Introduction
Structural changes must be introduced in the care model currently used with patients requiring surgical treat ments.1-5 Proposed changes include eliminating silos, and focusing on meeting the needs of the patient, the caregivers and the community. The first of these changes requires going back to integrated health systems and adding primary and home care settings to the daily practice of the anesthetists.6-11 The second change requires an expansion of the horizon for assessing the outcomes of perioperative care to consider long-term results.12-15 Moreover, it means gaining new competencies, in particu lar non-technical skills16,17 (assertive communication, teamwork, professional and institutional leadership, and awareness of social conditions), and systematizing the non-declarative knowledge gained so far after a century of practicing the "art of anesthesiology".18
This means that, although many specialties in medicine tend to shrink their field of action, anesthesiology tends toward expansion.19,20 Predictions regarding the develop ment of traditional medical and surgical specialties in the near term point toward more encapsulated and deeper scientific knowledge limited to certain diseases, focused procedural skills with a high degree of interaction with technology, and concentrated competencies for highly controlled and systematized workplaces designed for the care of selected population groups.21 In contrast, predic tions on the future of anesthesiology point to in-depth knowledge of social sciences, optimization of non-techni cal competencies and non-declarative knowledge (art), expanded settings for daily practice, longer care time, and a greater number of people and situations needing our services.22-24 Predictions also tell us that the areas of greatest interest for perioperative medicine in the 21st century will be complex studies with large databases on long-term outcomes, innovations in information technol ogy and telecommunications, and advances in bioethics and health economics.25,26 This is so as the most significant challenges foreseen will have to do with providing high-quality, timely, and equitable surgical care for the entire population, with increasingly limited access to specialized care and with insufficient resources. The objective of this reflection article is to describe the issues with the current model, analyze proposed solutions and the results observed during their implementation, and to point to the changes that we should begin to implement. After posing a series of questions related to this process and attempting to answer them, the conclusion is that we must ready ourselves immediately to face the changes that will surely come our way over the next decade.
Why should we expand our horizon?
As health economics analysts tell us that the current landscape is not viable. Global spending in health doubled over the past 2 decades, reaching 10% of the gross domestic product (GDP) at a global level, ranging between 5% in the poorest countries and 15% in the richest; at least half of health spending goes to surgical care, and 3/4 is concentrated in 10% to 20% of the total population, represented by elderly individuals with multiple comorbidities. In Colombia, health spending in 2003 accounted for 5.9% of the GDP, and the annual per capita spending in health amounted to $156 USD; in 2012, spending repre sented an increase of 1% in the GDP (6.9%), but the per capita cost increased by 300% ($476 USD); these figures are approximately 1/2 of those reported by the United States of America (mean spending amounting to 12% of the GDP and per capita spending amounting to $1000 USD)27 where forecasts are that health spending in 2030 will account for 25% to 30% of the GDP and the per capita cost will be $9000 USD.28 For this reason, they claim that the financial situation of the social security systems cannot wait the usual50years the scientific community has taken to adopt new trends, or the 1 or 2 decades that professionals normally take to assimilate new behaviors.29 The main arguments to justify the call for an immediate change of model are the growing gap between income and expenses in the health sector, the poor results observed when comparing health services with other service sectors, the dissatisfaction voiced by users and government leaders alike, the open mistrust among the stakeholders in the system, and the recent social and bioethical transformations.30-33
Which way ahead.?
The development of perioperative medicine as a care model has resulted in a substantial improvement in the safety34 and care of surgical patients, the expansion of clinical practice settings, and longer intervention times for the anesthetist (Table 1).35 The fundamental goals of care models, such as the perioperative surgical home (PSH),36 Integrated Health Care Routes (RIAS in Spanish),37,38 and Enhanced Recovery After Surgery (ERAS),39 are to improve individual experience with surgical care and provide comprehensive care to the patients using patient-cen tered care, objective scales that can help stratify biological risk, and emphasizing focus on care based on patient-related and procedure-related risks. These new patient-centered, comprehensive perioperative care models seek to respond to the concerns of the public and the disapproval of government leaders. They also seek to ensure that our work adds value to the care provided, as a result of less fragmentation, inefficiency, and ineffective ness, the end of the practice of defensive and reactive medicine, and the promotion of the right incentives for the various stakeholders.40,41 The ultimate goal is to solve the problems by helping with top-quality decision making.
Table 1 Characteristics of the practice of the specialty and the changes that have occurred over time
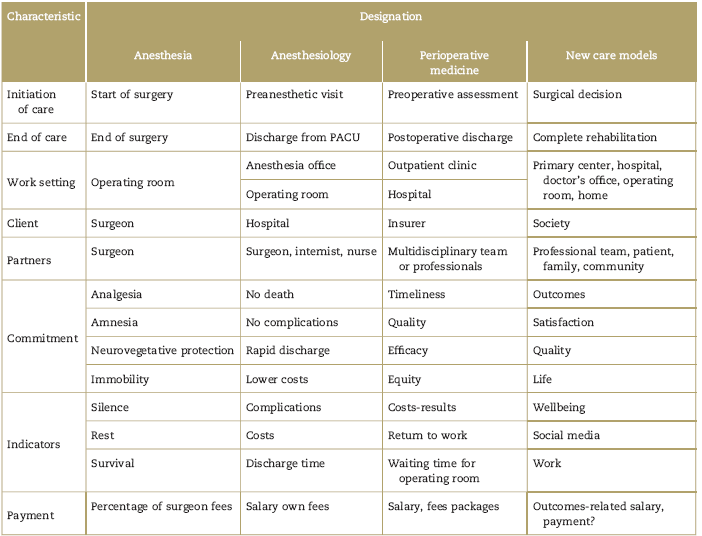
Note: Every time horizons are expanded, the designation of the job changes. PACU: Post-anasthesia care unity.
