Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Acessos
Acessos
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares em
SciELO
Similares em
SciELO -
 Similares em Google
Similares em Google
Compartilhar
Revista colombiana de Gastroenterología
versão impressa ISSN 0120-9957
Rev Col Gastroenterol vol.31 no.4 Bogotá out./dez. 2016
Nonalcoholic Steatohepatitis and Cardiovascular Risk Factors in Primary Care
Alicia Sahuquillo Martínez MD (1), Juan Solera Albero MD (2), José Antonio Rodríguez Montes MD (3), Ángel Celada Rodríguez MD (4), M.ª Loreto Tarraga Marcos MD (5), Pedro J. Tárraga López MD.(6)
(1) Primary Care Service at Hospital de Cuenca in Cuenca, Spain
(2) Primary Care Service at Hospital de Albacete in Albacete, Spain
(3) Professor of Surgery at Hospital Universitario La Paz de Madrid and the Universidad Autónoma de Madrid in Madrid, Spain
(4) Primary Care Service at Hospital Universitario de Albacete in Albacete, Spain
(5) Resident in Geriatric Medicine at Los Álamos de Albacete in Albacete, Spain
(6) Professor of Medical Sciences in the Integrated Attention Management and Universidad Castilla in La Mancha, Spain
Received:Â Â Â 12-04-16Â Â Accepted:Â Â Â 01-11-16
Abstract
Several factors motivate the growing interest in this disease. They include the high prevalence of the disease in the Western world, its ability to progress to more aggressive histological forms, and its association with diseases that increase cardiovascular risk.
Objective: The objective of this study was to analyze the relationship of nonalcoholic steatohepatitis (NASH) with cardiovascular risk factors in patients with criteria for metabolic syndrome.
Method: This is a descriptive cross-sectional study of 100 patients who had two or more cardiovascular risk factors, who did not consume alcohol or consumed only small amounts of alcohol, and who came to the primary care clinic. The patients selected underwent complete analyses including abdominal ultrasound. They were evaluated for hepatic steatosis, and, if they tested positive, it was stratified into three degrees. Among the qualitative variables used were sex, personal and family history of diabetes, hypertension, dyslipidemia, and the quantitative variables included age, weight, height, body mass index, pharmacological treatment, numbers of different analytical parameters, blood pressure and abdominal perimeter.
Results: There were 100 patients, 56% of whom were women. Patients' mean age was 61.84 SD +/- 9.5 years. Of the total number of subjects in the study, 23% did not have NASH, 29% had mild hepatic steatosis, 29% had moderate hepatic steatosis and 19% had severe hepatic steatosis. Of the men in the study, 82% had hepatic steatosis. Of the women, 28.57% did not have fatty livers. 22% were overweight and 38% obese. Only 22% had altered the systolic blood pressure and and 18% had altered diastolic blood pressure. 60% had altered basal glycemia. 36% had hypertriglyceremia, 41% had hypercholesterolemia including 65% with high LDL cholesterol and 16% with low HDL cholesterol. 83% of the patients had two or more criteria for metabolic syndrome.
Conclusions: There is a close relationship between the occurrence of NASH and cardiovascular risk factors in patients with metabolic syndrome, and it is advisable that the liver be analyzed.
Keywords
Hepatic steatosis, cardiovascular risk, ultrasound.
Introduction
The term nonalcoholic hepatic steatosis (NASH) was first introduced by Ludwig in 1980 to define a disease characterized by histological changes similar to those observed in individuals with alcoholic hepatitis, but who consume no alcohol or insignificant amounts.
NASH is part of a larger entity called non-alcoholic fatty liver disease (NAFLD). This includes simple hepatic steatosis, non-alcoholic liver steatosis and liver cirrhosis.
