Introduction
Postanesthetic excitation, awakening, and postoperative agitation are terms used interchangeably to describe restlessness, agitation, crying/moaning, disorientation, incoherence, and even paranoid ideation in a patient. Although it is usually short-lasting and self-limiting, delirium may require pharmacological intervention (52%), result in physical damage, delay reunion between the child and the parents, and prolong the stay in the postanesthetic care unit (PACU).1,2
Findings of varying incidences in pediatric patients have not only limited widespread knowledge but also the study and implementation of preventive and therapeutic measures during postanesthetic recovery. Many variables have been implicated, but only a few have been found to be true risk factors for delirium (head and neck surgery, patients under 5 years of age, and exposure to halogenated agents).1,3-6 In contrast, pain has been correlated as a risk factor for delirium, and, consequently, some analgesic therapies have already been tested in an attempt at reducing its presence and severity.6-11
This study was designed with the aim of determining the size of the problem in this population and assessing different variables that might modify its incidence. The incidence of delirium in the pediatric population and independent, múltiple, protective, or risk associations were studied.
Materials and methods
Having received the approval of the Research and Ethics Committees of the San José Children's Hospital and FUCS, a prospective observational analytical study of an incident cohort was designed to include patients between 2 and 10 years of age, American Society of Anesthesiology (ASA) I to II, taken to low-risk surgeries (surgical and bleeding risk), including head and neck, urologic, orthopedic, imaging, and gastroenterology procedures. Patients with neurological disorders or sequelae, a need for postoperative mechanical ventilation, and with incomplete follow-up were excluded.
Taking an incidence of delirium of 33%,1 accuracy was calculated at 5% confidence at 95%, and sample size at 340. To adjust for risk factors, based on a difference of 20% between the proposed stratified and raw incidences, a 95% confidence and a power of 80% (n = 59) was estimated for every factor to be analyzed (maximum of 4 variables).
The incidence of delirium was calculated as a percentage of exposed cases. Those incident cases were subjected to different stratified assessments. Demographic data and intraoperative variables are presented. The type of anesthesia, induction, maintenance, extubation, and analgesia were recorded. The medications used intraoperatively were identified and classified, and the confounding effect was assessed and analyzed by means of a stratified analysis.
On arrival at the PACU, delirium (Pediatric Active Enhanced Disease Surveillance [PAEDS]) and pain (Children's Hospital of Eastern Ontario Pain Scale [CHEOPS]) were assessed. The Aldrete score was determined on admission, and patients with Aldrete score 10 in the first 10 minutes were stratified. The assessments were repeated at 20 and 40 minutes. In the event of delirium or pain, the treatments used were documented (in the PACU).
The PAEDS values were stratified and matched with the presence of acute postoperative pain to explore the delirium diagnosis group exposed to pain. An exploratory bivariate analysis of variables listed in the outcomes tables was performed to find an association between delirium and acute postoperative pain. Variables with a P value <0.2 in the bivariate analysis were entered into a logarithmic regression model for a maximum of 4 variables, to generate an association model. Delirium versus acute pain (chi-square), and remifentanil versus acute pain (chi-square) were assessed. Differences were considered statistically significant if P < 5%. Finally, impact measurements for variables with statistical significance were calculated (relative risk [RR], number necessary to harm [NNTH]). The STATA 14 (StataCorp) software package was used.
Results
Overall, 340 records were collected prospectively and sequentially as of the second semester of 2016 (see Table 1 for the demographic and preoperative characteristics). Evaluation quality was secured through training for administering and interpreting the scores. Moreover, the researchers provided advice and recorded the secondary database prospectively and concurrently.
Table 1 Demographic characteristics.
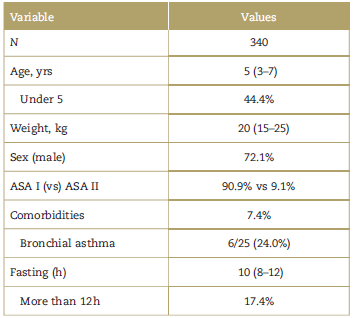
Values presented as means/medians and standard deviation or 25 to 75 range, or frequencies and percentages. ASA=American Society of Anesthesiology.
