Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Acessos
Acessos
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares em
SciELO
Similares em
SciELO -
 Similares em Google
Similares em Google
Compartilhar
Revista colombiana de Gastroenterología
versão impressa ISSN 0120-9957
Rev Col Gastroenterol vol.31 no.2 Bogotá abr./jun. 2016
A Case Report Peritoneal Tuberculosis Simulating Peritoneal Carcinomatosis in a Hemodialysis Patient
Carmen Cecilia Gómez MD (1), Ana Madeleine Barrera López MD (1), Óscar Mauricio Pérez MD (1), Danny Novoa MD (1), Fredy Andrés Luna V. MD (1)
(1) Department of Internal Medicine of the Fundación Cardioinfantil in Bogotá, Colombia.
Received: 13-07-15 Accepted: 18-04-16
Abstract
This is a case study of a 69 year old immunosuppressed man with renal failure who was on hemodialysis. He developed chronic abdominal pain and acute diarrhea that progressed to intestinal obstruction. Diagnostic laparoscopy reported peritoneal carcinomatosis, but histological diagnosis showed that it was peritoneal tuberculosis.
Keywords
Immunosuppression, chronic renal disease, peritoneal tuberculosis, peritoneal carcinomatosis.
INTRODUCTION
Tuberculosis (TB) is a chronic infectious disease caused by the mycobacterium tuberculosis complex. It can affect any organ or tissue, but lung tissue is affected most often. According to the Ministry of Social Protection, in Colombia extrapulmonary TB accounts for 15% of the total number of confirmed TB cases. Several risk factors for acquisition and development of TB have been described in end-stage renal disease patients. There are extrinsic host factors, as in other people who contract tuberculosis, which depend on the degree of contagiousness and close and prolonged contact with the source. There are also intrinsic factors including age over 65 years, male gender, low socioeconomic status, related diseases, diabetes, silicosis and chronic obstructive pulmonary disease (COPD).
Mechanisms for abdominal infections do not differ from those in other patients infected with TB. They include primary infection through ingestion of contaminated milk, secondary infection through ingestion of infected sputum, and hematogenous infections by direct extension from neighboring organs. The most common manifestations are chronic abdominal pain, ascites, and diarrhea alternating with constipation. In some cases, there is intestinal obstruction. Diagnosis by examination of ascitic fluid usually shows lymphocytic exudate type fluid with small numbers of bacteria, not more than 3% in a smear and less than 30% in a culture. Laparoscopy with peritoneal biopsy is almost always needed. It shows the specific granulomatous lesion of TB in 100% of cases.
CASE PRESENTATION
The patient was a 69 year-old retired man who lived in Bogotá but was originally from Tota in the department of Boyacá. He had worked as an automobile painter and had a medical history of hypertension, pulmonary fibrosis, limited cutaneous systemic sclerosis, and renal failure. The patient was on hemodialysis, and being treated with 40 mg/day of furosemide, 600 mg/day of calcium carbonate, 7.5 mg/day of prednisolone, 50 mg/day of losartan, 50 mg/day of azathioprine and parenteral iron. The patient was brought to the emergency department in poor condition. His vital signs were: Blood pressure: 130/70 mm Hg, Heart rate: 100/min, Respiratory rate: 17/min, Oxygen saturation: 90%, Fraction of Inspired Oxygen: 24%, Weight 45 kg (Two months earlier it had been 50 kg.)
For one month prior to admission the patient had suffered from nonspecific abdominal pain of 4/10 intensity that did not radiate. In the last five days before admission he had suffered from abundant, watery stools without mucus or blood (five/day). He had been seen twenty days earlier with similar symptoms. At that time he was diagnosed with duodenitis after a CAT scan and treated with ciprofloxacin.
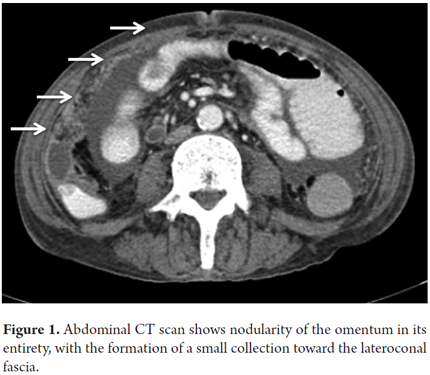
A physical examination showed a slightly distended abdomen, bowel sounds, pain on deep palpation of the lower abdomen without peritoneal irritation, but no masses or organ enlargement. Paraclinical tests showed no systemic inflammatory response. Altered electrolyte balance was found in relation to the underlying nephropathy. Because of occult blood in the patient's stool, a colonoscopy was performed. It showed thickening of the fold at ileocecal ampulla and a 2 cm sessile adenomatous polyp in the cecum with a wide base. Biopsies showed a tubular adenoma without high-grade dysplasia. A contrasted CT scan showed expansion of the middle third of the esophagus. In relation to the patient's history of scleroderma, the jejunal proximal loops were distended supplemented and the valves of Kerckring had thickened. There was marked impairment of mesenteric fat and the entire omentum was nodular. This was associated with multiple lymphadenopathy with a small collection toward the lateroconal fascia (Figure 1).