NASH is associated with insulin resistance syndrome (IR) and related conditions. It has been suggested that it is the hepatic manifestation of metabolic syndrome due to the presence of IR, obesity, type 2 diabetes mellitus, hypercholesterolemia, hypertriglyceridemia and hypertension. (1-3)
The mechanisms that lead to the development of hepatic steatosis are only partially understood, but it is accepted that the factors that determine the appearance of steatosis are insulin resistance, increased fatty acid influx to the hepatocytes, less elimination of triglycerides by the liver and less oxidation of fatty acids. (4-7)
It is now accepted that adipocytes can play a central role in the development of insulin resistance and NASH. The adipocyte is an important endocrine organ that can trigger an inflammatory process that facilitates evolution to steatohepatitis because it can secrete substances such as tumor necrosis factor alpha (TNF-α), leptin, resistin and free fatty acids. The concentration of free fatty acids is related to insulin resistance. (8-11)
For this reason, obesity should be considered a proinflammatory entity in which the liver and other tissues are exposed to cytokines produced in adipose tissue.
In hepatic steatosis, it is accepted that increased fatty acids within hepatocytes are due to increased arrival via the blood from lipolysis and to increased De novo synthesis in the hepatocytes themselves. During fasting, fatty acids that reach the liver come from hydrolysis of triglycerides stored in adipose tissue. (10-14)
Several circumstances motivate growing interest in NASH: the high prevalence of this disease in the Western world, its ability to progress to more aggressive histological forms, and its association with diseases that increase cardiovascular risk.
Although the actual prevalence of FDL is not known, there is a general consensus that it has increased significantly in recent years. Estimated prevalences vary considerably and range from 3% to 46% of the population analyzed. (14-19)
There are limited data on the natural histories of patients with NAFLD due to the indolent nature of the process and the absence of large prospective studies. Patients with simple steatosis present a benign course, in contrast to about 23% of patients with NASH, who progress to cirrhosis in a period of 10 to 15 years. On the other hand, 30% to 40% of patients with NASH have advanced fibrosis at the time of diagnosis. Some patients with cirrhosis due to NAFLD develop hepatocellular carcinoma in a period of 10 years. In addition to death from hepatic causes, increased cardiovascular mortality results in lower life expectancy than that of normal population controls of the same age and gender.
A diagnosis of NAFLD should be based on a combination of data from the medical history and non-invasive diagnostic methods. (20-24)
Appropriate diagnosis should include the following:
- Diagnosis of suspected NASH includes verification of alcohol withdrawal, exclusion of potential causes of hepatic steatosis, and diagnosis of possible associated diseases.
- Diagnosis of insulin resistance.
- Assessment of cardiovascular risks.
- Evaluation of severity of hepatic steatosis using non-invasive techniques such as ultrasound.
Objectives
Given the above, the objectives of this article are as follows.
Primary Objectives
The primary objective is to calculate the prevalence of hepatic steatosis in a population with metabolic syndrome or several cardiovascular risk factors.
Secondary Objectives
- Assess the epidemiological characteristics of these patients including gender, age and other cardiovascular risk factors.
- Stratify the degree of steatosis into mild, moderate or severe based on ultrasound criteria.
- Evaluate whether there is a correlation between echographic results, serum triglyceride and aminotransferase levels (GOT and GPT), and body mass index (BMI).
Materials and Methods
This is a descriptive cross-sectional study performed over 12 months. It included 100 patients from the primary care clinic of Casas de Haro in Cuenca, Spain. Study participants each had two or more cardiovascular risk factors but did not consume alcohol or only consumed insignificant amounts of alcohol.
Sample size was calculated on the basis of a 24% prevalence of metabolic syndrome in the general population and a 30% prevalence of NASH. Systematic random sampling was used to choose one of every two patients.
The selected population met the following inclusion criteria:
- Abstinence or low consumption of alcohol (<20 g/day in women and <30 g/day in men).
- Alteration or non-hepatic function tests not due to viral hepatitis or other hepatobiliary or systemic diseases, nor to drug causes (glucocorticoids, synthetic estrogens, amiodarone, aspirin, among others).
Once patients had been selected, the following demographic and biochemical variables were analyzed: age, gender, alcohol intake, history of diabetes, systemic arterial hypertension, weight, height, BMI (defined as weight/height2), arterial blood pressure (defined as ≥130/85), baseline serum glucose (Defined as ≥110 mg/dL), glycosylated hemoglobin, total cholesterol (hypercholesterolemia ≥200 mg/dL), HDL cholesterol (defined as <40 mg/dL in men and <50 mg/dL in women), LDL cholesterol, triglycerides (hypertriglyceridemia ≥200 mg/dL, for the criterion of MS due to ATP III ≥150 mg/dL), AST, ALT, bilirubin and alkaline phosphatase. Fasting glucose, cholesterol, triglycerides, transaminases, bilirubin and alkaline phosphatase were measured using routine laboratory techniques (colorimetric and enzymatic technique).