Source: Authors.
Ninety per cent (90%) of the patients were taken to orthopedic, urological, otolaryngological, and pediatric surgical procedures (Table 2), and 16.5% were taken to head and neck surgery. Four patients (1.2%) received dexmedetomidine 0.97 |xg/kg (±0.15 mg/kg) and 2 received midazolam 0.11mg/kg (±0.04mg/kg) during induction.
Table 2 Surgical procedures (n = 340).
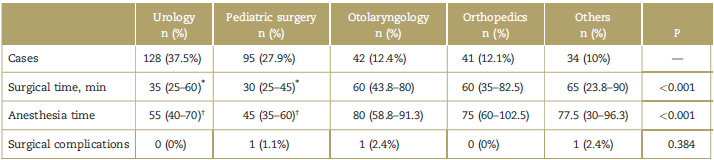
Frequency, average anesthesia time, surgical time, and complications are included (scatter is shown as percentile range (25%-75%).
* P=0.005.
† P < 0.001 as compared with other surgical groups.
Source: Authors.
The most common anesthetic induction model consisted of sevoflurane-fentanyl-propofol (54.1%), followed by sevoflurane-fentanyl (13.2%) and sevoflurane-propofol (12.4%). The most common anesthesia maintenance model was fentanyl-sevoflurane (58.2%), followed by a total inhalation model (sevoflurane) (15.3%), fentanyl-desflurane (10.9%), and remifentanil-sevoflurane (10.3%). The halogenated agents most frequently used were sevoflurane (81.5%) and desflurane (18.5%). In 100% of cases, halogenated agents were used for maintenance.
The strategy most commonly used for intraoperative analgesia was a single fentanyl bolus (37.4%), followed by fentanyl-remifentanil-halogenated (31.8%), sevoflurane (15.3%), and remifentanil-halogenated (13.2%). Dexameth-asone was given to 60% of the patients. Nonsteroidal anti-inflammatory agents (diclofenac 1.1mg/kg [±0.025] or dipirone 21.4mg/kg [±0.9]) were used in 87.7%; additionally, 9.1% (27/298) received morphine 0.06mg/kg (±0.004), 13.1% hydromorphone 0.01 mg (±0.001), and 13.8% tramadol 1.61 mg/kg (±0.06). Tramadol was used 50 times (14.7%), but singly in 3 patients. A total of 22.1% of patients received regional analgesia (plexus, major nerves, or caudal analgesia); 20.3% were extubated while still in deep plane.
The incidence of delirium in the PACU was measured at 0,20, and 40 minutes. The incidence of pain was measured at the same time (Table 3). The mean PAEDS score was 5 (0-7), 3 (0-5), and 0 (0-3) at 0, 20, and 40minutes, respectively.
Table 3 Postoperative delirium in pediatrics.
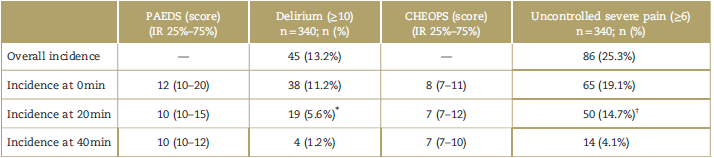
Overall: presence of delirium during the first 40 minutes in recovery.
CHEOPS=Children's Hospital of Eastern Ontario Pain Scale; IR=interquartile range 25%-75%; PAEDS=Pediatric Active Enhanced Disease Surveillance.
* Eight of the 18 cases of delirium (44.4%) were diagnosed for the first time at 20 minutes; of the 18 cases with delirium, 44.4% were diagnosed for the first time at 20 minutes.
† Twenty-one of the 50 cases with uncontrolled severe pain (42%) were diagnosed for the first time at 20 minutes.
Source: Authors.
