What do we know about the problem?
- OHCA is an important event among the general population and its management requires a different approach to the links in the chain of survival.
- OHCA survival is low and depends on the appropriate functioning of the components in the chain of survival, particularly the activation of the Emergency Medical Services and pre-hospital care for stabilizing and transferring patients to a hospital.
What does the study contribute with?
- The incidence rate of OHCA cases cared for in Medellín, Colombia is low as compared to what is reported in the literature.
- It is necessary to know the local operational characteristics of OHCA care in order to adjust the event records and intervene in the components of the chain of survival.
INTRODUCTION
Every year five million people around the world experience an out-of-hospital cardiac arrest (OHCA); its incidence is 88.8 cases per every 100,000 inhabitants/ year in average, and the survival is below 10 %. 1,2 Less than 40 % of the patients receive help before arrival to the Emergency Medical Services (EMS) and of those who receive care and survive, a significant percentage develop permanent neurological sequalae 3,4.
Witness assistance and the activation of the EMS are essential links in the OHCA chain of survival 5. The EMS is a structured network combining the first responders, call takers, emergency dispatchers, medical and paramedical pre-hospital care personnel (PHCP), and the local network of clinics and hospitals. 1,6 Ambulance operators (AO) are responsible for the delivery of care to patients experiencing an OHCA, their stabilization and further transfer to a hospital facility to continue with resuscitation and care required. 1,5 Medellín has a public AO and several private agencies that together provide care for approximately 2.4 million inhabitants. 6-8
The information about OHCA and the operating characteristics during the response to the event is scarce in our environment. 9 The purpose of this study is to estimate the incidence rate of OHCA in Medellín, Colombia, the response time of AO and to explore any survival-associated factors among this population.
METHODS
Type of study
Population-based retrospective cohort based on the databanks and clinical records of three groups of public and private AO in Medellín, from January 1st, 2018 to December 31st, 2019.
Scenario and study population
The Medical Emergencies System (EMS) is a comprehensive general model intended to articulate the various stakeholders of the General Social Security System to ensure timely response to the victims of the disease, traffic accidents, trauma events or OHCA requiring emergency medical care 6. In Medellín, the EMS operates as a public system and the out-of-hospital care service is operated by one single agent (Metrosalud), which can be accessed over the telephone, dialing "123". Once the case is reported, the operator analyzes it and dispatches the ambulances. The EMS serves the entire population in cases of accidents or medical emergencies within the urban and rural areas that comprise a population of 2,372,330 inhabitants 10.
Among the private AO, there are several home care agencies that provide assistance to individuals and institutions (companies, shopping centers, universities, inter alia) under a previously agreed contract. Their chain of response is activated via their customer service lines for affiliates. They have their own dispatch center and may integrate with the city's EMS. Two of these AO - with the largest coverage and seniority in the system - participated in this study 11,12. Both public and private agencies have ambulances for basic healthcare transportation, medicalized vehicles and immediate response motorcycles. The basic ambulances are manned by prehospital care technologists, and the medicalized ambulances are crewed by prehospital care technicians (PHTs) and physicians.
The whole referral and counter referral process is managed from the Municipal Emergencies Coordination Center (CRUE) which plays the role of dispatcher, allocates the resources for care and directs the patient's pathway along the EMS. 6
All agencies had available the prehospital medical record for the longitudinal registration of the care variables and outcomes; this information was stored in the institutional databases.
Inclusion and exclusion criteria
Patients experiencing OHCA and receiving care by the above-mentioned AO during transfer to a hospital in urban and rural areas of Medellín were included. The information was provided by the Department of Information Management and Analysis of the three groups of AO included in the study.
All the cases of patients receiving care due to an alleged OHCA, sequentially and during the established period of observation were reviewed. The search and screening of medical records was based on the CIE-10 codes of interest: I460, I461, I469, R092, R960, R961 and R98X. Each of the medical records was reviewed to ensure compliance with the inclusion criteria; patients with an explicit DNR or who experienced a cardiac arrest during inter-hospital transfer, were excluded. All of the population available for the study during the observation period was considered.
Collection and classification of information
The information was collected manually and independently by two trained co-investigators, using a data collection instrument designed for this study. The variables of interest collected were sociodemographic, clinical and operational variables of care, and were recorded according to Utstein's guidelines for OHCA 13.
