Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Acessos
Acessos
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares em
SciELO
Similares em
SciELO -
 Similares em Google
Similares em Google
Compartilhar
Revista colombiana de Gastroenterología
versão impressa ISSN 0120-9957
Rev Col Gastroenterol vol.28 no.3 Bogotá jul./set. 2013
Validation of a Questionaire Regarding Gastroesophageal Reflux (GERD) in a Colombian Population
Margarita Santa María, MD. (1), Mario Andrés Jaramillo, MD. (2), William Otero Regino, MD. (3), Martín Alonso Gómez Zuleta, MD. (4)
(1) Medical Resident in Geriatrics, Bogotá, Colombia.
(2) Medical Resident in Internal Medicine. Bogotá, Colombia.
(3) Professor of Medicine, Gastroenterology Unit, Universidad Nacional de Colombia, Gastroenterologist at the Clínica Fundadores, Clínica Carlos Lleras, and Hospital San Carlos in Bogotá, Colombia. waoteror@gmail.com
(4) Medical Internist and Gastroenterologist, Professor of Gastroenterology at the Universidad Nacional de Colombia, Gastroenterologist in the Gastroenterology and Digestive Endoscopy Unit at the Hospital El Tunal in Bogotá, Colombia.
Received: 21-05-13 Accepted: 26-06-13
Abstract
Background: Gastroesophageal reflux disease (GERD) is a chronic condition resulting from retrograde flow of the gastroduodenal contents into the esophagus and/or adjacent organs. Prevalence of GERD in Western countries ranges from 10% to 20%. GERD accounts for 4% of consultations with family doctors.
Objective: The objective of this study was to validate a scale for the Colombian GERDQ (Gastroesophageal Reflux Questionnaire) and develop a diagnostic method for determining the severity of GERD.
Materials and Methods: A diagnostic scale was validated on 84 patients and retested on 55 patients in the gastroenterology practice of the Clinica Fundadores in Bogotá. All patients diagnosed with GERD by gastroenterologists from January to April 2013 were asked to answer the GERD questionnaire.
Results: Multiple correspondence analysis showed that when GERDQ has an 8 point score its correlation with diagnoses made by gastroenterologists is 89% which implies a 92% correlation with the scale of Montreal.
Conclusion: This study shows that the GERDQ is a valid instrument for use in Colombia by general practitioners, internists and geriatricians for diagnosing GERD.
Keywords
Gastroesophageal reflux disease, diagnosis, scales, questionnaire, validation, evaluation of symptoms, impact.
INTRODUCTION
Gastroesophageal reflux disease (GERD) is a chronic condition resulting from the partial backflow of the gastroduodenal contents into the esophagus and/or neighboring organs. This can cause a wide spectrum of signs and symptoms in or outside of the esophagus and with or without damaging tissues.
Clinically, GERD has a variety of presentations. Since these symptoms do not correlate with endoscopic findings, patients may present a variety of combinations including:
a. Typical reflux symptoms (heartburn and/or regurgitation) with endoscopic evidence of damage to the mucosa.
b. Typical reflux symptoms with normal upper gastrointestinal (UGI) endoscopy.
c. Absence of typical reflux symptoms combined with endoscopic evidence of damage to the esophageal mucosa.
d. Atypical symptoms such as dyspepsia, coughing, asthma etc. (1-3).
Because of this variety the 2006 Montreal consensus defined GERD as, "a condition that develops when reflux of the gastric content causes unpleasant symptoms and/or complications" (1, 4).
