Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Acessos
Acessos
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares em
SciELO
Similares em
SciELO -
 Similares em Google
Similares em Google
Compartilhar
Revista colombiana de Gastroenterología
versão impressa ISSN 0120-9957
Rev Col Gastroenterol vol.34 no.4 Bogotá out./dez. 2019
https://doi.org/10.22516/25007440.289
Case report
Endoscopic diagnosis of Uncinariasis, presentation of a case with severe iron deficiency anemia
1Residente de Medicina Interna, Universidad Pontificia Bolivariana, Medellín, Colombia.
2Unidad de Gastroenterología y Endoscopia Digestiva. Hospital Pablo Tobón Uribe, Medellín, Colombia.
We present the clinical case of a young man from a rural area who required transfusion of blood products due to severe iron deficiency anemia although there was no obvious bleeding. Multiple tests ruled out hemolytic, autoimmune causes and chronic disease as the cause of his anemia. Endoscopy found massive ancylostomiasis, a potentially curable cause of anemia in our environment. In this article we describe the clinical case, discuss differential diagnoses of iron deficiency anemia, and review the literature.
Keywords: Anemia; ancylostomiasis; parasitic diseases; endoscopy; differential diagnosis
Presentamos el caso clínico de un joven, proveniente del área rural, con anemia ferropénica severa, sin sangrado evidente, quien requirió transfusión de hemoderivados y múltiples exámenes, donde se descartaron causas hemolíticas, autoinmunes y anemia de enfermedad crónica. En estudios endoscópicos se le documentó uncinariasis masiva como causa de su cuadro clínico. La uncinariasis es una causa sub-diagnosticada y potencialmente curable de anemia en nuestro medio. En este artículo hacemos la descripción de un caso clínico, la discusión sobre diagnósticos diferenciales de anemia ferropénica y revisión de la literatura.
Palabras clave: Anemia; infecciones por uncinarias; enfermedades parasitarias; endoscopia; diagnóstico diferencial
Introduction
Hookworm infections (also known as ancylostomiasis or hookworm infections) are caused by Necator americanus or Ancylostoma duodenale nematodes. They are transmitted by direct contact with soils containing these parasites. In humans, they primarily manifest in the digestive tract, and their most frequently found symptoms are chronic blood losses, secondary iron deficiency anemia and protein-losing enteropathy with secondary hypoalbuminemia.
Although hookworm infections are common in Colombia, they are usually underdiagnosed or underestimated in cases of severe anemia. 1,2 Hookworm infections are endemic especially where physical and sociocultural environment favors fecal-oral contamination. Preschool and school children are most susceptible to infection, but the disease also occurs in adults. 2,3 Several studies published in Latin America and Africa have confirmed the causal relationships of hookworm infections with poverty, poor environmental sanitation, and residence in rural areas. 4,5,6 Diagnosis is usually made by identifying the parasite or its eggs in fecal matter.
Clinical case
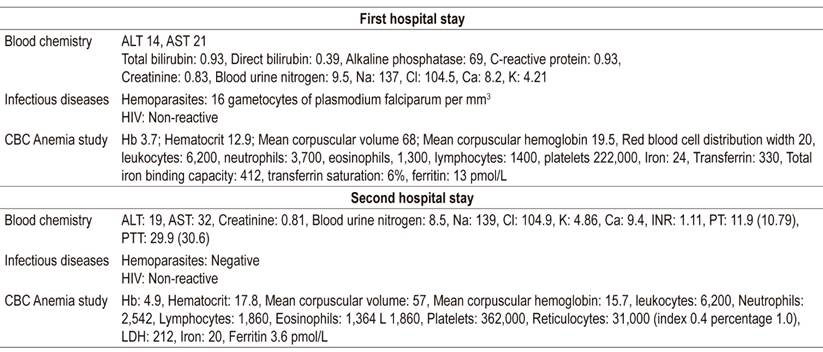
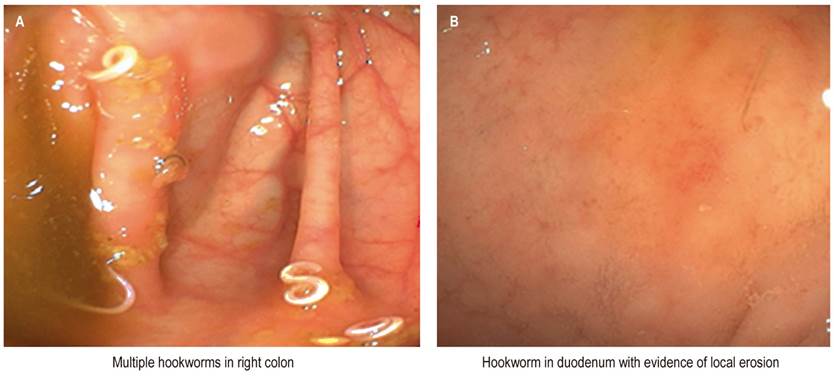
A 20-year-old farmer from a reservation of indigenous people in Cauca was evaluated at the municipal health center in February 2017. He had been suffering unquantified intermittent fevers, feelings of weakness, fatigue and diaphoresis. On physical examination, his overall physical condition was found to be poor. He had marked cutaneous and mucosal paleness and a fever of 38.5° C. Blood tests showed severe anemia with a hemoglobin (Hb) count of 3.6 g/dL. A thick smear was positive for malaria (P. falciparum with 1520 asexual forms). Treatment was initiated with 4 tablets of Coartem® (20 mg of artemether and 120 mg of lumefantrine) every 12 hours for 6 doses in total. He was referred to our medical center, where additional blood tests of ferrokinetics, hemolysis and other infections were performed (Table 1). In addition, the thick smear was repeated and found a significant decrease of parasitemia. He was treated for anemia with 3 units of packed red blood cells and antimalarial treatment continued. His fever disappeared and his Hb count increased to 7.8 g/dL, so he was discharged.