The information was entered into a Microsoft Excel® table and stored in an electronic database for future analysis. Access to this information was exclusively restricted to the groups of investigators in charge of analyzing the information.
Statistical analysis
A descriptive analysis of the data was performed where categorical variables are reported as absolute values and percentages and quantitative variables as means, with their respective standard deviations (SD) or medians, and the corresponding interquartile ranges (IQR), according to the distribution of the data. Frequency histograms were analyzed to determine the distribution of the variables.
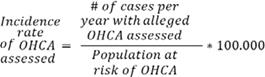
The incidence rates for OHCA were standardized for the general population of Medellín over that time period 2. The following formulas are based on the 2022 statistical report of heart diseases and cerebrovascular accidents of the American Heart Association (AHA) 2, the Cardiac Arrest Registry for Enhanced Survival (CARES) 14, and the study of regional variation of the incidence of OHCA 15.
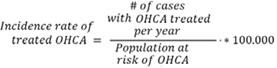
Timely delivery of care by the EMS was defined as the total sum of the time intervals in minutes, between the time when the ambulance was activated by the dispatcher (t0) and the arrival time of the ambulance on site for delivery of care to the OHCA patient (t1), divided by the number of patients who received care by the EMS over that period:
Timely care was classified for analysis into 5 groups: <4 minutes, 4-7 minutes, 8-14 minutes, 15-29 minutes and ≥30 minutes 16.
The groups of patients treated by the AO, as well as those assessed by these AO were studied 2,16.
To establish any potential OHCA survival-associated factors a raw bivariate analysis was conducted, with no changes based on confounders; the results are expressed as Odds Ratio (OR) with the corresponding 95 % CI. The variables included in this comparison were selected based on clinical relevance. Additionally, differences in timeliness of care between the patients who survived and those who died were investigated, using the Wilcoxon test for unpaired samples.
All of the analyses were performed with a level of significance of 0.05. The statistical analyses were made using software R (version 4.1.0, R Foundation for Statistical Computing, Vienna, Austria) and R Studio (version 1.4.1717, R Studio Inc. Boston, USA).
RESULTS
Sociodemographic and care characteristics - OHCA Incidence rate
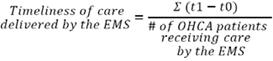
A total of 2,312 medical records of patients experiencing a probable OHCA, who received care by the AO in Medellin were reviewed. 865 cases were excluded, mostly because they were outside the city area. Other exclusion criteria are listed in the flowchart of events (Figure 1). In the end, 1,447 cases that met the inclusion criteria were reviewed and analyzed; OHCA events receiving care by the PHCP of the AO in Medellín.
CA: cardiac arrest; DNR: Do-not-resuscitate; MR: medical record. Source:Authors.
Figure 1 Flowchart of events analyzed.
58.5 % (n = 846) of the patients with OHCA were females; the mean age was 84 years (IQR 16); 94.5 % (n =1,367) had at least one underlying pathology. 96.5 % (n =1,396) of OHCA occurred at home, 2.8 % (n = 40) in public areas, and 54-8 % (n = 793) were not witnessed. In 10.0 % (n =145) of the cases, the rhythm of the detected arrest was not amenable to defibrillation and 1.9 % (n = 28) were; no report was submitted for the rest of the cases.
Of all the population receiving assistance, 11.8 % (n = 171) underwent some type of cardiopulmonary resuscitation (CPR); of these, 18.13 % (n = 31) received CPR only by a layperson and 81.8 % (n = 140) were treated by PHCP from the AO. Of this latter group, 65.0 % (n = 91) received CPR by PHCP only and 35.0 % (n = 49) by both, laypersons and PHCP. Of the group of patients treated by PHCR the mean age was 75 years old (IQR 22.8) and 52.5 % (n = 73) were males. In 90.7 % (n =137) of the cases, the OHCA was witnessed; 57-9 % (n = 81) received adrenaline treatment, 34-3 % (n = 48) IV fluids and assisted ventilation was provided with a bag-valve-mask device in 64.3 % (n = 90) and with orotracheal intubation in 7.9 % (n = 11). 20.7 % (n = 29) underwent defibrillation. Table 1 shows the baseline characteristics of the population studied.