GERD is frequently found in the community and in everyday clinical practice. Its incidence rate in Western countries is from 10% to 20%. In Latin America it ranges from 11% to 31% when diagnosed on the basis of heartburn and/or weekly regurgitation (5). It has a relatively lower rate in Asia of 5.2% to 8.5% (6). In family practice GERD accounts for approximately 4% of all consultations (3). Due to its varied clinical manifestations, it is frequently not easy to establish a diagnosis (7). Traditional diagnostic methods of the barium swallow and upper gastrointestinal (UGI) endoscopy have sensitivities of 10% to 50% and 30% to 50% respectively while 24 hour and monitoring of esophageal pH may present a normal reading for 6% to 15% of the patients with abnormal symptoms and endoscopic evidence of esophagitis. In addition, this technique is not broadly available. As a consequence of these issues, there is no gold standard objective diagnostic test (8) and, as a consequence, there has been constantly rising interest in the development of simple methods that can help primary care physicians to promptly diagnose GERD and orient the handling of this pathology (9). In this regard, the Diamond study (10) developed the Gastroesophageal Reflux Disease Questionnaire or "GERDQ" tool with the purpose of obtaining GERD diagnoses based on symptoms. The questionnaire is easy to use in primary patient care consultation and as such is an excellent aid for establishing a diagnosis and prescribing treatment. It is also excellent for monitoring medicated patients who have GERD. The GERDQ's questions are based on a selection of items from three previously validated GERD outcome tools synthesis: the reflux disease questionnaire or RDQ (11), the gastrointestinal symptom rating scale or GSRS (12) and the gastroesophageal reflux disease impact scale or GIS (13). Based on experience with these three, questions were chosen that would succeed in measuring the symptoms and seriousness of the ailment with greater accuracy (14, 15).
A comparison of questionnaires about the sensitivity and specificity of the GERDQ and RDQ for diagnosing GERD given to family doctors and gastroenterologists who took part in the DIAMOND study showed that a GERDQ score cutoff point of eight is closest to a diagnosis by a gastroenterologist. Patients with a score of eight or more have a high probability of suffering from GERD while those with a score lower than eight have a low probability. Because a score of eight has high specificity (71.4%) and sensitivity (64.6), it was proposed as the cutoff point for diagnosing GERD. It has been confirmed in various studies that the accuracy of a gastroenterologist's diagnosis is reached with the GERDQ questionnaire (14-17). Taking into consideration that in our midst there have been no studies validating international GERD questionnaires, we conducted this study to validate the GERDQ as a tool for the diagnosis of GERD in a Colombian population. This scale was selected taking into consideration that previous studies have shown that it is easy for primary health care physicians to apply and have shown its diagnostic value and accuracy (15, 18-20). The benefits of validation instead of developing a new scale are lower expenses, faster achievement, and internationally comparable results (21-23). The objective of this study was to evaluate the correlation of the GERDQ scale in a population group of patients with established diagnoses of GERD.
METHODOLOGY
This is a validation study of a diagnostic scale. The instrument was applied to 84 adults over 18 years of age from the contributory health care system who had been gastroenterology outpatients at the Clinica Fundadores in the city of Bogota. Signed informed consent forms were obtained from all participants prior to participation in the study. Subsequently, participants were interviewed by telephone within 15 days of initial consultation. 55 of the 84 patients who initially entered the data base answered the questionnaire. Interviews took place between January and April 2013.
The GERDQ is composed of 4 positive GERD indicators and two negative GERD indicators. The positive indicators are heartburn, regurgitation, sleep disorder due to these 2 reflux conditions, and use of drugs in order to relieve the symptoms (found to be positive indicators in the DIAMOND study). The two negative indicators are epigastric pain and nausea. Positive indicators were scored from 0 to 3 and negative indicators were scored in inverse order from 3 to 0. The GERDQ score was calculated as the sum of all indicators which gives possible total scores of 0 to 18. As suggested (17, 24, 25) a review committee was formed for the translation process. The committee was made up of 2 bilingual gastroenterologists with experience in the use of the tool and knowledge of the original language of the scale (17). They carried out the word for word translation. The important differences in the details between the two translations were solved jointly by the two translators who reached agreement on discordant elements (24). Subsequently this inverse translation was given to a third native English language reviewer who is immersed in Colombian culture. This review brought to completion the inverse translation and production of the final translated version of the scale. This translated version of the scale was subject to a preliminary adjustment trial on 15 patients by two different interviewers. The trial was used to evaluate ease of comprehension, ambiguous terms, time required for the measurement, need for special training of interviewers, and ease of evaluating the final score of the scale (24).
