INTRODUCTION
In accordance with the United Nations Universal Declaration of Human Rights "All human beings are born equal in dignity and rights" 1. Article 25 reads: "Everyone has the right to a standard of living adequate for the health and well-being of himself and of his family, including food, clothing, housing and medical care and the necessary social services"; and then it states: "Motherhood and childhood are entitled to special care an assistance" 2. In this context, the social determinants of heatlh (SDH) understood as the social characteristics by which people live and work, support different cultural, economic and social systems and mechanisms that give rise to inequality in terms of access to goods and services such as healthcare. 3 Moreover, the SDH generate the health gradient which is present in every society, according to which the health conditions - particularly the prevalence of acute and chronic diseases - follows the distribution of the social structure. In other words, the lower the social level, the higher the prevalence of almost all illnesses and health problems. Hence, social inequality is reflected on health. 4
According to the United Nations Report on Human Development of 2019, the proportion of income between the wealthiest one fifth and the poorest one fifth of the planet, changed from 30:1 in 1960, to 74:1 in 1997. For 2006, the wealthiest 10 % had 85 % of the world's capital, while half of the population only had 1 %. 5 Additionally, studies on social exclusion, poverty and inequality in Latin America show the situation of inequality of the indigenous population and of afro-descendent groups, which originated during colonialism and under the slavery system of which they were victims. 6 Recent World Bank data show the high level of inequality existing in Colombia, which reflects in the way wealth is distributed and the poor Human Capital and Social Mobility Indexes which are particularly low among the historically neglected populations; as we shall discuss, these are determining factors for quality of neonatal surgical care in the country.
The purpose of this manuscript is to evidence the relationship between the SDHs and the quality of neonatal care in Colombia, highlighting the need for adequate training in pediatric anesthesiology, as part of the strategy to reduce health inequalities in the country.
What approaches are available to explain the relationship between social environment and health?
Two different, though complementary approaches have become popular after the second half of the 20th Century for some authors7,to address the causal relationship between the social environment and the health-disease process. One is of Anglo-Saxon and capitalistic origin, called social determinants of health, which from the ontological point of view has a functionalistic perception of society and considers that the individual is exposed to environments of social inequality leading to different living conditions; i.e., the risk is determined by the social status and health is understood as redistributive social justice, where each individual is responsible for providing for himself/herself the means to access health services. 8 Under this perspective, the State actions are addressed to intervene at the different links of the causal chain, without changing the economic model. 9 The other, which originated in Latin America under the principles of Marxism and is called social determination of health, considers that health is defined by the forces of power, domination and social inequality. Ontologically, it dimensions society as an irreducible whole where the biological is subsumed in the social and questions the core of positivism in health, causality and risk theory. It argues that the job of the State should be focused on social transformation 9; the State should solve the causes of the causes. Hence, these models present important differences in power relationships, in how ethics is conceived, and finally in the understanding of the health-disease process. 9
With the purpose of generating health equality around the world, the World Health Organization established the Commission on Social Determinants of Health in 2005. This commission provided the conceptual framework summarized in Figure 1, to explain how inequality is generated in the distribution of social goods. 8
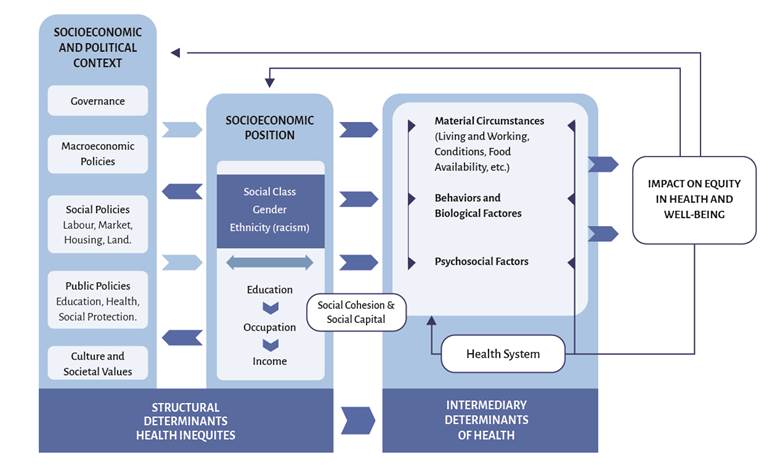
Source: WHO Commission of Social Determinants of Health. 8
Figure 1 Conceptual framework of the social determinants of health.
