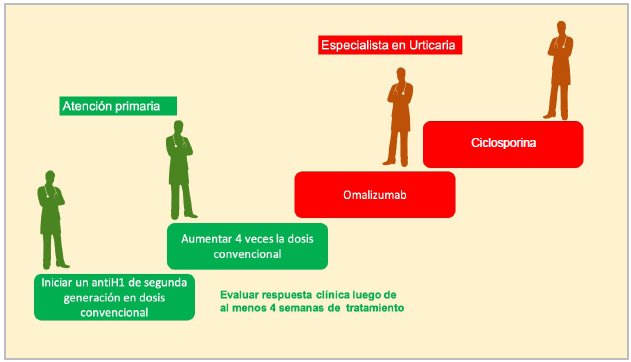
Figure 1 Urticaria classification flowchart. (Classification and suggested management. The management of the trigger depends on the patient; complementary studies are not always required to identify the cause, and it often is not found. Other times, it can be due to infections or food and drug allergies).
"What do the lesions look like?
When did they appear?
How long have you had the lesions?
How often do they appear?
How long does each lesion last?"
Based on these questions, we can determine if the patient has urticaria, and if it is chronic or acute (Table 2). We recommend that, if possible, the lesions should be confirmed with photographs (if they are not present when the patient consults), as the patient and physician may, at times, have different ideas of what constitutes a welt or angioedema. Acute and chronic urticaria tend to have different causes and prognoses (Figure 2): the acute form tends to occur together with or preceded by an infectious process, tends to be self-limiting and does not usually require additional diagnostic tests 13. The few exceptions occur when there is a suspected food or drug allergy presenting with a rash with welts or angioedema, which may be suspected when the reaction occurs soon after exposure to the suspect substance (usually within the first two hours) and does not occur spontaneously. On the other hand, the causes of chronic urticaria seem to be mainly self-reactivity mechanisms, and it is divided into two types: chronic spontaneous urticaria (CSU), in which welts occur independently of an environmental stimulus, and chronic inducible urticaria (CIU), in which certain physical stimuli can repeatedly trigger the skin manifestation, especially cold, water, heat, pressure, friction, vibration, exercise, etc. In 5-30% of patients both types of chronic urticaria may occur together. Therefore, it is important to ask the patient:
"What do you suspect causes the problem? Do the symptoms occur ONLY when you are exposed to this stimulus, or can they occur spontaneously?"
Since welts and angioedema are not pathognomonic of urticaria, the disease must be differentiated from other processes like anaphylaxis, hereditary angioedema, and urticarial vasculitis, among others. In this case, we can ask some questions aimed at ruling out differential diagnoses. In Tables 1 and 2 and Figure 1 we present the most common clinical characteristics of urticaria, and the main points to ask about and describe in the medical chart.
IDENTIFIED BARRIERS
Often, patients with urticaria are referred to specialists even before confirming if they have acute or chronic urticaria, which makes it difficult to access appropriate treatment promptly. Similarly, referrals to the emergency room and the lack of follow up in primary care lead to impaired disease control.
SOLUTION
Improved recognition of the disease helps differentiate it correctly from other processes which, while possibly also accompanied by welts and angioedema, have a different course and treatment. With the flowchart provided and the key questions, the correct diagnosis of urticaria can be improved.
Table 2 Clinical assessment of urticaria.