To determine whether the content of the scale validly reflects the structure of the domain of the syndrome, each item of the instrument was measured on at least five patients who had already been clinically diagnosed as having gastroesophageal reflux by a gastroenterologist. This construct is based on patient symptoms and on the answer to the question regarding treatment with proton pump inhibitors. In this case there were a minimum number of 30 patients (26). In order to determine "validity of criteria" about whether the scale functions in a manner similar to other certified instruments (18), it was compared with still another already validated scale, the Montreal definition. Their correlation was established by multiple correspondence analysis (MCA). To evaluate the sensitivity of the scale to change, the initial values were compared with subsequent scores taken from a time when the clinical conditions had been modified. In this case the appropriate therapy with proton pump inhibitors had commenced (27) and, within 15 days, patients were interviewed once again by telephone to answer questionnaire.
STATISTICAL ANALYSIS
A descriptive univariate analysis for continuous variables calculated the mean, median, standard deviation, variance, minimum, maximum and range. The frequency of categorical variables was analyzed and bar graphs were produced. Subsequently, in accordance with the proposed objectives, items of interest were validated by multiple correspondence analysis (MCA) which was used in an effort to obtain the relations among the the Montreal scale, the diagnosis by a gastroenterologist (diagnostic method of reference), the type of relation of the score obtained for each item by patients applying the scale with respect to the seriousness or the risk of gastroesophageal reflux. The MCA method was chosen because of the possibility of determining the relation between the categorical variables to which an exact correlation value cannot be given due to the nature of this data. IBM SPSS Statistics 20 was used for the analysis while SPAD was employed for the validation analysis. A consistency check done to determine the reliability of the instrument included construction of a number of different tables of contingency in which the answers to a determined item were compared. The answers from the first instrument were placed in the rows while and the answers from the second administration of the questionnaire were placed in the columns. The Kappa indexes and the significance of the correlation were extracted from these tables. The Chi Square Test was carried out in order to determine the degree of dependence between the classification of the proposed scale and the diagnosis by a gastroenterologist. The corrected Pawlik coefficient of contingency and its level of significance were produced in order to numerically specify the relation.
RESULTS
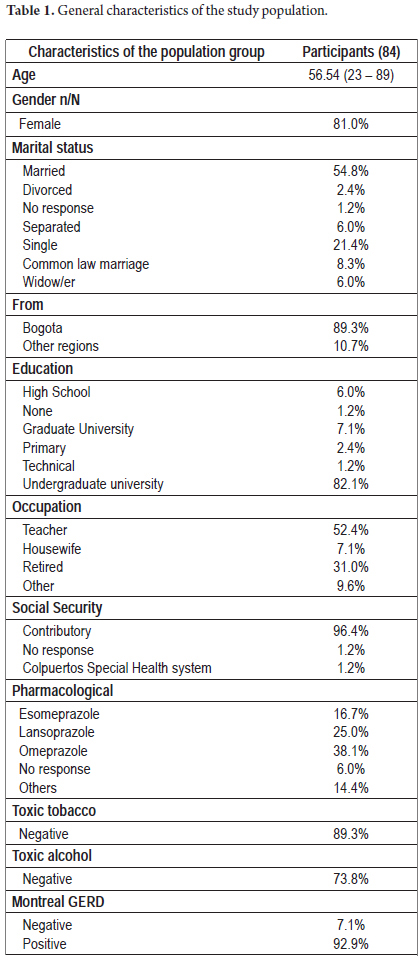
81% of the participants were women. The average age of the study population was 56: the youngest participant was 23 and the oldest was 89 (Table 1).