In Colombia, health was considered a public service delivered and/or managed by the State instead of a fundamental right enshrined in the Political Constitution. However, some jurisprudences of the Constitutional Court, when expressing their opinion about minimum livelihood and quality of life, highlighted the inseparable relationship between health and life, which means that health is a right related to life and life with dignity. 10 Additionally, following the development of the First Healthcare Decade of Colombia 2012-2022, established within the amendment to the General System of Social Security in Health (Sistema General de Seguridad Social en Salud - SGSSS) of the country (Law 1438 of 2011), health was no longer a government policy and became a State policy. The SGSSS has as a crosscutting mandate the strategy of Primary Health Care, to make a positive impact on the social and economic determinants of health in the country. 11
What is the situation in terms of neonatal mortality in the world?
Neonatal mortality is impacted by the SDHs (biological, socioeconomic, demographic, healthcare system, cultural practices and technologies, inter alia) 12, and hence it reflects the efficacy of the healthcare systems, the quality of education and the socioeconomic status of a country. Neonatal death is in most cases preventable and up to two thirds of deaths may be prevented by providing the essential neonatal care during delivery and the neonatal period. 13
With a view to reducing the rate of neonatal mortality (NMR) in the world, the United nations submitted the Sustainable Development Goals (SDGs) in 2015, placing maternal and neonatal health problems at the center and setting a NMR of less than 12 deaths per 1,000 life births. 12 However, the NMR in the planet was 15.1 in 2019 (equivalent to 45 % of the total number of deaths in children under five years old) 14 with a significant difference between the developed countries and the medium and low income countries (2 vs. 37 per 1,000 life births). 15 These data show that the neonatal period is the most vulnerable period for the human being, with a risk of dying of almost 15 fold versus any other time during the first year of life. 12
What is the situation of neonatal mortality in Colombia?
According to the Analysis of the Current Health Situation in Colombia (ASIS) 2020, neonatal mortality in the country accounts for 64.7 % of the deaths before one year of life; 50.6 % of the mortality in children under five years old and 61.6 % of child mortality. 16 The NMR in Colombia in 2019 was 6.98 per 1,000 life births, lower than the world average but with large differences among the regions. Hence, while in Bogotá the NMR was 5.74, the Chocó Department for instance reported a NMR of 13.11, with some areas in that region of more than 40 per 1,000 life births (medio Baudó, Rio Iro and Unión Panamericana); something similar happens in La Guajira: 12.9; Vaupés: 14.37; Vichada: 11.11 and Atlántico: 10.41. 17
The typical problems identified in the analysis of perinatal and neonatal deaths conducted by the territorial health agencies in Colombia 18 were: type 1 - 57.2 % associated with quality of care, followed by type 2 - 28.2 % due to failure to recognize the problem; type 3 - 9.7 % poor access to care - referral and counter-referral); type 4 - 4.9 % due to delayed decision-making and action. It may be concluded that types 1 and 2 are associated with the practitioners opinion and judgement during perinatal care and involve the skills developed during medical training and years of professional practice.
Which is the relationship between the Social Determinants of Health and Neonatal Care in Colombia?
The report of the World Bank, entitled "Towards the construction of an equitable society in Colombia" 19 describes the high level of social inequality existing in the country. Some relevant data include:
The GINI index of household income (a standard measure of inequality) was 0.53 in 2019, after it was corrected with the tax burden and distribution of transfers.
The income of the 10 % wealthiest population of Colombians is eleven fold higher than the poorest 10 %.
The level of income and the level of education of parents determine the future levels of income and education of their children, which marks one of the highest rates in the global scale of social inequality from one generation to the next. As Fractal Poverty Traps.
Inequalities are particularly acute among specific population groups, to the detriment of women, people living in rural areas, indigenous groups, Afro-descendants and migrants.
The Human Capital Index in the country is 0.60, which indicates that a neonate in Colombia who reaches his/her 18th birthday, could only be 60 % productive as compared to what he/she could be if access to quality human development was available; i.e., survival, education and health. This index ranges between 0.53 for the poorest quintile of the population (similar to Nigeria, Tanzania, Malawi and Mozambique) and 0.73 for the wealthiest quintile (similar to the high income countries).
