Introduction
Cardiovascular disease CVD is the leading cause of morbidity and mortality worldwide, present in all countries, regardless of whether they are considered developed or not, with a progressive growth in prevalence and incidence, which implies that, in low- and middle-income countries, there is a greater challenge in the health sector to face these diseases 1,2. Thus, according to World Health Organization (WHO) data, CVD caused 17.9 million deaths (31 % of all deaths) worldwide in 2016, of which 75 % were in low and middle income countries; furthermore, 85 % of all global disabilities were caused or related to these diseases 3,4.
According to the who, to reduce CVD mortality, it is crucial to understand and adequately manage risk factors, including dyslipidemia, hypertension, diabetes mellitus, and smoking 5. It is also indicated that the highest number of CVD deaths are due to the high prevalence of dyslipidemia and diabetes mellitus, related to the increase of obesity in the population; high blood pressure and smoking have been controlled to a certain extent. Therefore, the early diagnosis and treatment of dyslipidemias, which represents the most important risk factor for the development of atherosclerosis, are considered fundamental to reduce the incidence and mortality from CVD 6.
Lipoprotein metabolic disorders are known as dyslipidemia, characterized by decreased HDL levels, or elevated plasma levels of cholesterol, LDL and/or triglycerides 7,8.
Dyslipidemia has become a public health problem in many countries due to its high prevalence and due to its causal relationship with chronic non-communicable diseases. At an early age, it can cause an atherosclerotic process and contribute to the development of CVD in adulthood 9.
Although the prevalence of dyslipidemia increases with age, it can also be present in young individuals; around 36 % of adults between 20 and 29 years old and 43 % between 30 and 39 years old have elevated lipid levels 10.
In developed countries such as the United States, up to 53 % of the population has some lipid disorder, and in 2011 the number of deaths from CVD represented 1 in 3 deaths 11. In Latin America, in 2010 it was reported that the prevalence rates of dyslipidemia in men and women, from 25 to 65 years old, were respectively: 75.5 % and 48.7 % in Barquisimeto-Venezuela; 70 % and 47.7 % in Bogotá; 50.4 % and 24.1 % in Buenos Aires; 73.1 % and 62.8 % in Lima; 62.5 % and 37.5 % in Mexico City; 52.2 % and 38.1 % in Quito, and finally 50.8 % and 32.8 % in Santiago de Chile 12. In addition, it is estimated that during 2020, seven out of ten deaths are due to non-communicable diseases and that coronary heart disease will be the main cause in the Latin American region 13.
The traditional management of dyslipidemia according to several international societies includes lifestyle modification and pharmacotherapy, based on groups considered as at low, medium or high risk for cardiovascular events 14. Thus, due to the asymptomatic nature of dyslipidemia, its identification requires adequate screening, which is beneficial for its early management and resolution.
The literature on the prevalence of dyslipidemia in the young population is scarce; in a systematic review of 352 articles made by Chou et al. for age groups from 21 to 39 years, no studies were identified that determine benefits or harms of screening, treatment in this specific population group, or strategies additional to screening, so extrapolation with the data obtained in clinical trials in adults is required 15.
Thus, the objective of the study was to determine the prevalence of dyslipidemia and its relationship with body mass index and waist circumference in students of the Superior Technology Specialization in Military Sciences and military personnel at University of Armed Forces of the Ecuador (ESPE). Likewise, it aimed to identify correlation between the prevalence of dyslipidemia with body mass index and waist circumference and determine the lower limits of the anthropometric indices studied to present dyslipidemia.
Materials and methods
This was an analytical, non-experimental study with a universe of 1100 students of Superior Technology Specialization in Military Sciences, class of Prevalence of Dyslipidemia in Military Students and Military Personnel Attending Primary Care in Ecuador and Correlation with Anthropometric Values 2019 - 2021, as well as 366 military personnel from ESPE. This academic and formative institute is in Ambato - Ecuador.
The studied looked at a sample of 495 students and 196 military personnel who meet the established inclusion and exclusion criteria and corresponds to a confidence level of 95 % and a margin of error of 3 %. The inclusion criterion included second-year students of the Superior Technology Specialization in Military Sciences, class of 2019- 2021 as well as military personnel working at the ESPE; exclusion criterion was the presence of an injury that does not allow daily physical activity.
Annual medical checkups were used as a source of information collection for both the students as well as military personnel . The medical records were from 2020, based on exams at Health Center B “Enforce” from October to December. The annual medical record includes personal information, medical check-up, laboratory tests, dental checkup, vital signs, anthropometry and psychological check-up.
The lipid profile was obtained with the chemical analysis equipment - Erba Mannheim, model XL-100, using reagent Cholesterol Liquid A (ref.: 990159, lot.: 190560) and Triglycerides MR (ref. 1155055, lot.: 15898) respectively.
The anthropometric values were obtained by measuring weight and height without shoes, in underwear, with a weight scale with manual altimeter -Seca model 700-; waist circumference (WC) was measured with a non-elastic measuring tape - Premax model 19394 at the level of the widest part of the buttocks, and at the level of the iliac crests.