Table 1 Baseline characteristics of the population with OHCA receiving care by PHCP in Medellín, Colombia, between 2018 and 2019.
| Variable | Evaluated (n = 1.307) | Treated (n = 140) | Total (n = 1.447) | |
|---|---|---|---|---|
| Age, median (IQR) | 85 (15) | 75 (22.8) | 84 (16) | |
| Female gender, n (%) | 780 (59.7 %) | 66 (47.5 %) | 846 (58.5 %) | |
| Underlying conditions,% (n) | ||||
| IHD | 154 (11.8 %) | 9 (4.2 %) | 163 (11.3 %) | |
| CVA | 221 (17.0 %) | 9 (4.2 %) | 230 (16.0 %) | |
| CAOD | 18 (1.4 %) | 0 (0.0 %) | 18 (1.3 %) | |
| Smoking | 203 (15.6 %) | 14 (10.0 %) | 217 (14.9 %) | |
| Diabetes mellitus | 329 (25.2 %) | 31 (22.1 %) | 360 (24.8 %) | |
| HBP | 829 (63.6 %) | 71 (50.7 %) | 900 (62.1 %) | |
| Arrythmia | 188 (14.4 %) | 5 (3.5 %) | 193 (13.3 %) | |
| Sudden death | 1 (0.01 %) | 0 (0.0 %) | 1 (0.06 %) | |
| COPD | 336 (25.8 %) | 19 (13.5 %) | 355 (24.5 %) | |
| CHF | 242 (18.6 %) | 14 (10.0 %) | 256 (17.6 %) | |
| Level of education, % (n) | ||||
| Illiterate | 9 (0.07 %) | 0 (0.0 %) | 9 (0.6 %) | |
| Primary | 137 (10.5 %) | 4 (2.8 %) | 141 (9.7 %) | |
| Secondary | 89 (6.8 %) | 2 (1.4 %) | 91 (6.2 %) | |
| Technical | 26 (2.0 %) | 1 (0.7 %) | 27 (1.9 %) | |
| Professional | 46 (3.5 %) | 4 (2.8 %) | 50 (3.4 %) | |
| No information | 1.000 (76.5 %) | 129 (92.1 %) | 1.129 (78.0 %) | |
| Health insurance regime, % (n) | ||||
| Subsidized | 25 (0.2 %) | 15 (10.7 %) | 40 (2.8 %) | |
| Contributory | 1.120 (85.6 %) | 105 (75.0 %) | 1.225 (84.7 %) | |
| Noninsured | 5 (0.3 %) | 0 (0.0 %) | 160 (11.1 %) | |
| No information | 144 (11.0 %) | 15 (10.7 %) | 9 (0.6 %) | |
| Special | 13 (0.9 %) | 0 (0.0 %) | 13 ( 0.9 %) | |
| Site of occurrence, % (n) | ||||
| Public area | 10 (0.8 %) | 30 (21.4 %) | 40 (2.7 %) | |
| Home | 1.291 (98.8 %) | 105 (75.0 %) | 1.396 (96.4 %) | |
| Ambulance | 2 (0.2 %) | 2 (1.4 %) | 4 (0.2 %) | |
| Other | 4 (0.3 %) | 3 (2.1 %) | 7 (0.4 %) | |
| Initial rhythm of arrest, % (n) | ||||
| Non amenable to defibrillation | 51 (3.9 %) | 94 (67.1 %) | 145 (10.0 %) | |
| Amenable to defibrillation | 3 (0.2 %) | 25 (17.9 %) | 28 (1.9 %) | |
| Non identified | 1.253 (95.9 %) | 21 (15.0 %) | 1.274 (88.0 %) | |
| CPR attending personnel, % (n) | ||||
| Layperson | 31 (2.4 %) | (0 %) | 31 (2.1 %) | |
| PHCP | - | 91 (65.0 %) | 91 (6.2 %) | |
| Layperson and PHCP | - | 49 (35.0 %) | 49 (3.3 %) | |
| No CPR | 1.276 (97.6 %) | 0 (0 %) | 1276 (88.1 %) | |