In Colombia, the Departments (States) with the highest NMR are those with the highest social inequality. These are also the regions with the lowest capacity and quality of installed healthcare for the population, According to the data of the Colombian Society of Neonatology, there are 187 Neonatal Intensive Care Units in the country, most of them concentrated in Cundinamarca (36), Atlántico (25), Valle (15), Bolívar (13), Antioquia (12) and Córdoba (10); in other words, 59.3% of the NICUs are concentrated in six Departments 20. In contrast, the following Department do not have any NICUs: Amazonas, Casanare, Chocó, Guainía, Guaviare, La Guajira, Putumayo, Vaupés and Vichada. These Departments account for 7.89 % of life births in Colombia (48,137 neonates, of which around 10,000 are premature) (Table 1). Considering that there were 609,739 births in Colombia in 2021, the distribution of NICUs is about one per every 3,260 life births. This means that the nine departments without NICU beds should have at least 15 units installed. This is the result of the decisions guiding the distribution of healthcare services in Colombia, which are governed by economic factors, rather than by the needs of the population.
Table 1 Perinatal results in the Departments without NICU beds in Colombia.
| Department | Life births 2021 | Preterm 2021 (rate per 1,000 life births) | Low birth weight 2021 (rate per 1,000 life births) | Home deliveries2021 (%) | Mortality in babies under 1 2019 (rate per 1,000 life births) | Neonatal mortality 2019 (rate per 1,000 life births) |
|---|---|---|---|---|---|---|
| Chocó | 7,003 | 6.3 | 96.4 | 3.7 | 57.34 | 13.11 |
| Putumayo | 4,716 | 4.5 | 73.2 | 3.3 | 27.34 | 4.58 |
| Amazonas | 1,071 | 5.6 | 64.4 | 16.2 | 38.29 | 8.48 |
| Casanare | 6,153 | 3.1 | 66.5 | 2.4 | 16.80 | 5.24 |
| Guainía | 1,234 | 10.5 | 60 | 13.9 | 49.83 | 5.21 |
| Guaviare | 1,369 | 1.5 | 59.9 | 5.7 | 25.93 | 9.51 |
| Vaupés | 706 | 2.8 | 70.8 | 35.3 | 67.76 | 14.37 |
| Vichada | 1,778 | 12.9 | 52.3 | 26.7 | 59.18 | 11.11 |
| La Guajira | 24,107 | 3.9 | 101.5 | 2.2 | 53.57 | 12.9 |
| Total | 48,137 | |||||
| National average | 1,8 | 98,4 | 1,4 | 17,34 | ,98 |
Source: Author.
In the same World Bank report, these Departments exhibit a high rate of home deliveries, a low number of prenatal controls during pregnancy, and a significant education gap as comparted to other regions in the country; due to the shortage of healthcare practitioners available (the number of doctors and nurses in Chocó, for example, is 1.2 per every 1,000 inhabitants; in Kenya it is 1.69) 19, and also because of the higher proportion of black, Afro-Colombian, Palenqueros and indigenous people which altogether add up to 4.671,160 inhabitants representing 9.34 % of the country's population. 17 There are also differences between rich and poor with regards to the place of prenatal care, since the wealthiest people use private clinics and the centers of the Health Promoting Entities (EPS), while the poorest use the government care centers (Figure 2).
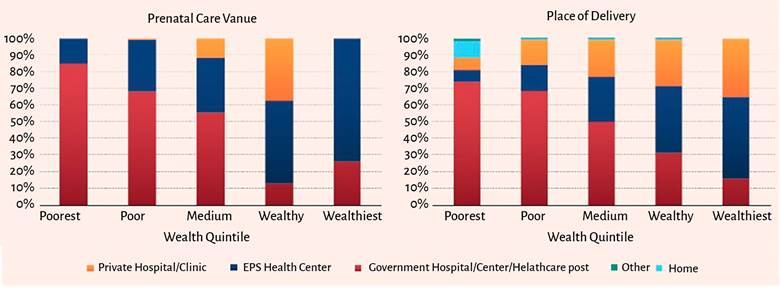
Source: Hacia la construcción de una sociedad equitativa en Colombia 19.
Figure 2 Prenatal care facilities (private or public) in accordance with the level of income.