Relative frequencies of socio-demographic variables were as follows: 81% of the surveyed patients were women and 19% were men. 89.3% of the patients live in Bogota. 82.1% have professional degrees and 96.4% of the patients belong to the Contributory Health system. 82.1% of the patients declared having been diagnosed with GERD by a gastroenterologist. 17.9% had been diagnosed with strokes, diabetes mellitus, chronic liver pathologies, and high blood pressure. 38.1% of the patients take omeprazole, 25% take lansoprazole, 16.7% take esomeprazole and the remaining 20.2% take other varieties of medicine. 89.3% declared they had not been exposed to tobacco, and 73.8% denied consuming alcoholic beverages. The Montreal definition of GERD includes two categories for this variable: negative and positive. According to that definition, 92.9% of the study group members were positive.
As soon as patients answered, a score between 0 to 18 points was generated by the questionnaire. Conclusions from those scores are as follows: if the patient has a score of 0 to 2 points there is a low probability of GERD, a score of 3 to 7 points indicates a 50% probability of GERD, a score of 8 to 10 points indicates a 79% probability and a score of 11 to 18 points indicates an 89% probability of GERD. For purposes of analysis and to produce a classification for further validation, these score groups have been named: Low (0-2 points), Medium (3-7 points), High (8-10 points) and Very High (11-18 points), all this in order to classify the validation that is proposed later in this article (Table 2).
Figure 1 shows bar graphs of the classification variable and the severe GERD variable. The classification variable is the score given to each patient according to their answers to the questionnaire. It can be seen that 56% of the patients had a very high probability of having GERD, 32.1% had a high probability and the remaining 11.9% had a 50% probability of GERD according to the proposed scale. On the right hand bar graph which evaluates the severity of GERD, 0 is the lowest level of severity and 6 is the maximum level. The graph shows that 29.8% of the patients had severity values of 5, 20.2% had values of 2, 15.5% had severities of 6 and 11.9% had values of 0.
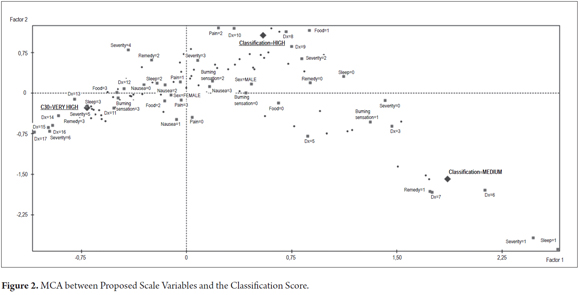
The validation of the items considered in this survey was carried out through the Multiple Correspondence Analysis method (MCA). Categories of the different items were classified and grouped according to the proposed GERD classification and the scores generated given that this group consists of categorical variables, and the MCA is a multi-variable analysis tool which permits analysis with few individuals and a large number of variables.
The first graph shows the MCA generated by the classification variable and the different scores obtained from the surveyed patients.
Figure 2 shows that scores from 11 to 17 are related to classifications of Very High probability of having GERD. These are associated with high severity scores from 4 to 6. The multiple correspondence analysis shows that the highest score on the severity question leads to a very high probability of GERD. A classification of High probability is correlated with scores from 8 to 10 and is related to severities of 2 and 3. These patients have a High probability of having GERD. The last group or cluster contains patients with Medium probability of presenting GERD. This classification is correlated with scores of 3 to 7, and is related to severities of 0 and 1. This group contains patients with a 50% probability of having GERD.
Figure 3 shows the Classification variables, GERD severity and Montreal GERD classification. The Very High Classification on the left has 89% probability of presenting GERD and is correlated with a Positive rating on the Montreal scale. The High Classification correlates slightly less well with a positive rating on the Montreal scale, whereas the Medium Classification is correlated to a negative rating on the Montreal scale.
Patients were resurveyed in order to evaluate the level of agreement of the questionnaire and the sensitivity of the scale to changes. Of the 84 initial patients, 54 were resurveyed. For the Montreal GERD variable, 88.89% of the patients were positive for GERD according to the Montreal consensus and the remainder of 11.11% did not present sufficient criteria. Table 3 shows comparisons of items evaluated.