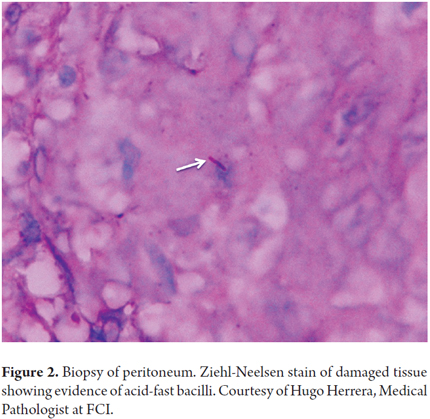
Because the patient had developed an intestinal obstruction, diagnostic laparoscopy was performed. It showed a large amount of sallow ascitic fluid, with severe visceral parietal adherence syndrome as well as adherence between loops. There was peritoneal seeding on the parietal and visceral peritoneum suggesting a macroscopic diagnosis of carcinomatosis peritoneal. The cytology study of the ascites fluid returned a negative report for malignancy and an adenosine deaminase test (ADA) reported 76.80 U/L (positive value> 36 U/ L). The biopsy (Figure 2) showed chronic granulomatous inflammation with the presence of Acid- Fast Bacilli (AFB) which is consistent with peritoneal tuberculosis. Treatment was initiated with twice a day doses of 300 mg of rifampicin and 150 mg of isoniazid, 1 g/day of pyrazinamide, and 2 g/day of ethambutol. A search for active TB in the patient's close relatives was negative. Prior to discharge, a culture of the patient's sputum culture was positive for pulmonary TB, so treatment was maintained.
DISCUSSION
Tuberculosis (TB) is a chronic infectious disease that can affect any organ or tissue, although the most commonly affected organs are the lungs. Of the 9,361 cases reported in Colombia to the National Surveillance System (SIVIGILA) in 2008, 7,566 cases (80.8%) were pulmonary TB and only 73 cases (0.7%) were meningeal tuberculosis. The 1,727 (18.3%) remaining cases were other extrapulmonary forms. (1) The abdomen is the sixth most common site of extrapulmonary TB. It most often affects the peritoneum, and the terminal ileum is the most common gastrointestinal site due to its great wealth of lymphoid aggregates. (2)
Some case series have shown an association between abdominal TB and classic risk factors such as HIV, transplants, substance abuse, renal failure, malignancy, low socioeconomic status, COPD and silicosis. (3) For patients with end-stage renal disease, associated risk factors include diabetes mellitus, patient age over 61 years, male gender, malnutrition, and iron overload. (4) Our patient had several of these factors as well as symptoms suggestive of infection which manifested as a chronic syndrome with alternating periods of diarrhea and constipation and even intestinal obstruction. Abdominal TB, as in this patient, presents with chronic abdominal pain and subsequent ascites in relation to peritoneal compromise, open or closed, with liquid lymphocytic exudative but with low levels of bacillus (not more than 3% in a smear and less than 30% in a culture). (2). In all cases, laparoscopy peritoneal biopsy is almost always necessary. (5)
Culturing material obtained from biopsy or ascites fluid is the gold standard for diagnosis, but it requires a minimum of two weeks to give results with current methods. Positive results have been obtained in 25% to 36 % of cases. (8) The ascitic fluid usually has a protein count higher than 3 g/dL, and a cell count of 150 to 4000 U/L which are predominantly lymphocytes (more than 70%). ADA levels are high in tuberculous ascites because of stimulation of T cells by mycobacterial antigens, so an ADA test of the ascitic fluid is useful. Its sensitivity and specificity are both greater than 80% with cutoff values over 35 U/L. (9)
Findings from CAT scans include smooth thickening and enhancement of the peritoneum, thickened and nodular mesentery, high density ascites (25-45 HU) and low density lymph nodes. (10) However, in the absence of risk factors or clinical findings to alert the physician to suspect TB, it is impossible to distinguish abdominal TB from peritoneal carcinomatosis, which is its main differential diagnosis, Crohn's disease, and others. (11, 12) Our patient presented unusual clinical manifestations of abdominal tuberculosis, but they were not sufficient to consider this diagnosis at admission. Later, B symptoms, the postoperative diagnosis of peritoneal carcinomatosis, the ADA test report and the direct biopsy became the diagnostic tools used for our patient. Finally, although the patient had no respiratory symptoms, we also documented pulmonary TB. Most patients do not have active associated pulmonary conditions at the time of diagnosis, but the association of lung and abdominal TB has been found in 20% of patients without HIV coinfection. (13).