In Colombia, 2 of every 10 neonates are born before 37 weeks of gestation 21, and prematurity is the main cause of death before 5 years of age. Additionally, neonates are the population group with the highest risk of perioperative complications, which demands technological resources, practitioners with proper training and a network of specialized healthcare services. However, the current unequitable distribution of the healthcare system places newborns at a disadvantage in some regions of the country. This in itself represents a contradiction for the neoliberal development model prevailing in Colombia, especially when considering the potential of productive life years lost, the burden to the healthcare system due to sick leaves from the first days of life, the cost involved in the transfer from remote areas of the country into the capital cities, plus the social cost involved by neonatal disease and death, and in particular, the bioethical implications arising from such much inequality.
The research conducted by Ortiz et al, to assess ethnicity and social exclusion between 2012 and 2017 in Colombia, found that when ethnicity increases by 1%, the level of social exclusion increases by 7% in the country. 22 These "ethnic gaps" account for the large differences in the high NMRs in these areas of the country versus the national average.
A study conducted between 2003 and 2009 which identified variations in child mortality rates (CMR) among the various Departments of Colombia and its relationship with the socioeconomic conditions and the availability of healthcare services 23, found that the impact of insurance, the availability of private beds and medical care, have a stronger impact than the socioeconomic conditions on the CMR. The hypothesis of the authors is that as socioeconomic conditions improve and the CMR decreases, quality medical care becomes increasingly important. Therefore, the healthcare delivery network and the quality of the services provided become critically important, since both condition access to services and programs of the different social groups and become a determinant of the position that individuals reach in the social structure. 5 In this context, quality medical training, technological resources and infrastructure become relevant for neonatal care in the country, as social equity factors.
There are at least 10 healthcare organizations in Colombia exclusively devoted to the pediatric population. Nonetheless, most children in the country receive care in hybrid institutions (caring for all population groups), which results in limitations of infrastructure, technology, inputs, medicines and specialized human resources. Most important yet, the areas of the country with higher neonatal mortality rates and premature births, lack the infrastructure and the specialized human resources to deliver care, and these patients must then be transferred with the inherent risks and social cost involved. However, this gap of resources is not only a fact in the areas described; in the urban areas of Colombia with better resources, there are also obstacles for neonatal care. The decision about where to take care of patients is made based on the business relations among the various institutions, not always privileging the patient's needs, ethnicity, social status, language and cultural barriers not even at the facilities with the best resources to care for the patient's health issues.
These social differences have been studied in other countries. In the United States, black babies are twice as likely to be born premature as compared to white babies 24,25 and exhibit a higher mortality. 26 Such discrepancies in the results are also applicable to Hispanic, American indigenous, and Puerto Rican populations. They also originate from a complex set of factors including racism, and the structural disadvantages of minority families which cannot be accounted for based on biological or genetic differences.
These social barriers generate differences in access to healthcare and quality of services among the various ethnic groups which are reflected in sensitive indicators such as healthcare-associated infection 27 and breast feeding after discharge. 28 Breast feeding is critical since it reduces the incidence of chronic pulmonary disease, necrotizing enterocolitis, blood infections and improved neurodevelopmental results. 29 The long term consequences of these disparities are profound: high risk of morbidity, adverse neurodevelopmental results and behavioral deficits affecting health and quality of life over the years. 30
What is the importance of the role of the anesthesiologist in neonatal care?
Over the last few decades we have witnessed great progress in perinatal medicine. This has increased the number of diagnostic and surgical procedures performed in neonates - frequently premature babies - that require anesthesia. Perioperative mortality in newborns is around 400 per 10,000 (one third occurs during the first 24 hours postop). 31 Hence, neonates and infants represent the group of patients at higher risk of perioperative complications. 32 Critical incidents associated with anesthesia occur in 5 % of anesthetic procedures and are to a large extent associated with the skills and knowledge of the perioperative team about the specific needs of the children. Consequently, there is a need to invest in continuous medical education and to design protocols for common procedures and guidelines for critical situations. 31
An important factor not so widely discussed among the pediatric anesthesia community, is that poor anesthesia decisions, regardless of the type of drug administered, may result in significant neurological morbidity or even mortality in small children. 33. However, these more visible outcomes, are just the "tip of the iceberg" and other more subtle morbidities are unrecognized.
Multicenter studies such as APRICOT 34 and NECTARINE 35, which measured the incidence of anesthetic complications in the pediatric population, reveal the need to set standards for neonatal anesthetic procedures in order to lower the high risk of severe complications. The results of these studies suggest that the outcomes are influenced by post-conception age at the time of surgery, the severity of the underlying disease, and above all, the ability to maintain the normal physiological parameters of the patient, which is directly associated with the experience of the anesthesiologist. 36
What are the difficulties existing in Colombia for the qualification of human resources in pediatric anesthesiology?