The was readmitted on October 5, 2017 due to marked asthenia, adynamia, fatigue, itching and pulsatile headache. He said he had not suffered any manifest gastrointestinal bleeding or jaundice. At admission, he required a blood transfusion due to severe anemia (hemoglobin: 4.9 g/dL). Upper digestive endoscopy found evidence of inflammatory changes and erosion in the duodenum where moving parasites were identified (Figure 1A). Colonoscopy identified at least 15 elongated whitish worms that were moving within the right colon and cecum (Figure 1B). Daily oral doses of iron salts for 6 months plus treatment with 10 mg/kg of pyrantel pamoate for 3 days every 6 months for 3 years was recommended for the patient and his close relatives. In addition, he was offered health education on basic hygiene. In telephone follow-up calls at 6 and 9 months, he reported complete improvement of his symptoms.
Discussion
Iron deficiency anemia, the world’s most common nutritional disorder, is a global public health problem. It affects more than 2 billion people with approximate prevalences of 40% in preschool children, 30% in women of childbearing age and up to 38% in pregnant women. 7 It is responsible for almost half of all cases of anemia in low and middle income countries. 8 In developing countries it usually results from poor nutrition or gastrointestinal blood loss due to intestinal parasites. 7
The symptoms of anemia vary greatly and are nonspecific. Classic symptoms include fatigue, dyspnea related to exercise, itching, headache and impaired concentration (which can manifest as the result of iron deficiency without associated anemia). Some obvious signs are cutaneous and mucosa paleness, tachycardia and orthostatic hypotension. Other less frequent, and perhaps more subtle, symptoms include glossitis, angular stomatitis and koilonychias. 9
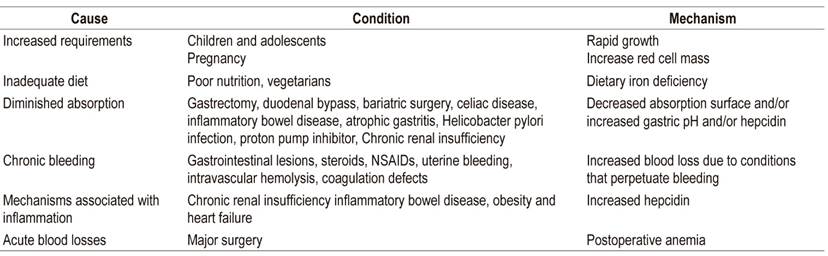
There is a broad spectrum of possible causes of iron deficiency anemia (Table 2), not least of which is gastrointestinal bleeding (manifest or occult). 10 Parasitosis should be considered in the initial diagnosis of patients with iron deficiency anemia due to digestive losses. Late diagnosis can generate use of unnecessary diagnostic aids and expose patients to risks of possible complications such as neurodevelopmental delay, heart failure, miscarriages, and morbidity in pregnant women. 2,7
The most serious cases of anemia produced by parasites are observed in hookworm infections, malaria, trichuriasis and diphyllobothriasis. Parasitosis can cause anemia secondary to chronic malnutrition through various pathophysiological mechanisms. These include malabsorption and anorexia resulting from inadequate diet; hemolytic anemia, as in cases of malaria and babesiosis; and gastrointestinal bleeding due to lesions in the gastrointestinal mucosa such as those that occur in infections by protozoans such as Entamoeba histolytica, Balantidium coli or infections by helminths such as Ancylostoma duodenale, Necator americanus, Strongyloides stercoralis and Trichuris trichiura. 10
The etiology of anemia in this case was initially attributed to more than one factor since the initial diagnosis was P. falciparum malaria. However, hemolysis markers were not documented nor did the patient’s hemoglobin levels improve noticeably successful completion of treatment with artemether/lumefantrine (Coartem®). In addition, eosinophilia is rare in cases of malaria.