A bivariate analysis was performed for sex, age, patients under 5 years of age, ASA, and comorbidities, but no statistical significance (P > 0.05) was found for any of these variables. A bivariate analysis was also performed for the sociodemographic, surgical, and anesthetic variables, and an association was found with the outcome of interest for surgical time (P = 0.026) and anesthesia time (P = 0.037). Data associated with dexmedetomidine and midazolam were excluded due to the low frequency of their use; however, it is worth highlighting that they were not associated with delirium. Only 1 patient required specific pharmacological management for delirium, which was controlled with propofol-ketamine (at 20 minutes).
The Aldrete score at 0 minutes was 9 (8-9). The mean recovery time (Aldrete score 10) was 10 minutes (5-20), and 54.1% reached that level in less than 10minutes (PACU). The presence of uncontrolled severe acute pain was assessed at 0, 20, and 40minutes, using the CHEOPS score (Table 4). There is evidence of clinical differences in all the strata of the analysis; however, differences were significant only on admission to the PACU, and in the global delirium measurement (defined as delirium within the first 40 minutes in the PACU).
Table 4 Pain versus delirium in the postanesthetic care unit.
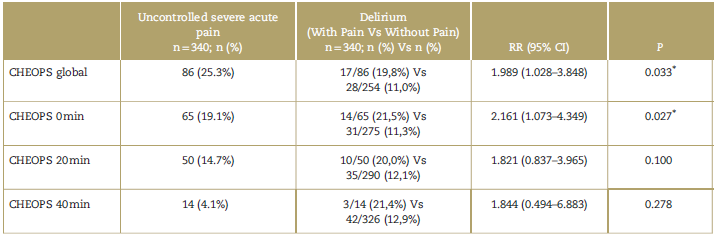
Column "n" includes the cases of severe acute pain.
CHEOPS=Children's Hospital of Eastern Ontario Pain Scale; CI=confidence interval; RR=relative risk.
* P < 0.05.
Source: Authors.
When staging different strata of postoperative pediatric delirium (10-12/13-16/>16) for practical purposes (low/ intermediate/high, respectively), it was found that, on admission to the PACU, 44% of the individuals with low PAEDS score had pain, 70% with intermediate PAEDS, and 100% with high a high PAEDS. This revealed statistically significant differences between the low level and the intermediate/high level (P = 0.035). At 20minutes, 66.7% of the individuals with low PAEDS and 75% with intermediate PAEDS had diagnostic values on the CHEOPS scale (P= 0.627). Finally, none of the patients had pain at 40 minutes.
Stratified incidences of acute pain associated with the intraoperative analgesic strategy were calculated in surgery. A comparative analysis between analgesic strategies for this cohort and their impact was added, highlighting the incidences of uncontrolled acute pain stratified to the use of remifentanil versus other analgesic strategies used (Table 5).
Table 5 Analysis of the intraoperative analgesic strategy versus incidence of uncontrolled severe acute pain.
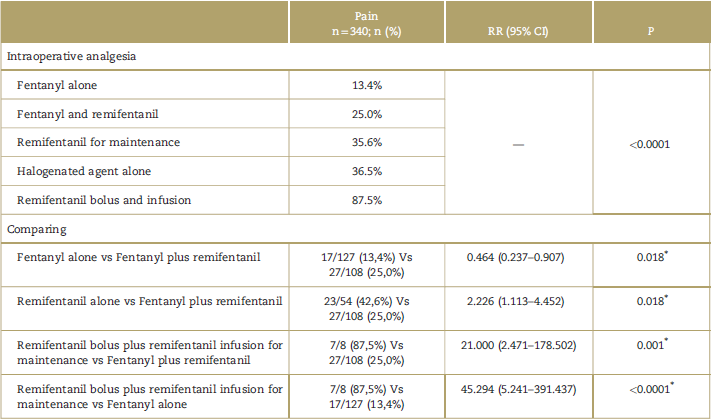
CI=confidence interval; RR=relative risk.
* P < 0.05.
Source: Authors.