| Assisted ventilation % (n) | ||||
| BVM | - | 90 (64.3 %) | 90 (6.2 %) | |
| OTI | - | 11 (7.9 %) | 11 (0.7 %) | |
| Face mask | - | 5 (3.6 %) | 5 (0.3 %) | |
| No information | 1.307 (100 %) | 34 (24.3 %) | 1.341 (92.6 %) | |
| Defibrillation | ||||
| 4 (0.3 %) | 29 (20.7 %) | 33 (2.3 %) | ||
| Adrenaline | ||||
| Yes | - | 81 (57.9 %) | 81 (5.5 %) | |
| No | 1304 (99.8 %) | 44 (31.4 %) | 1.348 (93.1 %) | |
| No information | 3 (0.2 %) | 15 (10.7 %) | 18 (1.2 %) | |
| Antiarrhythmic agents | ||||
| Yes | - | 14 (10.0 %) | 14 (0.9 %) | |
| No | 1,306 (99.9 %) | 115 (82.1 %) | 1,421 (98.2 %) | |
| No information | 1 (0.1 %) | 11 (7.9 %) | 12 (0.8 %) | |
| Intravenous fluids | ||||
| Yes | 2 (0.2 %) | 48 (34.3 %) | 50 (3.4 %) | |
| No | 1,305 (99.8 %) | 81 (57.9 %) | 1,386 (95.7 %) | |
| No information | - | 11 (7.9 %) | 11 (0.8 %) | |
| Cause of the arrest | ||||
| General disease | 1,289 (98.6 %) | 134 (95.7 %) | 1,423 (98.3 %) | |
| Other | 15 (1.1 %) | 5 (3.5 %) | 20 (1.3 %) | |
| No information | 3 (0.2 %) | 1 (0.7 %) | 4 (0.2 %) | |
| ROSC | ||||
| - | 24 (17.1 %) | 33 (2.2 %) | ||
| Final vital status | ||||
| Alive | 9 (0.6 %) | 21 (15.0 %) | 30 (2.0 %) | |
| Interval in minutes alert and arrival PHCP | ||||
| 27 (60) | 13 (12.3) | 26 (55.2) | ||
The quantitative variables are reported as medians and IQR.
BVM: bag-valve-mask; CAOD: chronic arterial occlusive disease; CHF: congestive heart failure; COPD: chronic obstructive pulmonary disease; CPR: cardiopulmonary resuscitation; CVA: Cerebrovascular accident; HBP: high blood pressure; IHD: Ischemic heart disease; OTI: orotracheal intubation; PHCP: pre-hospital care personnel; ROSC: return of spontaneous circulation.
Source: Authors.
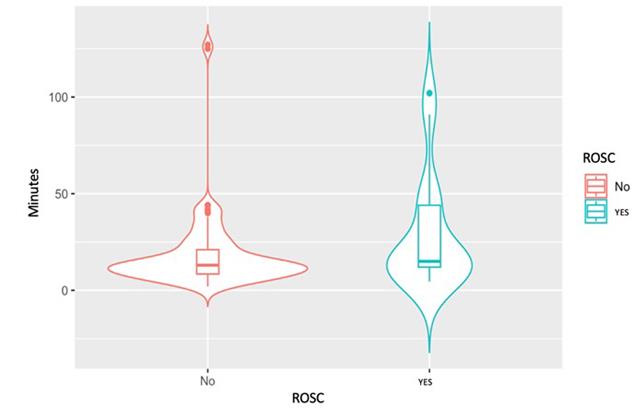
The response time from activation to delivery of care by the PHCP of the AO in the cases assessed was a median of 27 minutes (IQR 60) and in the group of treated patients was 13 minutes (IQR 12.3) (Figure 2). In this latter group, 25.7 % (n = 36) of the cases failed to record the arrival time and hence it was impossible to estimate the response time. The distribution of response times between dispatch of the PHCP and on-site arrival is shown in Table 2.
Source: Authors.
Figure 2 Time in minutes between the response from the moment of activation until PHCP care in cases of treated OHCA presenting with ROSC.