Between the first and second interview changes in the variable "GERD classification were as follows: the proportion of patients with a "very high probability" of presenting GERD changed from 51.9% to 33%, the "Medium probability" of GERD increased from 11.1% to 42.6% and "High probability" moved from 37% to 24.1%. The variable "GERD severity" changed in very notorious ways as well. On the first survey, the highest incidence was in the high severity range or close to 6 while on the second survey the highest incidence appeared in the lowest severity classification or close to 0.
DISCUSSION
This investigation shows that the GERDQ scale has been validated as an measuring instrument in Spanish in a Colombian population group which had conclusive diagnoses of GERD just as it had already been validated in the English and Chinese languages (11). This demonstrates its benefits for diagnosing GERC on basis of symptoms. In our study, the correlation of a diagnosis with 8 points or more on the questionnaire and the diagnosis performed by the gastroenterologist was 89%. This is comparable to the positive predictive value of 92% (95% CI of 86% to 97%) which a Swedish study recently found (36).
A high score could make additional examinations unnecessary and commencement of PPIs recommended. Nevertheless, a request for upper endoscopy (28) would be justified for patients who suffer from "carcinophobia" or who have signs or symptoms of "soul". In Hatlebakk's study, the questionnaire interviews were conducted in an open endoscopy service. It established a negative predictive value of 22% (95% CI, 13% - 34%) In our study, the questionnaire interview was conducted with patients whose definitive diagnosis of GERD had included upper gastrointestinal (UGI) endoscopy. Consequently, the specificity of the questionnaire in our population group cannot be valued. Nevertheless, it can be inferred that for patients with less than 8 points (low probability) the use of an additional diagnostic test like upper endoscopy or studies of esophageal pH should be recommended in order to verify a diagnosis of GERD, as was recently suggested in a Swedish investigation (29).
The validation of this scale in Spanish profits a quick and cost effective measuring tool with broad clinical benefits for GERD diagnosis, determination of the severity of the ailment, as a follow-up tool to measure response to treatment, and epidemiologically to establish the prevalence of the ailment. With respect its epidemiological use this scale was recently used in Uruguay to determine the prevalence of GERD in the population without having validated the instrument beforehand (30) which is considered a limitation (31).
Changes of scores in second interviews conducted at least 15 days after start of treatment with PPIs, shown in Table 3, included a decrease in "high probability" of GERD from 51.9% in the first survey to 33.3% in the second, and an increase in "medium probability" from 11.1% to 42.6%. The severity of the symptoms suffered notorious changes. In the first survey the highest frequencies were in the high severity range or close to 6. In the second survey, the highest frequencies were located in the lowest severity classification or close to 0. These changes reflect improvement of patients' symptoms due to treatment with PPIs which suggests that the scale can be used to determine or measure response to treatment. Nevertheless, to determine this new use, specifically designed studies would be needed especially because only 64% of the population group were interviewed the second time in our study. This could be a limitation for establishing the true usefulness of the questionnaire for evaluating responses to PPI treatment. Other instruments such as the "GERD Impact Scale (GIS)" (32) and the Questionnaire on Changes of GERD (RDQ) (20, 33) have demonstrated their usefulness for facilitating doctor-patient dialogue after a diagnosis of GERD. These have already been validated for the Spanish speaking population (34) but are not diagnostic tools.

When the presence of the ailment was evaluated on the basis of the Montreal definition, with which instrument the scale to be validated was compared, it was found that 92.9% were positive according to this parameter. When applying the GERD scale, the probability of suffering the ailment was classified as low, medium, high and very high according to the score obtained. A GERDQ score of higher than 8 points was correlated with the gastroenterologist's diagnosis in 89% of cases (HIGH and VERY HIGH probability). According to this score 56% of the patients had VERY HIGH probabilities of suffering from GERD and 32.1% had HIGH probabilities. In establishing the correlation between the GERDQ scale and the Montreal definition, it may be appreciated that The VERY HIGH classification (92% probability of presenting GERD) is correlated with a positive Montreal score, while the MEDIUM classification is correlated with a negative Montreal score which demonstrates with assurance that the proposed scale is consistent with the Montreal consensus and fulfills one important criteria for its validation.