| # | Initial medical history | Comment |
|---|---|---|
| 1 | Time of onset of the disease | Time in months or years. |
| 2 | Description of the lesions | Number of welts, shape, size, distribution, duration and frequency of the events. |
| 3 | Associated angioedema (yes or no) | Location, frequency, possible association with respiratory symptoms |
| 4 | Associated symptoms | Joint pain, fever, abdominal pain, among others. |
| 5 | Family history of welts and angioedema. | The presence of urticaria in several members of the family should lead to a suspicion of other conditions. |
| 6 | Describe possible triggers | Foods, medications, infections, stress, physical activity, physical stimuli (pressure, water, etc.). Special attention to NSAIDs or ACE inhibitors. |
| 7 | Comorbidities | Special attention to autoimmune diseases. |
| 8 | Social, work and leisure activity history | To explore their relationship with the disease. |
| 9 | Prior treatment and clinical response | What medication has been taken, for how long, and disease control. |
| 10 | Prior procedures/ diagnostic results | Note all tests performed for the disease |
| A positive answer to questions 4, 5 or 6 means that other diagnoses must be considered along with a possible referral to an allergist or dermatologist. NSAIDs: nonsteroidal anti-inflammatory drugs ACE inhibitors: angiotensin-converting enzyme inhibitors. | ||
HOW DO I CLASSIFY URTICARIA ACCORDING TO ITS SEVERITY?
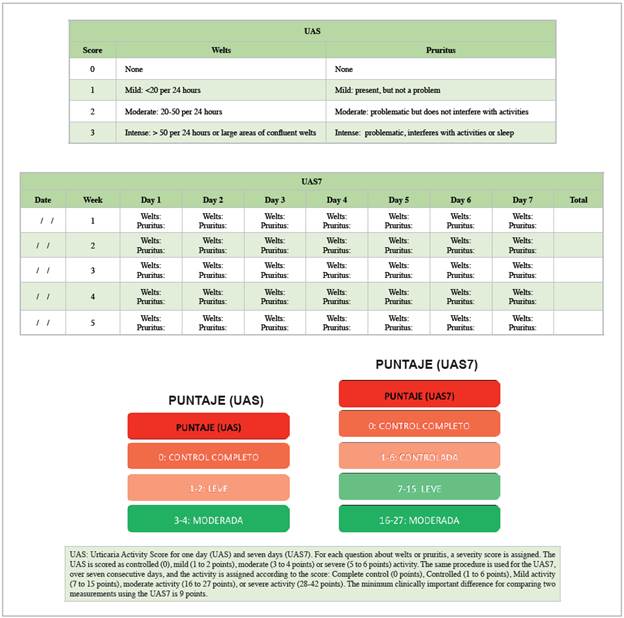
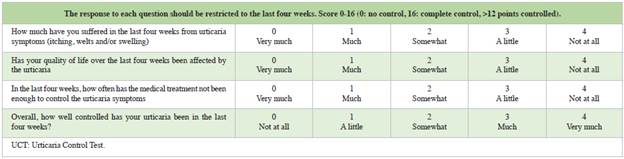
The activity of chronic urticaria is an important aspect that helps determine the level of control of the disease and the need for treatment changes. Two simple scales which are easily applied during an office visit and help give an idea of the severity and response to treatment are the Urticaria Activity Score (UAS) and the Urticaria Control Test (UCT). The UAS is based on the evaluation of the welts and pruritis, which are the key signs and symptoms of urticaria and can be easily documented by the patient 14,15.
The score evaluates the number of welts (0-3 points) and intensity of the pruritis (0-3 points) in 24 hours and assigns a score from 0-6. This scale can be applied on the day of the appointment, but ideally the patient should use it for at least seven consecutive days prior to the office visit, as this allows changes over time to be evaluated; in one week of evaluation, the maximum score is 42 points (Table 3). Qualitatively, the results are divided according to disease activity into "complete control" (score of 0), "control" (1-6 points), "mild" (7-15 points), "moderate" (16-27 points), and "severe" (28-42 points). The minimum clinically important difference on the UAS7 is nine points. Various web pages (e.g., https://www.profesionalessanitarios.novartis.es/areas-terapeuticas/dermatologia/urticaria/recursos-medico/cuestionario-uct) and/or cell phone applications (e.g. UrticariApp) are available free of charge to calculate this score.