Source: Author.
In the United Kingdom, the Minister of Health received a letter signed by several presidents of professional associations and a report signed by the leaders of ERAS, summarizing the results observed up until 2013.1 This was all that was needed to adopt ERAS care in public hospital, undertake structured training programs for its implemen tation, and create a national audit system to measure its impact. Government officials accepted the suggestions of the scientific societies and mandated the inclusion of some clinical tools such as preoperative and postoperative assessment protocols focused on high-risk populations, pre-habilitation programs to optimize functional capacity and improve the expected physiological reserve before the upcoming trauma, and the adoption of RIAS to attenuate organ damage caused by surgery and optimize post operative rehabilitation.42 Over the past decade, some governments of the old British empire, the "British Commonwealth of Nations," such as Australia, Canada and New Zealand, and the countries of the Nordic Alliance (Sweden, Norway, Finland, Iceland) followed the example of the United Kingdom and included the new patient-centered comprehensive perioperative care models as part of their public health strategies designed to impact surgical care outcomes. According to reports from government agencies of those countries and of academic groups that have participated in multicenter studies, results show gradual increases in compliance with process indicators, from 25% to 30% up to 85% to 95%, a mean reduction of 2 to 3 days in length of stay, of 30% to 40% in hospital costs, and of 50% to 75% in non-surgical complications.43-45
The same concern exists in the United States of America, although the solution has been slower to come. In 2007, the National Surgical Quality Improvement Program (NSQIP) of the American College of Surgeons, based on data analysis of the process and the results, showed improvement in quality, as well as reduced morbidity, mortality, and costs. Moreover, a retrospective study carried out by NSQIP the following year concluded that creating a work team for the operating room staff was associated with improved results. In 2008, the National Institute of Medicine proposed a partnership between the public and the private sector with the aim of achieving 3 objectives: improve the experience of care, improve the health of the populations, and reduce per capita healthcare costs. In 2011, the assembly of the American Society of Anesthesiologists gave its approval for the promotion of the PSH perioperative medicine model, which resulted in a large number of publications in the American journals on the application of that model. Today, the health crisis in that country is so serious, that Klein actually compared it to an off-shore oil rig on fire, when there is no time for thinking or making adjustments and the only thing left to do is to jump into the water to save your life.46
In Latin America, there is no reliable information to determine with any certainty whether our current situa tion and our future outlook are similar, but demographic, economic, and epidemiological data show similarity with global trends. In fact, diagnostics regarding the situation of the health sector, carried out by the Colombian government, are consistent with the findings of the UK National Health Institute in the early 21st century, and the solutions set forth in the reform to the national health system, reflected in the most recent decrees passed by this administration, include the adoption of RIAS (Compre hensive Healthcare Pathways), patient-centered care, task forces for the integration of primary care with specialized levels, measurement of process and outcome indicators, and the payment of outcomes-based incentives. Presti gious hospitals in Mexico, Brazil, Argentina, and Colombia have adopted the ERAS care model with small groups of patients and follow-up periods of 6 to 12 months;47,48 according to initial reports, they had to overcome administrative and cultural hurdles similar to those found in Europe and found the same benefits in terms of shorter lengths of stay and less postoperative compli cations.
Can the new goal be achieved?
Despite government support, the commitment of the scientific societies and the admonitions of the experts, multiple barriers have come in the way of the implemen tation of the proposed changes for perioperative medicine models, with all the parties involved in surgical care arguing their own reasons to oppose the new model.49 Surgeons are suspicious of a multidisciplinary model as they fear losing control over patient management and having to share their fees. Anesthetists see it as an extension of the responsibilities of their regular job, with no clear-cut notion of what they will receive in exchange for playing a non-traditional role. For the entire team, the change means leaving the comfort of the operating theater as their natural work environment and moving into the patient's own natural environment, that is, the home and the workplace. Payers have been very stringent when it comes to incorporating new codes for authorizing proce dures under the comprehensive perioperative care model and outcomes-based incentives, as their usual response to a decision that does not fill their expectations regarding costs is to deny service access. At a managerial and administrative level, hospital directors are also fearful due to the high cost of the technology and the implementa tion, the lack of leadership and failure to involve physicians, and due also to the responsibility of main taining process changes throughout time.
However, it has been found that the best way to drive motivation for change is to start implementation and observe the results, and that the resources required to finance change may come from the savings created by the new model.50
Conclusion
Contrary to the historical trend of halting innovation implementation until safety and efficacy had been proven, government decision-makers are now open to receive suggestions and act immediately to transform them into regulations and decrees, and administrators are willing to try new models. These points to the criticality of the situation they are facing. Consequently, it is incumbent upon us to begin to gain new knowledge and build the skills required to incorporate comprehensive periopera tive care in our daily practice without delay. This is so as we will surely soon be faced with the need to work in new settings in which we will come in as novices, as is the case with primary care in the community and with home care. As anesthetists, we have to reflect on those things we need to change inside ourselves and be honest in identifying our failures and ways to overcome them.











 texto em
texto em 