Having proven the GREDQ's diagnostic accuracy, an extension of this study will be initiated that uses the questionnaire in family practice outpatient visits and in general medicine to establish its efficiency in an open a endoscopy service in primary care consultation.
CONCLUSIONS
1. This study has, for the first time in Colombia and in the Spanish language, validated the GERDQ scale following the methodological recommendations for validation of a scale and using the multiple correspondence analysis.
2. The correlation between a high score of 8 on the scale and a gastroenterologists' diagnosis is close to 90%.
3. A change in the initial score is observed with treatment which suggests that the GERDQ eventually can be used for follow up of patients' treatments.
4. When the score is greater than 8, additional paraclinical studies should not be necessary for diagnosing GERD.
REFERENCIAS
1. N Vakil PK, J Dent, R Jones. Global Consensus Group. The Montreal definition and classification of gastroesophageal reflux disease: a global evidence-based consensus. Am J Gastroenterol 2006; 101: 1900-20. [ Links ]
2. Bredenoord A. Mechanisms of reflux perception in gastroesophageal reflux disease: a review. Am J Gastroenterol 2012; 107: 8-15. [ Links ]
3. N Vakil PM, G Salis, N Flook, M Hongo. An international primary care survey of GERD terminology and guidelines. Dig Dis 2008; 26: 231-6. [ Links ]
4. Vakil N vZS, Kahrilas P, Dent J, Jones R. Global Consensus Group. The Montreal definition and classification of gastroesophageal reflux disease: a global evidence-based consensus. Am J Gastroenterol 2006; 101: 1900-20. [ Links ]
5. Salis G. Revisión sistemática: epidemiología de la enfermedad por reflujo gastroesofágico en Latinoamérica. Acta Gastroenterol Latinoam 2011; 41: 60-69. [ Links ]
6. Jung H. Epidemiology of gastroesophageal reflux disease in Asia: a systematic review. J Neurogastroenterol Motil 2011; 17: 14-27. [ Links ]
7. B Seifert GR, N de Wit, C Lionis, N Hall, P Hungin, R Jones, M Palka, J Mendive. The management of common gastrointestinal disorders in general practice A survey by the European Society for Primary Care Gastroenterology (ESPCG) in six European countries. Dig Liver Dis 2008; 40: 659-66. [ Links ]
8. I Forgacs AL. Overprescribing proton pump inhibitors. BMJ 2008; 336: 2-3. [ Links ]
9. NoEDGD G. Dyspepsia: managing dyspepsia in adults in primary care. NICE guidelines 2004. [ Links ]
10. R Jones OJ, J Dent, N Vakil, K Halling, B Wernersson, T Lind. Development of the GerdQ, a tool for the diagnosis and management of gastro-oesophageal reflux disease in primary care. Aliment Pharmacol Therap 2009; 30: 1030-8. [ Links ]
11. Shaw M DJ, Beebe T. The Reflux Disease Questionnaire: a measure for treatment response in clinical trials. Health Qual Life Outcomes 2008; 6: 31. [ Links ]
12. Revicki D WM, Wiklund I, Crawley J. Reliability and validity of the Gastrointestinal Symptom Rating Scale in patients with gastro-oesophageal reflux disease. Qual Life Res 1998; 7: 75-83. [ Links ]
13. Jones R CK, Wiklund I. The gastrooesophageal disease impact scale: a patient management tool for primary care. Aliment Pharm Ther 2007; 25: 1451-9. [ Links ]
14. Tytgat GN MK, Tack J, Holtmann G, Hunt RH, Malfertheiner P, Hungin AP, Batchelor HK. New algorithm for the treatment of gastro-oesophageal reflux disease. Aliment Pharmacol Ther 2008; 27: 249-56. [ Links ]