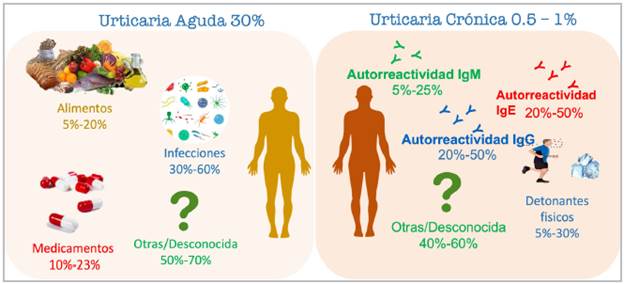
Figure 2 Causes of acute and chronic urticaria. (Acute urticaria may affect one in three patients. Its cause is often not identified, but it should be suspected in the context of infections, for example, after infections with SARS-CoV-2 and other viruses). In chronic urticarias, concomitant spontaneous and inducible urticarias are also frequently found.
HOW DO I CLASSIFY URTICARIA ACCORDING TO ITS LEVEL OF CONTROL?
The UCT evaluates urticaria control according to the response to pharmacological treatment. This scale contains questions which determine if the disease is "controlled" (12 or more points) or "not controlled" (11 or fewer points) 16. The abbreviated UCT consists of four simple questions 17 with a maximum score of 16 points (Table 4). The minimum clinically important difference is three points. Lack of control on the UCT or on the UAS7 indicates a need for treatment adjustment, and this is why it is important to apply them at each office visit. Various web pages (e.g., https://www.profesionalessanitarios.novartis.es/areas-terapeuticas/dermatologia/urticaria/recursos-medico/cuestionario-uas) and/or cell phone applications (e.g. UrticariApp) are available free of charge to calculate this score.
Some other symptoms can indicate severe urticaria, and referral to an urticaria specialist should be considered (Figure 3). Up to 20% of patients with chronic urticaria can have associated symptoms such as respiratory distress similar to anaphylaxis. However, these events tend to not be repetitive, and thus should not be managed chronically, but rather just during the acute event. If, on the other hand, the event is repetitive, the patient should be urgently referred to an urticaria specialist, preferably an allergist. Some patients may occasionally develop symptoms such as joint pain, fever or dizziness, or may report residual skin lesions. Once again, if these events are repetitive, they should be referred to an urticaria specialist, preferably a dermatologist.
BARRIERS IDENTIFIED
Primary care physicians do not make much use of the clinical scales for urticaria, which makes it difficult to clearly determine the severity of the condition.
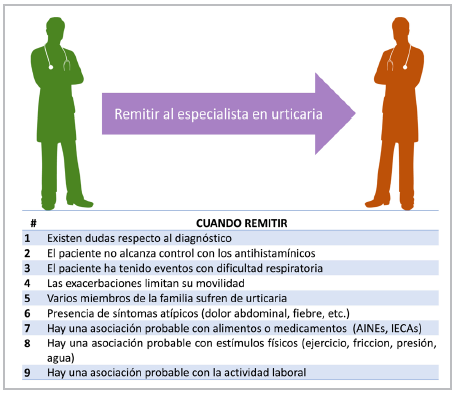
Figure 3 When to refer. (If one of the previous points is found, consider referring to the dermatologist and/or allergist. NSAIDs: nonsteroidal anti-inflammatory drugs. ACE inhibitors: angiotensin-converting enzyme inhibitors).
SOLUTION
The use of simple disease-specific clinical scales and awareness of warning signs that encourage ruling out other diagnoses help correctly stratify the disease and level of control provided by each patient's pharmacological treatment. The use of a common language within the medical team facilitates communication between the different care levels and streamlines the patients' appropriate treatment. Access through web pages, cell phone applications, etc., facilitates the use of these scales.