When controlling for the confounding effect (logistic regression) for the type of induction, the anesthesia maintenance strategy and the intraoperative drugs (hydromorphone-midazolam-dipyrone-morphine-fentanyl-propofol), no variable had statistical significance for delirium. The patients who received various analgesics (hydromorphone-diclofena-tramadol-ketamine) were analyzed using multiple logistic regression, and in this way they were excluded from an association model because of the lack of final statistic impact for the presence of delirium.
The incidence of delirium was higher among individuals who received dexamethasone (16.7% vs 8.1%; P=0.015; RR 2.273; 95% confidence interval [CI] 1.108-4.660) and (odds ratio [OR] 2.273; 95% CI 1.108-4.660). When multiple logarithmic regression was included, of the variables with statistical significance (P < 0.2) related to the development of delirium, only dexamethasone (OR 2.398; 95% CI 1.1395.050) maintained the association, whereas head and neck surgeries (OR 1.546; 95% CI 0.707-3.383) did not generate a multiple association.
Concerning uncontrolled acute pain (postoperative), the analysis found that none of the analgesic medications showed statistical significance in relation to multiple statistical analysis. Finally, it was found that the patients who received dexamethasone had a lower incidence of uncontrolled pain in the PACU (21.6% vs 30.9%; P=0.057; RR 0.62; 95% CI 0.38-1.008). The analysis (logistic regression) showed a similar statistical significance (P = 0.054; OR 0.61; 95% CI 0.376-1.01). Although they could not be considered significant, these findings are clinically relevant.
Discussion
This research study found a low incidence of pediatric delirium (13.2%) associated with procedures with low surgical risk, which challenges the high incidences detected by Bock et al12 (38%), those calculated by Smessaert et al13 (8%, between 11 and 17 years), and those reported by Gooden et al14 (19.3%). Although various indices have been used for this outcome in the world literature, it is important to consider the origin of those results. For years, the diagnosis of delirium was based on appreciations with no consensus, and, consequently, expert opinion on the subject was the only tool available. This did not only limit the ability to derive inferences, but it also challenged the diagnostic criteria of each of the studies. The statistics estimated by Dahmani et al,7 JOHr,15 and Voepel-Lewis et al1 are clear examples of these assertions (incidences 2%-80%). However, with the advent of validated scores like the PAEDS, the objectivity and validity of the research were enhanced. A case in point is the study by Pieters et al,9 which found an incidence of delirium of 18% applying this tool.
The population in our study showed a lower rate than that reported for the world (and for the region). We suggest that the use of a specific calculation for the search of delirium under clear criteria, resulted in 1 of the largest samples reported in the literature, providing more accurate statistics for the study.
It is worth noting that the diagnosis of delirium was not made only on admission to the PACU, because an important proportion of patients showed delirium at 20 minutes (44.4%). It needs to be underscored that 1.2% of the cases showed persistent diagnostic criteria for delirium during 40 minutes, pointing to a trend of short-term recovery. Despite the severity of the pictures, no patient developed complications, adverse events, or required additional treatment.
Several authors have discussed multiple risk factor for delirium. According to the bivariate analysis of this report, anesthesia time (RR 1.01; 95% CI 1.002-1.019), surgical time (RR 1.013; 95% CI 1.003-1.022), and the use of dexamethasone (RR 2.273; 95% CI 1.108-4.660) were associated with the outcome, but this was not replicated in the logistic regression.
Aono et al16 stated that patients under 5 years of age exposed to similar anesthetic models with sevoflurane showed a higher rate of delirium (40% vs 11.5%; P = 0.032), unlike our reported bivariate analysis (12.6% vs 13,8%; P= 0.440). Aono et al16 concluded that central nervous system immaturity and the effect of "early emergence" in an unknown setting were the causes of delirium. In this study, the rate of delirium was not increased in children under 5 years of age; moreover, the assertion on "early emergence" is refuted, given that no statistically significant differences regarding delirium were found between patients with a score of 10 on the Aldrete scale (within the first 10 minutes in the PACU) and patients with deep-plane extubation and late emergence. Sevoflurane and desflurane have been ruled out as delirium inducers.17 Viitanen et al18 showed a higher incidence of delirium with halothane versus Thiopental (sodium) (29% vs 7%; P< 0.01); however, that evidence was not replicated when halothane was compared with propofol (29% vs 23%; P= 0.07). Notwithstanding, he also suggested that a higher probability of delirium was associated with that inhalation agent.