Table 2 Time interval between dispatch of PHCP and on-site arrival for assistance.
| T_Min_groups | Assessed n = 1.275 (%) | Treated n = 104 (%) | Total n = 1.379 ( %) |
|---|---|---|---|
| <4 | 9 (0.7) | 3 (2.9) | 12 (0.9) |
| 4-7 | 44 (3.5) | 12 (11.5) | 56 (4.1) |
| 8-14 | 306 (24.0) | 44 (42.3) | 350 (25.4) |
| 15-29 | 295 (23.1) | 27 (26.0) | 322 (23.4) |
| ≥ 30 | 621 (48.7) | 18 (17.3) | 639 (46.3) |
T_Min_groups: Time interval in minutes for each group. The time interval between the PHCP dispatch and on-site arrival was not available in 68 cases; 36 of them correspond to treated patients and 32 to patients assessed.
Source: Authors.
Out of the total number of cases in which CPR was attempted, 19.3 %(n = 33) experienced return of spontaneous circulation (ROSC) at some point during the CPR procedure. The survival in the group of treated patients at arrival to the hospital was 14.2 % (95 % CI 5.5-22.8) and 15.5 % (95 % CI 7.4-23.5) for 2018 and 2019, respectively; the mortality of the patients assessed was 99.9 %.
The incidence rate of OHCA assessed by an AO was 28.1 (95 % CI 26.0-30.3) and 26.9 (95 % CI 24.9-29.1) cases per 100,000 inhabitants/year, for 2018 and 2019, respectively; the incidence rate of treated OHCA was 2.6 (95 % CI 2.0-3.3) and 3.2 (95 % CI 2.5-4.0) per 100,000 inhabitants/year, for 2018 and 2019.
OHCA survival-associated factors
A bivariate analysis found that defibrillation during CPR is associated with survival (OR 3.71; 95 % CI 1.35-9.99), whilst the identification of an initial rhythm not amenable to defibrillation is associated with non-survival (OR 0.16; 95 % CI 0.050.46). The administration of adrenaline, the use of anti-arrhythmic agents, assisted ventilation, CPR by laypersons, and response time between AO dispatch and on site arrival to the OHCA event for assistance, were not associated with survival in this population (Table 3). However, given the number of patients treated and the number of outcomes registered, the regression was not modelled due to potential confounding variables.
Table 3 Exploration of survival-associated factors in OHCA in PHCP treated patients.
| Variable | Odds Ratio | IC 95 % | |
|---|---|---|---|
| Lower limit | Upper limit | ||
| CPR before PHCP | 1.79 | 0.69 | 4.61 |
| Defibrillation | 3.71 | 1.35 | 9.99 |
| Adrenaline | 0.67 | 0.20 | 1.92 |
| Antiarrhythmic agents | 2.10 | 0.37 | 39.4 |
| Assisted ventilation | 4.10 | 0.95 | 16.08 |
| Initial rhythm non amenable to defibrillation | 0.16 | 0.05 | 0.49 |
| Interval between alert and PSCP arrival | 1.90 | 0.93 | 3.99 |
These Odds Ratio are raw.
CPR: cardiopulmonary resuscitation; PHCP: pre-hospital care personnel.
Source: Authors.
DISCUSSION
This study shows the operating and clinical characteristics of an OHCA receiving care from an AO in Medellín, Colombia. The primary finding was that the incidence rates of the OHCA assessed and treated by PHCP are lower when compared against those reported in the literature. In a systematic review published in 2010, which included 67 studies, Berdowski et al. reported rates between 83.7-95.9 and 34.7-62.3 per 100,000 people/year, of cases assessed and treated by the EMS, respectively. This rates only included studies from Europe, North America, Asia, and Australia; African and Latin American trials were not included 4. Some trials such as Nichol et al., report variable rates of cases assisted by the EMS, ranging from 70 to 153 cases per every 100,000 inhabitants/year in several cities in Canada and the United States, during 2006 and 2008 15. Another more recent study by Lim et al., in Singapore and Victoria (Australia) between 2011 and 2016, showed and incidence of OHCA among people over 20 years old of 90 cases per 100,000 inhabitants/year 17. This finding is comparable to that previously mentioned, but in healthcare systems similar to ours.