TREATMENT RECOMMENDATIONS
Urticaria has a high impact on quality of life but tends to be self-limiting; acute urticaria disappears within the first six weeks and chronic urticaria tends to resolve in 50-80% of cases within the first five years 18,19. Therefore, the goal of urticaria treatment is to control the symptoms of the disease until it disappears. The steps for pharmacological treatment are found in Figure 4. During primary care, physicians can begin with second generation antihistamines and identify possible triggers. This applies both to outpatient care as well as emergency and inpatient care. Below, we will discuss first line management, which includes avoidance measures and the use of antihistamines. Then we will mention other therapies and treatment in a few special groups.
WHAT SHOULD A PATIENT WITH URTICARIA AVOID?
Due to its spontaneous appearance, patients with urticaria often associate the onset of the events with multiple stimuli (20). However, in most cases, these associations are not relevant to the disease, and avoidance measures are therefore unnecessary. The patient must be asked if the events also occur spontaneously or only when they are exposed to a given stimulus. If the patient associates the events with a stimulus, it is also important to ask if the events always occur with exposure to the stimulus or only sometimes. When the patient has spontaneous events which also sometimes occur with the suspect stimulus and sometimes not, a causal association is unlikely, and it should be considered spontaneous urticaria.
On the other hand, if the patient strongly suspects a given stimulus and reports that the event is recurrent with exposure, restrictive measures are needed until the patient undergoes confirmatory tests by an urticaria specialist (Figure 3). As mentioned previously, urticaria may sometimes occur secondary to exposure to a physical stimulus (in the case of chronic urticaria), or to food or medications (in acute urticaria). In these cases, if the acute events recur with further exposure to the suspected stimulus, these patients should be referred to an allergy specialist, as the urticaria may be a symptom of food or drug allergies.
BARRIERS IDENTIFIED
Patients often impose restrictions on themselves with no clear evidence of their usefulness, based on their own decisions, informal information from nonmedical sources or even, at times, medical recommendations which in most cases do not contribute to improved clinical control. This increases the burden of the disease as it affects the patients' quality of life and social and recreational interaction.
SOLUTION
A correct assessment of the suspected triggers identified by the patient helps avoid unnecessary restrictions. If a trigger is identified which may be related to the clinical condition (e.g., foods, medications or physical stimuli), the patient must be referred to a specialist.
WHAT IS THE APPROPRIATE PHARMACOLOGICAL TREATMENT FOR URTICARIA?
The symptoms of acute and chronic urticaria are mainly mediated by the action of histamine on the H1 receptors located in the endothelial cells of the skin. Therefore, histamine blocking is central to urticaria treatment. The continuous use of antihistamines in acute and chronic urticaria is supported by the results of several studies which show their high efficacy, effectiveness and safety even after several years' use 5,9. Currently, no urticaria or rhinitis guideline supports the use of first-generation antihistamines due to their frequent side effects, interactions with other medications or foods, and lack of clearly superior efficacy over second generation antihistamines 9,21. Among the most frequently reported side effects are their sedative and anticholinergic effects, and their effects on the quality of sleep, concentration and motor skills. All of these effects are uncommon with second-generation antihistamines like loratadine, desloratadine, cetirizine, levocetirizine, fexofenadine, bilastine, and rupatadine, among others.
The initial dose in all patients is the usual daily dose according to age (Table 5). If after at least one month of daily use no relevant symptom improvement is found on the UAS7 and/or UCT, a second line of treatment should be considered, consisting in increasing the dose to up to four times the usual daily dose (Figure 4). This measure has proven beneficial in various studies 22-25. It is important to emphasize that the increased dose does not significantly increase the risk of side effects. If control is not achieved after at least one to three months of treatment, referral to an urticaria specialist should be considered.