The diagnosis of dyslipidemia was established according to Aguilar et al. (2004), and Latin- American Diabetes Association ALAD (2013): a) normal total cholesterol (<200mg/dl), b) high total cholesterol (> 200mg/dl), c) normal triglycerides (<150mg/dl), d) high triglycerides (> 150mg/dl) and, e) mixed dyslipidemia (Total-C> 200mg / dl and TG> 150mg / dl) 16,17.
The information obtained from the medical records was entered into a previously established Microsoft Excel matrix. Subsequently, the statistical analysis and correlation of the variables were carried out with the statistical program SPSS v22, and MedCalc, using Pearsons index and roc curve, respectively.
The study information was obtained with prior authorization from the Director of the Escuela de Formación de Soldados del Ejército “Vencedores del Cenepa” and with individual informed consent. None of the participants was exposed to any risk and all data was managed with confidentiality according to the Helsinki declaration and the ethic principle within the institution.
Results
The study was carried out on 495 students of the Superior Technology Specialization in Military Science, class of 2019-2021 with an age range between 19 and 23, and 196 military personnel at ESPE, with an age range between 23 and 51. In addition, all subjects were men (n: 495 and n: 196), and 91,9 % (n: 455) of the students and 97,45 % (n: 191) of the military personnel identified themselves as Latino (Table 1).
The mean value of total cholesterol was 148,65 mg/dl and triglycerides 106,55 mg/dl in students, and 185,59 mg/dl and 146,33 mg/dl, respectively in military personnel. In addition, the presence of hypercholesterolemia was 1,82 % (n: 9), hypertriglyceridemia 6,26 % (n: 31) and mixed dyslipidemia 0,40 % (n: 2) in students and hypercholesterolemia 9,186 % (n: 18), hypertriglyceridemia of 25,51 % (n: 50) and mixed dyslipidemia of 23,98 % (n: 47) in military personnel. Therefore, general dyslipidemia occurred in 8,48 % (n: 42) of students and 58,67 % (n: 115) of military personnel (Table 1).
Table 1 Characteristic of the study population, according to study, in Ecuador, 2020.
n: number, %: percentage, SD: standard deviation. Max: Maximum, Min: Minimum, BMI: Body mass index, WC: Waist circumference, WHtR: Waist height ratio
Source: Authors
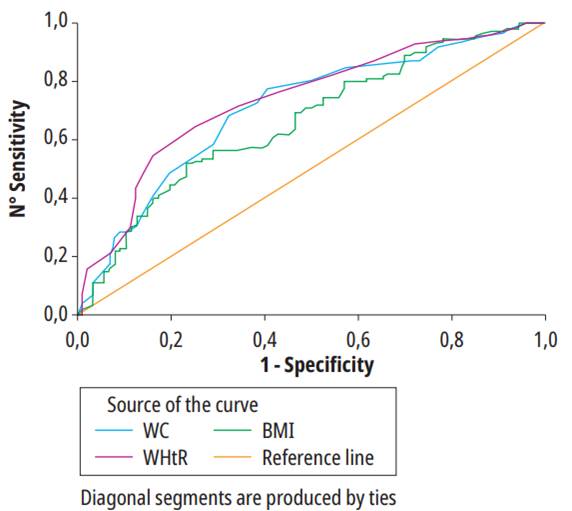
Table 2 shows that the lower limit for body mass index to present dyslipidemia in students is 25,67 kg/m2 (AUC: 0,523, 95 % IC: 0,478-0,568, p: 0,898), waist circumference is 76,5 cm (AUC: 0,506, 95 % IC: 0,461-0,551, p: 0,569), and waist height ratio of 0,47 (AUC: 0,555, 95 % IC: 0,510-0,599, p: 0,177), in addition, in military personnel the optimal cut of body mass index is 26,3 kg / m2 (AUC: 0,681, 95 % IC: 0,610-0,745, p: <0,0001), waist circumference is 86 cm (AUC: 0,716,95 % IC 0,647-0,778, p: <0,0001), and waist height ratio of 0,52 (AUC: 0,740, 95 % IC: 0,662-0,808, p: <0,0001) respectively (Table 2, Figure 1 and 2).
Table 2 Prediction of anthropometric index values for diagnosis of dyslipidemia, according to study, in Ecuador, 2020.
n: Number, %: Percentage, WC: Waist circumference, BMI: Body mass index, WHtR: Waist height ratio.
Source: prepared by the authors from the results obtained.
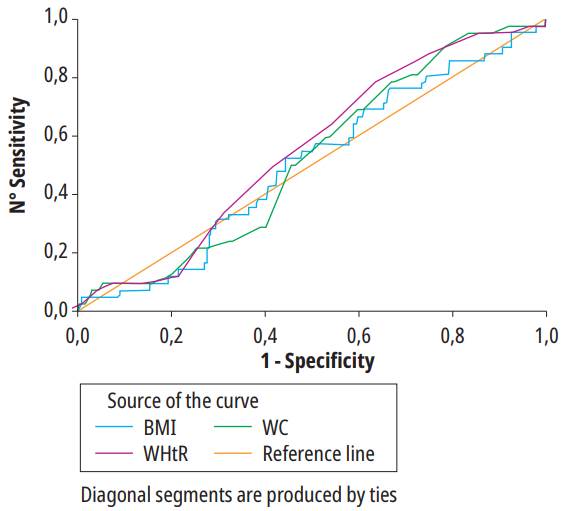
Source: prepared by the authors from the results obtained.