This shows that the incidence of OHCA identified in this study is far below the average reported in other regions worldwide. While these variations may be associated with differences in the health systems and the provision of pre-hospital service due to the regional context, it should be highlighted that in high income countries health systems, the arrival of seriously ill patients to the emergency department - including OHCA - accounts for 42-93 % via the EMS and AO 15,18,19; in contrast, a study conducted in Bogotá, Colombia, by Bustos et al., reported a 20% involvement of AO with patients arriving to the emergency room. However, this percentage fails to discriminate the type and severity of patients (20). As already mentioned, care of these events in Medellín is based on a hybrid system with the participation of AO from the public EMS and private agencies. This study showed that the largest proportion of the treated events were addressed by private AO. Patients experiencing a cardiac arrest who were transferred directly by members of the community or by other means to the hospital center - which until now are not reported in the literature or other sources of information - may impact our estimates.
In the current study, the survival at arrival to the hospital was 15 %, a number below that reported by Tsao et al., who in their report about heart diseases and stroke show a survival for OHCA of 25.6% at arrival to the hospital 2. The findings in this study are clearly poorer as compared to other studies and this may be due to the impact of the response times after the cardiac arrest by the PHCP and to the low frequency of help from witnesses prior to the arrival of the AO. Some research studies report CPR assistance by witnesses of up to 72 % of the cases in some regions in the United States, which represents a significant two-fold or higher impact on the activation of the chain of survival versus non-participation of witnesses, improved participation of the various EMS components and increased survival of the OHCA population when arriving to the hospital of up to 48 % when there is active involvement of bystanders or witnesses in vital support maneuvers 2,4,16. The lack of involvement of witnesses and the community in assisting a cardiac arrest decreases the likelihood of having the desired impact of the activation of the chain of survival; hence, it is critical to develop well-structured programs for training of first-responders and to update the healthcare personnel on effective OHCA care interventions, with a view to improving compliance with the international resuscitation guidelines resulting in enhanced quality indicators in this population.
Another factor to be emphasized is that in the group of treated patients, most of the cardiac arrest events developed at home or residences (75 %), while one fifth (21.4 %) developed in public areas. The report by Tsao et al. shows similar findings, evidencing that 73.9% of this type of events in the United States develop at home and 21 % in public areas 2. The study by Park et al., reported that 22 % of OHCA occurred in public areas, and in the study by Ong et al., conducted in Asian countries, 13.3% of the events occurred in this setting 16,21. Therefore, preparedness and assistance should focus on the management of cardiac arrest in these settings, keeping in mind the differences between the identification of the arrest on site, stabilization, and transportation of the patient to the hospital.
General disease represented 98.3 % of the population assessed, in contrast to the study by Navarro Vargas et al., conducted in Bogotá, which reported that 64.0 % of OHCA were secondary to medical conditions and 22.0 % were trauma related 9. A large proportion of the population in this study is elderly; a similar finding reported in other studies, where the mean age ranged between 69.9 - 71.2 years 16,21. These findings may in part be due to the fact that most of the sample was collected from private AO, in which elderly patients account for a large proportion of the affiliations to these agencies; however, this evidences that the event is more frequent among the elderly and this is no exception in our setting.
This observational research - according to a non-adjusted analysis - evidenced that defibrillation during OHCA increases the probability of survival by over three-fold, and consistent with this finding, the identification of a rhythm non-amenable to defibrillation reduces the probability of surviving the OHCA by more than 50 %. These factors have been described in the literature with the same impact; for example, Lim et al., found that the use of a defibrillator during CPR in a public venue may increase the probability of survival by more than two-fold; similarly, other factors such as identifying a rhythm amenable to defibrillation, an OHCA witnessed and assisted by bystanders and the arrival time of the PHCP of the EMS may all improve the survival of this population 17. It should be highlighted that the purpose of this work was exploratory and further studies are needed, including additional details about these associations and their nature.
Resuscitation performed by lay personnel prior to EMS arrival was low, with the aggravating factor that the initial arrest rate was not determined in most of the sample. This suggests a lack of preparedness of the general population in the care of OHCA and in activating the chain of survival, which may directly impact the likelihood of survival and reduce neurological sequelae. This has already been demonstrated in several studies which have shown that the presence of a rhythm amenable to defibrillation during OHCA is associated with twice the probability of survival (OR 2.1; 95% CI 1.68-2.63), even more so if the patient is resuscitated by lay personnel 3,22. It should be noted however that in the analysis of the current study only a raw analysis was conducted, given the frequency of occurrence of the outcome 23; this fact should be taken into account for the interpretation of the findings.