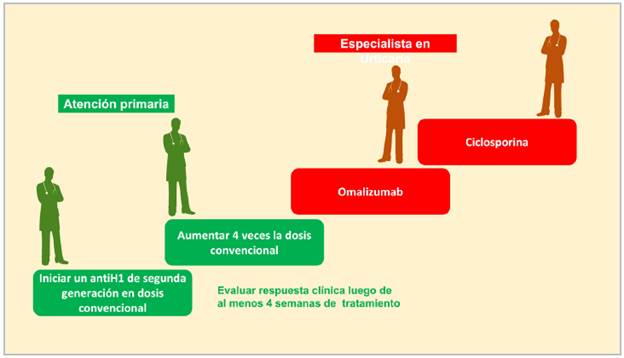
Figure 4 Treatment steps. (Each treatment step is added to the following one according to the patient's control. The recommended evaluation period with antihistamines is at least four weeks. If there is no response, an increase of preferably four times the conventional dose is recommended.)
If the patient has had urticaria for less than six weeks, antihistamines should be recommended for at least one or two months. If the patient stops having welts and/or angioedema, withdrawal can be considered. On the other hand, if the patient has had urticaria for more than six weeks or still has pruritis, welts or angioedema, even if they are occasional, treatment should be extended for at least six months and suspension considered only when the patient has experienceed three to six months without skin lesions and without moderate or intense pruritis.
Omalizumab is an anti-IgE biologic medication which is effective and safe for treating chronic spontaneous or inducible urticaria. Real-life studies have shown that cyclosporine also positively affects the management of chronic urticaria, especially in patients with an unsatisfactory response to antihistamines. These two treatments should be ordered by physicians who are experts in the treatment of urticaria, like dermatologists and allergists, due to their cost and/or safety profile.
BARRIERS IDENTIFIED
Many times, treatment is applied intermittently and for less time than necessary to evaluate the clinical response and/or achieve disease control. The use of first-generation antihistamines is still common, despite having more side effects than second-generation antihistamines. Combining antihistamines is also common, which has not proven to be more effective than using a single antihistamine at a higher dose.
SOLUTION
Applying the guideline recommendations that have been summarized in this consensus facilitates the proper use of treatment, emphasizing the safety of second-generation antihistamines even at four times the conventional dose for an extended period of time.
MANAGEMENT IN CHILDREN
Management in children follows the same steps described above, adjusting the antihistamine dose according to age (Table 5). Only medications with proven efficacy and safety in the pediatric population should be used25-27. Cetirizine, desloratadine, fexofenadine, levocetirizine, rupatadine, bilastine and loratadine have been well studied in children over the age of two, and some real-life studies suggest that loratadine, cetirizine and fexofenadine can even be used in six-month-old children. For children under six months old, a case-by-case assessment should be performed to determine the need for antihistamines versus the risks.
PREGNANT AND LACTATING WOMEN
In principle, the same considerations described above apply to pregnant and lactating women, although none of the urticaria treatments have been studied in clinical safety trials in pregnant women. Some real-life studies allow the use of second-generation antihistamines to be recommended, especially loratadine, cetirizine, desloratadine and levocetirizine 28,29. There are no studies available during lactation, either; however, some real-life observations with loratadine, cetirizine and fexofenadine seem to indicate a low risk for mothers and infants 30. If a patient has chronic urticaria and is on second-generation antihistamines when she finds out she is pregnant, it does not appear to be necessary to change the medication, regardless of the one being used. However, if control is not achieved and she requires a higher dose, we suggest changing to one of the previously mentioned drugs.
Table 5 Conventional antihistamine doses.
| Antihistamine | Adults | Children |
|---|---|---|
| Loratadine | 10 mg/day | 0.2 mg/kg/day |
| Cetirizine | 10 mg/day | 0.2 mg/kg/day |
| Levocetirizine | 5 mg/day | 0.1 mg/kg/day |
| Desloratadine | 5 mg/day | 0.1 mg/kg/day |
| Fexofenadine | 180 mg/day | 6 months to 2 years: 30 mg per day. 2 to 11 years: 30 mg twice a day. |
| Rupatadine | 10 mg/day | Children 2 to 11 years old (>25 kg): 5 mL/day Children weighing >10 kg and less than 25 kg: 2.5 mL/day |
| Bilastine | 20 mg/day | 6-11 years old with a body weight of at least 20 kg (4 mL of oral solution) |
The daily dose is presented by age. Subject to availability in each country.