While it is difficult to show a direct relationship between the neonatal mortality of a country and the quality of training of human resources in neonatal anesthesiology (for instance, some countries in Europe do not have formal sub-specialization programs in pediatric anesthesiology and have lower mortality rates versus countries that do have such programs), there is indeed a proven relationship between the level of training and perioperative complications in neonatal surgery.
The anesthesiologist, as a fundamental part of the team involved in neonatal care, requires a high level of scientific knowledge, specific skills and abilities, and experience to respond to the perioperative challenges presented by these patients. In accordance with the level of exposure of the anesthesiologist to pediatric anesthesia cases, having a minimum number of cases per year of 200 to 300 children under 10 years old and at least one infant per month per anesthesiologist, is enough to limit the number of complications. 37,38 The occasional practice of pediatric anesthesia (<100 cases per year) represents a five-fold risk as compared to a frequent practice (>200 per year) and severe complications of almost one per every five infants anesthetized. 38
The programs of anesthesiology residencies worldwide include pediatric anesthesia rotations in the curriculum; however, there is no consensus available about the number of cases needed during the training of future anesthesiologists to ensure the minimum skills in neonatal anesthesia. In Argentina, for example, 30 cases are suggested in patients under one year old throughout the complete training program. 39. The Spanish Society of Anesthesia suggests at least 4 to 6 months of training during the education program and a minimum of 6 neonates 40; the Council of Accreditation for Graduate Medical Education (ACGME) recommends 5 cases of children under 3 years old 41 and Washington University requires 15 cases of infants less than one year old 42. Moreover, the Framework Document of the Plan for Studies and Competencies in Anesthesiology in Colombia, of the Colombian Society of Anesthesia Anesthesiology and Resuscitation (S.C.A.R.E.), which involved the participation of universities with anesthesiology specialization programs throughout the country, reported that only 40 % of those programs include in their curriculum subjects on neonatal anesthesia; however, it does not address the number of minimum cases needed to accomplish the necessary the skills. 43. This reality is no different from the anesthesiology training programs in the rest of South America and the Caribbean and offers an opportunity for our country to become a training center for these regions.
Some previous attempts from different universities in Colombia to implement formal sub-specialization program in pediatric anesthesiology have been frustrated because of the reluctance of the Ministry of Health and Social protection to authorize their implementation. It is a contradiction that the care of the surgical newborn is understood by the State as complex in the pediatric and surgical specializations, but this is not the case for perioperative anesthesia care, which is critical for outcomes. This unfortunate reality has forced some anesthesiologists to seek formal training abroad, although that effort may not be recertified when they return to the country. Unfortunately this scarce human resource is concentrated in the capital cities and is not available in many places where care is delivered to surgical neonates in Colombia.
Aware of these difficulties, the Committee of Pediatric Anesthesia of the Colombian Society of Anesthesiology and Resuscitation (S.C.A.R.E.) has made big efforts to highlight the vulnerability of the surgical neonate and to improve the training of anesthesiologists in the country through continuous medical education and constantly participating at congresses, in publications and training courses. 44. However, these efforts are not enough to make skilled human resources available in the remote areas of the country, since the problem is structural. Consequently, a State Policy is needed intended to meet the social demands and consider specialized training of practitioners as a pillar to foster equity in healthcare, so that the surgical neonate shall not be required to be transferred to procure services, but rather that the State provides such services in those regions. This approach places education at the center of the strategy for social transformation Colombia requires and shall ensure better qualification of anesthesiologists interested in this specialty in the country.
CONCLUSIONS
The Social Determinants of Health bring about significant differences in health, life and development opportunities of newborn babies in areas that historically have been neglected in Colombia.
Neonates are the population group with the highest risk of complications and perioperative mortality, and thus demands a high level of training of human resources.
There is consensus in Colombia about the need to implement neonatal anesthesiology as a study subject in the curriculum of the specialization. However, there is a need to overcome the government barriers to develop the subspecialty in pediatric anesthesiology so that more qualified human resources will be make it possible to reduce the inequality of neonatal care in the country.











 texto em
texto em 