15. Jones R, Junghard O, Dent J, et al. Development of the GerdQ, a tool for the diagnosis and management of gastro-oesophageal reflux disease in primary care. Aliment Pharmacol Ther 2009; 30: 1030-8. [ Links ]
16. Jones R, Coyne K, Wiklund I. The gastro-oesophageal reflux disease impact scale: a patient management tool for primary care. Aliment Pharmacol Ther 2007; 25: 1451-9. [ Links ]
17. Hambleton R. Adaptación de tests para uso en diferentes idiomas y culturas: Fuentes de error, posibles soluciones y directrices prácticas. In: Universitas E, ed. Psicometría. Madrid: Muñiz J; 1996. [ Links ]
18. Streiner D. Health Measurement Scales. A Practical Guide to their Development and Use. Oxford University Press 1995. [ Links ]
19. HG Guyatt SW, G Norman. Measuring Change Over Time: Assessing the usefulness of Evaluative Instruments. J Chronic Dis 1987; 40: 171-178. [ Links ]
20. Bland MJ. Validating scales and indexes. BMJ 2002; 324: 606-7. [ Links ]
21. Kerlinger F. Investigación del comportamiento. Métodos de investigación en ciencias sociales. 2002. [ Links ]
22. Sanchez R EJ. Validación de Escalas de Medicion en Salud. Rev Salud Pública 2004; 6: 302-308. [ Links ]
23. Alarcón AM. Medición en salud: Algunas consideraciones metodológicas. Rev Méd Chile 2008; 136: 125-130. [ Links ]
24. Prieto A. Method for Translation of Instruments to other Languages. Adult Education Quarterly. 1992; 43: 1-14. [ Links ]
25. Shaw M DJ, Beebe T. The Reflux Disease Questionnaire: a measure for treatment response in clinical trials. Health Qual Life Outcomes 2008; 6: 31. [ Links ]
26. Norman G. Componentes principales y análisis de factores. En: Libros M-D, ed. Norman GR, Streiner DL. Bioestadística. Madrid; 1996. p. 129-142. [ Links ]
27. HG Guyatt SW, G Norman. Measuring Change Over Time: Assessing the usefulness of Evaluative Instruments. J Chronic Dis 1987; 40: 171-178. [ Links ]
28. Hatlebakk JG. Endoscopy in gastrooesophageal reflux disease. Best Pract Res Clin Gastroenterol 2010; 24: 775-86. [ Links ]
29. Jonasson C MB, Bang C, Andersen KR, Hatlebakk JG. Randomised clinical trial: a comparison between a GerdQ-based algorithm and an endoscopy-based approach for the diagnosis and initial treatment of GERD. Aliment Pharmacol Ther 2012; 35: 1290-300. [ Links ]
30. Dacoll C UV, Tomasso G, Saona G, Aleman A, Cafferata ML, Villa-Gomez M, Cohen H. Prevalencia de la enfermedad por reflujo gastroesofágico en Uruguay. Gastroenterol Hepatol 2012; 35: 460-7. [ Links ]
31. Pérez-Alonso M R-DA, Sánchez-Blanco J, Romero Gómez M. Linguistic and transcultural validation of the Gastro-esophageal reflux disease questionnaire for a Spanish population. Pro Newsletter. Patient reported outcomes. 2009. [ Links ]
32. R Jones KC, I Wiklund. The gastrooesophageal disease impact scale: a patient management tool for primary care. Aliment Pharm Ther 2007; 25: 1451-9. [ Links ]
33. Federação Brasileira de Gastroenterologia; Sociedade Brasileira de Endoscopia Digestiva; Colégio Brasileiro de Cirurgia Digestiva; Sociedade Brasileira de Pneumologia e Tisiologia. Gastroesophageal reflux disease: diagnosis. Rev Assoc Med Bras 2011; 57: 499-507. [ Links ]
34. Nuevo Javier TM, Zapardiel Javier. Validación del cuestionario sobre alteraciones de reflujo (RDQ) y de la escala del impacto de la enfermedad por reflujo gastroesofágico (GIS) para población española. Gastroenterol Hepatol 2009; 32: 264-273. [ Links ]











 texto em
texto em