Personal and family histories of diabetes, hypertension, dyslipidemia, pharmacological treatment, abdominal perimeter and other analytical parameters were also collected.
Metabolic syndrome was defined when three or more of the criteria of the Adult Treatment Panel III (ATP III) were present.
- Abdominal obesity: hip circumference greater than 102 cm in men and greater than 88 cm in women
- Hypertriglyceridemia: ≥150 mg/dL
- HDL cholesterol: <40 mg/dL in men and <50 mg/dL in women
- Systemic hypertension: ≥130/85 mm Hg
- Fasting blood glucose: ≥110 mg/dL.
Ultrasonography of Liver
An Esaote MyLab 20 Plus ultrasound machine was used for abdominal ultrasounds. This is an innocuous, economical technique that is of great diagnostic value for abdominal pathologies. It has become the first line examination for patients with chronic hepatopathy for both and follow-up examinations.
The fundamental echographic characteristic of fat infiltration is increased liver echogenicity due to fat deposition (steatosis) in hepatocytes. Depending on the number of fatty hepatocytes, this deposit may be mild (<33%), moderate (33% to 66%) or severe (> 66%). This hyperechogenicity is fine-grained and very dense which gives the liver a bright appearance. It equals or exceeds the echogenicity of the pancreatic parenchyma and has slightly greater echogenicity than does the renal cortex. Increased echogenicity due to fat infiltration causes posterior sonic attenuation which makes evaluation of the deepest parts of the liver more difficult.
Depending on these characteristics, we can distinguish three grades of steatosis:
- Grade 1 is mild steatosis indicated by discrete increases in diffuse echogenicity with normal diaphragm and borders of intrahepatic vessels.
- Grade 2 is moderate steatosis indicated by moderate increases in diffuse echogenicity with difficulty assessing the diaphragm and intrahepatic vessels.
- Grade 3 is severe steatosis indicated by marked increases in echogenicity, with little or no visualization of the walls of intrahepatic vessels, diaphragm or posterior portion of the right hepatic lobe due to poor penetration of ultrasound.
Fat infiltration is usually distributed homogenously (diffuse steatosis), although irregular fat deposits (stellar or focal steatosis) may occur.
- The diffuse pattern affects the entire parenchyma, although hypoechoic zones that represent defined areas of normal parenchyma are sometimes seen. They is no evidence of any mass effect and they are frequently located in the hepatic hilum or in the area near the gallbladder.
- The focal pattern has regions of increased echogenicity on the bottom of a normal parenchyma. This pattern is common, especially in the right hepatic lobe. It is easy to diagnose and easy to differentiate from mass effect because it does not displace or compress the hepatic vessels or alter the liver contour. Also, it usually has geographical margins. Although echographic imaging is usually characteristic, diagnostic doubts are sometimes posed by other processes, such as hemangiomas (multifocal nodular steatosis), hepatic metastases, hematoma and abscesses. Therefore, computerized axial tomography (CAT scan) or magnetic resonance imaging (MRI) may be necessary; In some cases, a sonographically guided biopsy may be needed.
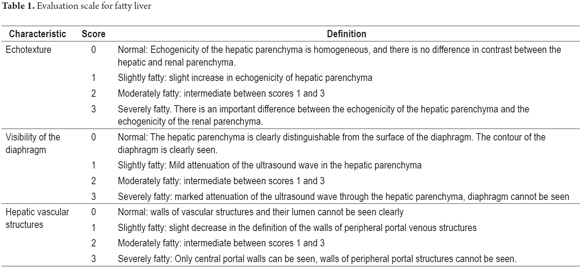
We used the measurement scale proposed by Chan et al. to evaluate the degree of fat infiltration (Table 1).
This scale stratifies liver steatosis into four grades: Grade 0 (0 points) indicates a normal liver, Grade 1 (1 to 3 points) indicates mild hepatic steatosis, Grade 2 (4 to 6 points) indicates moderate hepatic steatosis, and Grade 3 (7 to 9 points) indicates severe hepatic steatosis. (15-17)
The study was conducted in accordance with the Helsinki Declaration of 1983, and in all cases, the study participants signed an informed consent form.