Figura 1. ROC curve for anthropometric indices to predic Dyslipidemia student in all the poblation. ROC: Receiver operating characteristics; WC: Waist circumference; BMI: Body mass index; WHtR: Waist height ratio.
Discussion
The periodic medical checkups carried out by the “Esforse” Health Center search for risk factors in the students of the Superior Technology Specialization in Military Science that can alter their academic performance and in the military personnel of the University of the Armed Forces of Ecuador - ESPE that subsequently can alter their professional activity.
A study by Shahid R (2019), in Saudi Arabia, in a young population of 85 patients, with ages between 18 and 45, 79 % male and previous diagnosis of ischemic stroke, indicated that 43,5 % have a history of dyslipidemia, showing that in young people with cardiovascular diseases, almost half have a previous alteration of lipids 18.
The prevalence of dyslipidemia in our study is remarkably low in contrast to the data obtained in the study by Martinez et al. in 2009, carried out at the Central Military Hospital in Mexico City, with a sample of 9784 soldiers with an age range of 35 to 65, where 27,17 % had hypercholesterolemia, 37,85 % hypertriglyceridemia and 25,51 % mixed hyperlipidemia; likewise, a study by Tovar et al. in 2012, in the Colombian Army, with a sample of 1,317 medical records of male patients with an average age of 31 years, evidenced 56,9 % of the population with dyslipidemia. Both studies showed significantly higher dyslipidemia than that observed in our population 19,20.
In Ecuador, the incidence of dyslipidemia in students and military personnel differs from our study. Muñoz and Muñoz in 2018 studied a military unit in Zamora, with a sample of 80 soldiers between 30 and 59 years old, finding the prevalence of hypercholesterolemia was 41.25 % 21. Likewise, Castillo’s study in 2018, with 178 soldiers, without a specific age range, from a military unit in Quito, observed that 57 % had dyslipidemia 22. Similarly, a study by Pacheco and Romero (2019), with a sample of 248 individuals with an average age of 36 years, treated at the Military Hospital of Guayaquil, evidenced that 42,7 % had hypercholesterolemia and 51,2 % hypertriglyceridemia 23.
When comparing our results with studies of the general university population, a difference is also observed in the prevalence of dyslipidemia. In a study carried out by Llamazares et. al. in 2005, in a population of 111 students between 17 and 23 years of age, from a university in Mexico, 14,4 % showed hypertriglyceridemia 24. Similarly, a study by Llive and Trujillo in 2013 of undergraduate students at the Pontifical Catholic University of Ecuador, with a sample of 902 students (men: 363 and women: 539) with an average age of 21, evidenced that in male students, 12,4 % had hypercholesterolemia, 13,5 % had hypertriglyceridemia, and 9,9 % had mixed dyslipidemia 25 .Therefore, students of the Superior Technology Career in Military Science and military personnel working at ESPE, show a low prevalence of dyslipidemia, in comparison with similar age groups within the region and the country, and this difference is more marked when compared with older age groups.
In addition, physical exercise is well known as a protective factor, as seen in the study by Carrasco et. al. in 2005, in a population of 200 participants, of which 79 were men, between 25 and 45 years old and 34 % performed physical activity. This study showed that 1,3 % had hypercholesterolemia and 11,4 % hypertriglyceridemia. Similar values to those were found in the students of our study, all of whom perform daily physical activities as part of their academic and professional training respectively 26.
In this way, this study associated the intensive daily physical activities carried out by students of the Superior Technology Career in Military Sciences and military personnel at University of Armed Forces of the Ecuador (ESPE) as part of their academic and professional formation respectively as a preamble for early prevention actions to reduce future morbidity and mortality of cardiovascular disease in professional military personnel.
Finally, there is no scientific literature on the lower limit values of the anthropometric indices in students and military personnel to present dyslipidemia, however, the results of this study (BMI: 25.67 kg/m2, WC: 76.5 cm, WHtR: 0.47 in students and BMI: 26.3 kg/m2, WC: 86 cm, WHtR: 0.52 in military personnel) serve as a guideline for future studies, in order to improve the primary prevention of dyslipidemia by assessing anthropometry values as primary care predictors.
Conclusion
The results obtained evidence that the prevalence of dyslipidemia in students and military personnel is smaller than the general university population and military personnel of similar age.
According to this study, a WC of 86 cm and a WHtR of 0.52 are the lower limit anthropometric indices to predict dyslipidemia in professional military personnel; however, in the university students studied the anthropometric indices do not show a significant value acceptable as predictors for dyslipidemia.