Hookworm infection is a parasitic disease caused by Necator americanus or Ancylostoma duodenale, two species of blood-borne nematodes of the Ancylostomatidae family. These infections cause digestive disorders and hypochromic microcytic anemia which is more intense in massive infections. Infection in humans is caused by penetration of the skin by filariform larvae which are found in contaminated soils. In early stages of maturation, they are called rhabditiform larvae. In the migration phase, the larvae reach the lungs and penetrate the alveolar sacs. The intestinal phase begins with swallowing which results in erosions or ulceration of the gastrointestinal mucosa. The correlation between clinical severity and the intensity of parasitism varies according to nutritional status and any preexisting anemia in these patients. 2
Clinically, hookworm infections are considered to be mild when the fecal egg count is below 2,000 eggs per gram. Moderate infections have 2,000 to 4000 eggs per gram, and severe infections have counts greater than 4,000 eggs per gram. 2 For necator americanus, the approximate number of adult worms is obtained by dividing the number of eggs per gram of fecal matter by 80. Cases of severe infestation are estimated to have 50 adult parasites in the intestine. It has been shown that Necator americanus generates a daily blood loss of at least 0.04 mL per parasite while for Ancylostoma duodenale daily blood loss is estimated to be 0.20 mL per parasite. Transient bleeding results when a worm detaches itself from the mucosa to move to another site. After a few months of infection, the result is microcytic and hypochromic iron deficiency anemia. 2 Other manifestations include pruritic dermatitis and nonspecific neurological and pulmonary symptoms such as pulsatile headache and drowsiness. In cases of early childhood infections, retardation of growth and neurodevelopment may occur. 2
A diagnosis is confirmed when worm eggs are found in feces or when adult parasites are seen. Useful methods include direct examination, the Willis-Faust concentration method, and the quantitative techniques of Stoll and Kato-Katz which indicate the number of eggs per gram of feces. 10 Fecal culture by the Harada-Mori method allows differentiation between Ancylostoma duodenale and Necator americanus species according to the morphologies of their filariform larvae. 10
In the case presented, the diagnosis was made from the sum of clinical, laboratory and endoscopic data. Although the endoscopic studies in this case played an important role in the diagnosis, we believe that expensive and invasive examinations can be avoided with a more rational approach.
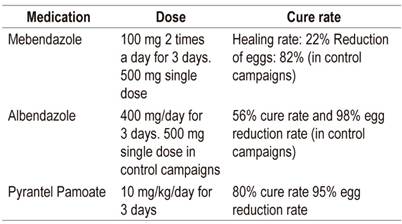
Treatment consists of administration of anthelmintics, especially benzimidazole and pyrantel pamoate, plus treatment of anemia. In Colombia, the most commonly recommended and most frequently used anthelmintics are mebendazole, albendazole and pyrantel pamoate. Their cure rates vary (Table 3). 1,2 The authors’ preference is pyrantel pamoate because it inhibits the cholinesterase enzyme and causes depolarization of the muscle plaque. This causes spastic paralysis of the nematodes which has a beneficial effect on massive parasitosis by minimizing the risk of larval migrations. 2. These schemes are inexpensive and have few adverse effects, so they can be administered whenever there is suspicion of a hookworm infection even in patients without a confirmed diagnosis who live in areas of high prevalence.
REFERENCES
1. Mosquera G, Correa NF, Concha A. Sangrado oscuro y anemia crónica severa: discusión sobre dos causas gastrointestinales subvaloradas en Colombia. Univ Med. 2014;55(2):229-34. [ Links ]
2. Botero D, Restrepo M. Uncinariasis. En: Botero D, Restrepo M (editores). Parasitosis humanas. 3ª edición. Medellín, Colombia: Corporación para Investigaciones Biológicas. 2012. p. 145-60. [ Links ]
3. Carrada-Bravo T. Uncinariasis: ciclo vital, cuadros clínicos, patofisiología y modelos animales. Rev Mex Patol Clin. 2007;54(4):187-99. [ Links ]
4. Udoski JK. Necator americanus infection: a cross-sectorial study of a rural community in relation to some clinical symptoms. Ann Trop Med Parasitol. 1980;78:443-4. doi: https://doi.org/10.1080/00034983.1984.11811845. [ Links ]
5. Hernández-Lira J. Distribución geográfica y patología de la uncinariasis en la República Mexicana. Rev Mex Patol Clin. 1949;13:111-5. [ Links ]
6. Bradley M, Chandiwana SK, Bundy DAP. The epidemiology and control of hookworm infection in the Burma Valley area in Zimbabwe. Trans R Soc Trop Med Hyg. 1993;87:145-7. doi: https://doi.org/10.1016/0035-9203(93)90463-Z. [ Links ]
7. Camaschella C. Iron deficiency anemia. N Engl J Med. 2015;372:1832-43. doi: https://doi.org/10.1056/NEJMra1401038. [ Links ]
8. Pasricha SR, Drakesmith H, Black J, Hipgrave D, Biggs BA. Control of iron deficiency anemia in low- and middle-income countries. Blood. 2013;121(14):2607-17. doi: https://doi.org/10.1182/blood-2012-09-453522. [ Links ]
9. Clark SF. Iron deficiency anemia. Nutr Clin Pract. 2008;23(2):128-41. doi: https://doi.org/10.1177/ 0884533608314536. [ Links ]
10. Camaschella C. New insights into iron deficiency and iron deficiency anemia. Blood. 2017;31(4):225-33. doi: https://doi.org/10.1016/j.blre.2017.02.004. [ Links ]
Received: August 26, 2018; Accepted: October 02, 2018











 texto em
texto em