BARRIERS IDENTIFIED
The diagnosis and treatment of urticaria in children and pregnant women causes concern. Early suspension of treatment in an effort to reduce the risk of side effects causes relapses and affects the patients' quality of life.
SOLUTION
Real-life studies suggest that continuous treatment at appropriate doses is secure and effective in managing urticaria in special groups.
EMERGENCY CARE
Up to 20% of the initial care of patients with urticaria is given in the emergency room, due to patients' fear caused by the sudden onset of the condition and their search for quick care. During their stay in the emergency room, the patients should be stratified, and the previously mentioned history taken (Figure 1, Tables 2, 3 and 4). The treatment steps are also the same (use of antihistamines as the first and second line of treatment) (Table 5). If the patient has not begun this treatment, administration of an H1 antagonist may be started in the emergency room until the outpatient follow-up, with referral to a primary care physician. If the patient has been taking an antihistamine in a single dose, but has not achieved adequate control, the dose can be raised, and a referral made to primary care. The effect of the antihistamine is generally seen within the first two hours, during which the patient can be kept under observation, if the physician deems it appropriate.
If the patient has already taken these steps and control has not been achieved, or if there is a warning sign (respiratory distress, mobility problems, etc.), after ruling out possible differential diagnoses which would require a specific treatment (e.g., adrenaline for anaphylaxis), a short cycle (no longer than five days) of a systemic steroid may be administered, adjusted to the patient's weight, and priority referral to an urticaria specialist should be considered.
BARRIERS IDENTIFIED
Many patients who have not received basic urticaria treatment go to the emergency room because they do not find rapid access to ambulatory care and/or are afraid. Steroids tend to be administered in the emergency room without appropriate patient stratification, and sometimes patients are not referred for outpatient monitoring.
SOLUTION
Knowledge of the proper diagnosis and treatment of urticaria will allow more effective management in the emergency room and promote an appropriate referral according to the severity of the condition. The use of systemic steroids should be restricted to patients who have not responded to the maximum dose of antihistamines. If the condition is accompanied by respiratory distress, other processes such as anaphylaxis should be ruled out.
FOR ACUTE URTICARIA
Due to its self-limiting nature, laboratory tests are not usually needed, unless a differential diagnosis (infection, urticarial vasculitis, anaphylaxis) or causal agent (e.g., infection, food or drug allergy) is suspected.
FOR CHRONIC URTICARIA
A complete blood count is recommended for all patients, along with acute phase reactants, total IgE and anti-TPO IgG antibodies. However, they are not indispensable in primary care and they may be restricted to cases being managed by urticaria specialists, who will interpret them according to each patient's context and complement them with other tests, if needed. For example, for patients with a strong suspicion of triggers such as foods, medications, physical stimuli, etc., referral to an allergist is recommended for specialized confirmatory tests (allergy skin tests, drug or food challenges, physical urticaria tests) or to a dermatologist for a biopsy if urticarial vasculitis is suspected.
DISCUSSION
The consensus identified various barriers which keep the primary care physician from providing the proper treatment to patients with urticaria. Specific recommendations are provided for each of these barriers based on the international guidelines. Most of the barriers result from confusion regarding how to make the diagnosis, when the patient should be referred to a specialist, and the initial treatment with antihistamines.
The application of the consensus could improve primary care physicians' skill in treating patients with urticaria and avoid delays with unnecessary referrals or beginning inappropriate management such as food or drug restrictions which usually have little impact on the disease.
The external validation performed by presenting the document constructed by the panel to members of the various participating societies confirmed that the identified barriers had a significant negative impact on patient management. There was also a positive reception regarding the feasibility of making the pertinent corrections with the proposed solutions. External validation also allowed some specific barriers to be identified, such as emergency room care or consultations in special populations.











 texto em
texto em