REFERENCES
1. Instituto Nacional de Salud Colombia. Proceso R-02 vigilancia y control en salud pública, protocolo de vigilancia y control de tuberculosis [Internet]. [citado 28 de mayo de 2016]. Recuperado a partir de: http://www.ins.gov.co:81/lineas-de-accion/Subdireccion-Vigilancia/sivigila/Protocolos%20SIVIGILA/PRO%20Tuberculosis.pdf [ Links ]
2. Ministerio de la Protección Social, República de Colombia. Guía de Atención de la Tuberculosis Pulmonar y Extrapulmonar. Guías y Normas 412 - Tomo 2. p65 - GUIAS DE ATENCION -TOMO DOS.pdf [Internet]. [citado 28 de mayo de 2016]. Recuperado a partir de: https://www.minsalud.gov.co/Documentos%20y%20Publicaciones/GUIAS%20DE%20ATENCION%20-TOMO%20DOS.pdf [ Links ]
3. Chou C-H, Ho M-W, Ho C-M, Lin P-C, Weng C-Y, Chen T-C, et al. Abdominal tuberculosis in adult: 10-year experience in a teaching hospital in central Taiwan. J Microbiol Immunol Infect. 2010;43(5):395-400. [ Links ]
4. Li S-Y, Chen T-J, Chung K-W, Tsai L-W, Yang W-C, Chen J-Y, et al. Mycobacterium tuberculosis infection of end-stage renal disease patients in Taiwan: a nationwide longitudinal study. Clin Microbiol Infect. 2011;17(11):1646-52. [ Links ]
5. García Marcos S, Borrego FJ, Martínez de la Victoria JM, Sánchez Perales C, García Cortés MJ, Pérez del Barrio P, et al. Ileocecal tuberculosis during hemodialysis simulating carcinoma of the colon. Nefrología. 2001;21(3):314-8. [ Links ]
6. Shankar MSR, Aravindan AN, Sohal PM, Kohli HS, Sud K, Gupta KL, et al. The prevalence of tuberculin sensitivity and anergy in chronic renal failure in an endemic area: tuberculin test and the risk of post-transplant tuberculosis. Nephrol Dial Transplant. diciembre de 2005;20(12):2720-4. [ Links ]
7. Segall L, Covic A. Diagnosis of tuberculosis in dialysis patients: current strategy. Clin J Am Soc Nephrol. 2010;5(6):1114-22. [ Links ]
8. Sharma MP, Bhatia V. Abdominal tuberculosis. Indian J Med Res. 2004;120(4):305-15. [ Links ]
9. Huertas DG, Maccaferri AE, Cedeño MG, Orozco JC. Utilización de la adenosin desaminasa (ADA) como parámetro en el diagnóstico de pacientes con tuberculosis extrapulmonar: pleural, peritoneal y del SNC. Revista Medicina. 2002;8(3):207-16. [ Links ]
10. Mamo JP, Brij SO, Enoch DA. Abdominal tuberculosis: a retrospective review of cases presenting to a UK district hospital. QJM. 2013;106(4):347-54. [ Links ]
11. Suárez T, García V, Estrada T, Acosta F. Imágenes en tuberculosis abdominal, Rev Col Radiol. 2010;21:(4):3025-35. [ Links ]
12. Pulimood AB, Amarapurkar DN, Ghoshal U, Phillip M, Pai CG, Reddy DN, et al. Differentiation of Crohn's disease from intestinal tuberculosis in India in 2010. World J Gastroenterol. 2011;17(4):433-43. [ Links ]
13. Martínez Ordaz JL, Benavides RB. Gastrointestinal tuberculosis. Rev Gastroenterol Mex. 2004;69(3):162-5. [ Links ]











 texto em
texto em