The median time between activation and EMS arrival was 13 minutes. It is important to work on decreasing the response time of the AO for OHCA assistance, given that the condition under study is time-dependent; that is, the more timely the assistance and specific interventions, the higher the probability of ROSC and hence of improved survival, since after this time range the metabolic changes become incompatible with life 13,17,24,25.
Based on the specific interventions for treating OHCA, a lack of compliance with the different resuscitation guidelines was observed 3,26,27; for instance, in 24% of the treated population no information was entered with regards to assisted ventilation and only 57.0 % received adrenaline treatment. Studies such as the one by Perkins et al., show higher probabilities of 30-day survival with the use of adrenaline versus placebo (OR 1.39; 95 % CI 1.06-1.82), although there was no improvement in neurological outcomes (OR 1.18; 95 % CI 0.86-1.61) 28.
Finally, since there are no guidelines for reporting OHCA cases at the national level the records and the quality thereof have to be optimized in the medical record, based on the recommendations of the International Liaison Committee on Resuscitation (ILCOR), better known as the Utstein guidelines, issued in 1991 for recording OHCA 13,26. The EMS agents responsible for cardiac arrest care must strive to disseminate and increase the use of these tools, which will help to improve the quality of the data recorded and the information for preparedness and deployment of the teams that will provide care in these cases.
In terms of limitations, the authors of this study found that the coding and storage of the medical records of the CA analyzed differ among the various AO. While the search of codes CIE-10 selected allowed for patient identification for later analyses, there may be some cases registered under the underlying condition and disease that presumably caused the CA, but not as a OHCA as such; this may have limited capturing all patients searched. Furthermore, in this study the survival at hospital discharge was not evaluated, neither the neurological condition of survivors, which are hard outcomes in this population. The scattered records based on the place of occurrence of the event (in-hospital or pre-hospital) and the attending AO, hinder follow-up and prevent the consolidation of the information. Actions should be encouraged to streamline the information through population records similar to those previously discussed, since this could be an option to mitigate such limitation in the future 14,17. Finally, the interpretation of the factors associated with this study should be considered exploratory.
The strength of this study is first and foremost that this is the first to be conducted in the city. Furthermore, the study analyzes the total OHCA population served by the public EMS and two of the largest and most senior private AO in the city; hence, the trial may be considered an actual reflection of the condition and the care delivered.
All of these is an indication that the OHCA care programs in the city where the study was developed, should be reviewed in terms of its implementation components, particularly the activation and community involvement phases. 5,16 A scenario should be considered in which public and private agencies together join operational, tactical and strategic efforts to improve preparedness and organization in the provision of prehospital care by PHCP for OHCA, which could have an impact on health indicators.
ETHICAL RESPONSIBILITIES
Ethical considerations
The study was approved by the ethics committee of Medical Researchs Institute of Universidad de Antioquia in Medellín, Colombia, as provided under minutes 024 of December 5, 2019 and endorsed by the Technical Committee of the three participating institutions.
Protection of humans and animals
The authors declare that no experiments have been made in humans or in animals for the purposes of this research project.
Confidentiality of the data
The authors declare that they have followed all of their institutional protocols about the publication of patient data.
Right to privacy and informed consent
The authors declare that this article does not mention any patient data. This study did not use an informed consent since it was considered risk free research, according to the scientific, technical, and administrative standards for health research in the local setting.
ACKNOWLEDGEMENTS
Contribution by the authors
SAMH and DEGB participated in the planning, data collection and data management, including quality control, data analysis, manuscript review, and significantly contributed to the drafting process.
JCVV participated supervising the observational research, analyzed the data and significantly contributed to the review of the manuscript.
PAEV participated in the data analysis and significantly contributed to the review of the manuscript.
CEVB participated in the conceptualization of the idea, supervision of the observational research, data collection and management, including quality control; analyzed the data, participated in the drafting of the manuscript, and significantly contributed to its review.











 texto em
texto em