In contrast, Pieters et al9 compared propofol versus sevoflurane in relation to delirium in patients taken to adenotonsillectomy, and concluded that there was a high raw incidence, despite higher diagnostic cut-off points (PAEDS score >13), but did not find significant differences (63% vs 53%; P > 0.05). Our study supports his conclusion in relation to inhalation anesthetics (alone/combined; induction/maintenance; sevoflurane/desflurane), which did not modify the incidence of delirium.
The analysis of "total intravenous anesthesia" (fentanyl-propofol) compared with other anesthetic strategies showed a dramatic increase. However, this comment needs to be taken with great care, as it is derived from a small sample of patients in this subgroup (n = 8). A larger sample size needs to be analyzed.
For years, head and neck surgery has been considered a risk factor.17 However, numerous authors have discussed dissimilar figures. Kotiniemi et al and Holm-Knudsen et al have not made reference to it as a risk factor for delirium,19-21 and Kain et al22 even stated that there were other subgroups with a higher risk (urogenital surgery). Consistent with this reference, the head and neck surgery subgroup did not show a significant association with delirium (P = 0.182) in this study.
Dexamethasone during induction was associated with delirium (16.7% vs 8.1%; P=0.015; RR 2.273; 95% CI 1.1084.660); after the logarithmic analysis, a relevant statistical significance with an important explanatory percentage was published. For the discussion of these findings, a systematic search of the literature was conducted in the Pubmed database (Metadata: Dexamethasone_AND_children_AND/ OR_Dexamethasone_AND_Delirium), with no restrictions. Four articles related to the topic were found, but only 1 applied to pediatric patients. In a placebo-controlled clinical study, Khalili et al23 assessed delirium after the use of dexamethasone (0.2mg/kg) and reported lower incidences (60% vs 85.7%; P=0.016). However, when analyzing dexamethasone versus acetaminophen-codeine for delirium, the author did not find differences (60% vs 65.7%; P = 0.752). Despite little evidence regardingthe effect of dexamethasone on the outcome of interest, the literature does not provide sufficient data to rule out its role. Our conjectures do not only revive a controversy but also seek to promote a scientific debate to solve this dilemma.
Unlike other clinical settings, tight monitoring of physiological responses to surgical stimuli in our patients, and titrated administration of the analgesics according to multiple responses during surgery, ensured an objective assessment of the effects of the analgesic techniques, allowing us to analyze their triggering or protective effect in terms of postoperative delirium. However, although it is impossible to consider that this assertion is unquestionable, because of the neuromodulation caused by the concurrent administration of hypnotic and amnesic agents, it would be unethical to consider experimental settings in which individuals would be exposed to intraoperative pain with the aim of consolidating observations and assessments in the absence of strong analgesics. Therefore, should a similar measure of delirium exist, it is derived for practical purposes from similar anesthetic models, rendering additional searches for the study of that temporality unnecessary.
Several authors consider acute postoperative pain as an important risk factor for delirium.1,4,8 In fact, severe acute pain during recovery was closely associated with delirium in this cohort. At 0 minute (admission to the PACU), pain behaved as a risk factor (55.3% vs 14.6%; P < 0.0001; RR 7.243; 95% CI 3.544-14.805; NNH 3.83). A similar behavior was found at 20 minutes (26.0 vs 2.1%; P < 0.0001; RR 16.623; 95% CI 5.960-46.407; NNH 4.18), but not so at 40 minutes (0.0% vs 1.2%; P = 0.845). This information is very clear and, therefore, supports 1 of the main assumptions of this study: pain is perhaps the most important risk factor for postoperative delirium in pediatric patients.
Various authors have argued that optimal analgesia (preventive/therapeutic) could lower the incidence of delirium in the PACU. In fact, Bock et al12 showed that clonidine (3 mg/kg epidural or intravenous) may reduce the rate of delirium (0% and 5% vs 39% for the control group; P = 0.01). In turn, Davis et al4 found lower rates of delirium for short procedures with ketorolac (independent from the inhalation agent: halothane-ketorolac 12% vs halothane-placebo 42%; P < 0.05; and sevofluorane-ketorolac 14% vs sevofluorane-placebo 38%; P < 0.05).
We recommend caution regarding these assertions, not with the aim of disputing the use of excellent multimodal strategies for the prevention and treatment of pain in children or to contradict ourselves when saying that some analgesic regimens have no effect on the rate of delirium. What we suggest is that the association between pain and delirium in this study does not point to a potential measurement bias, given the similarity of diagnostic items used in each score (PAEDS and CHEOPS); therefore, the association may be due more to the similarity of criteria and not necessarily to the diagnostic agreement between 2 clinical pictures in the same patient. Moreover, despite the use of regional analgesia in a significant number of patients, it was not associated with a lower incidence of acute postoperative pain, which is consistent with a potential misdiagnosis of pain or delirium, not comparable with what was found and discussed as valid by other authors. Consequently, it was sensible to cancel the performance of additional statistical analyses. Further controlled clinical trials are needed in order to be able to discuss those effects.
In view of the above, it is imperative to consider medications that protect against delirium and/or severe acute postoperative pain as part of the study design. Although measuring the effects of a given pain prevention strategy was not the objective of this study, in none of the cases were those preinduction measures used. Moreover, to strengthen this hypothesis of a causal relationship, we recommend the inclusion of numerical scales to weigh the intensity of pain in relation to delirium.
Finally, the analysis of delirium regarding the use of remifentanil (induction and/or maintenance) did not show causality. However, an association was found between remifentanil and severe acute pain. Although the ability of strong opioids to produce hyperalgesias has been the subject of debate for many years, there are currently few studies that refer to this fact in the pediatric population. Hyperalgesia secondary to the use of opioids, although new, has limited the options for opioid-based therapy. Since the in vitro studies by Zhao and Joo24 which showed evidence of lower thresholds for N-methyl-D-aspartate (NMDA) receptor excitation after the use of remifentanil, various studies, from different perspectives, have suggested similar hyperalgesia.25-28
This evidence provides arguments to dispute the use of remifentanil in pediatric patients, and it can even propose mechanisms to modulate its sensitizing effect by means of the use of analgesic drugs with major gamma half-life or uneven action mechanism.
Despite the magnitude of the statistical differences and their impact measurements (RR = 45.29/NNH = 1.35), it is important to note that those data come from a small sample, smaller than the necessary minimum to establish a causal association. Consequently, we suggest collecting a probabilistic sample that is sufficient to solve this uncertainty. In the meantime, we believe it is of great value to consider the concomitant use of hyperalgesia modulators with remifentanil.
Conclusions
Even though this is not the first study on this topic of research, we believe it is 1 of the first in the region that provides a clear incidence of delirium in the pediatric population. This incidence is low when compared with other reports in the world literature. However, we dispute the diagnostic strength of the scales used, given the similarity of their measurement parameters, and we believe it is crucial to develop a specific study regarding this matter. Dexamethasone was found to induce delirium, but further evaluations are needed to arrive at a conclusion. The association between pain and delirium is unquestionable and it is consistent with the evidence in the rest of the world. Finally, remifentanil may favor the presence of severe acute postoperative pain (hyperalgesia), something that needs to be verified with a larger sample and a specific methodology design for such a theory.
Ethical disclosures
Protection of human and animal subjects. The authors declare that the procedures followed were in accordance with the regulations of the relevant clinical research ethics commit-tee and with those of the Code of Ethics of the World Medical Association (Declaration of Helsinki).
Confidentiality of data. The authors declare that they have followed the protocols of their work center on the publication of patient data.
Right to privacy and informed consent. The authors declare that no patient data appear in this article.











 texto em
texto em 