Statistical analysis
This was an observational, descriptive and analytical cross-sectional study.
Variables noted in the data collection notebook were included and organized in the EXCEL database. Qualitative variables were expressed as exact values and percentages. Quantitative factors were expressed as means and standard deviations (SD).
Means were compared through Student's T-test for independent groups. When conditions of normality (application of the Kolmogorov-Smirnov test or Shapiro-Wilk test) were not met, the Mann-Whitney U test was used. The Chi-square test was applied to qualitative variables.
Using these criteria, the mean sensitivity of ultrasonography for diagnosis of NAFLD was 87% (60% to 100%) and the specificity was 86% (56% to 95%). The greater the amount of fat deposited, the greater was the sensitivity and specificity.
Results
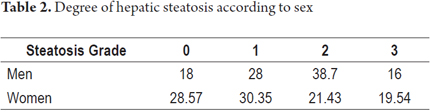
A total of 100 patients, 56% of whom were women, participated. Eighty-two percent of the men had hepatic steatosis: 28% were grade 1, 38.7% were grade 2, and 16% were grade 3 (severe). Of the women, 28.57% did not have fatty livers. Of the cases of steatosis among women, 30.35% were grade 1, 21.43% were grade 2, and 19.64% were grade 3 (Table 2). There were no statistical differences between the sexes.
The mean age was 61.84 ± 9.5 years with a minimum age of 33 and a maximum age of 87 years. The highest incidences of NASH and metabolic syndrome was observed in patients under 30 years of age (54%) and between 31 and 65 years of age (40%).
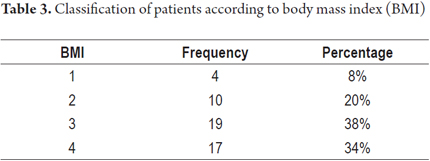
Twenty-four patients (24%) were overweight (defined as BMI ≥26-30 kg/m2), and 70 patients (70%) were obese (defined as a BMI ≥30 kg/m2). Mean weight was 86.59 kg ± 16.13 and mean BMI was 33.33 ± 4.31 kg/m2 (Table 3).
Of the patients diagnosed as having NASH, 38 (38%) had histories of diabetes mellitus and 41 (41%) had histories of hypertension. Mean fasting serum glucose was 115.31 ± 33.38 mg/dL and mean HgbA1C was 6.26 */- 5.1.
Mean systolic blood pressure was 135.68 ± 14.87 mm Hg, and mean diastolic blood pressure was 78.29 ± 10.92 mm Hg.
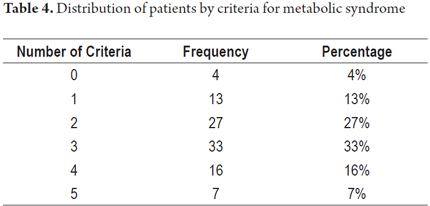
Eighty-three percent of patients had two or more criteria for metabolic syndrome (Table 4).
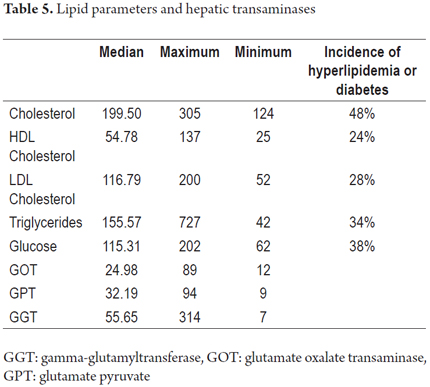
Thirty-four percent of these patients had hypertriglyceridemia, 48% had hypercholesterolemia, 24% had high levels of LDL cholesterol and 24% had high levels of HDL cholesterol (Table 5).
Twenty-three percent did not have NASH, 29% had mild hepatic steatosis, another 29% had moderate hepatic steatosis, and 19% had severe hepatic steatosis.
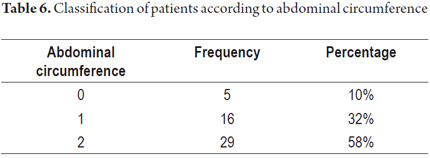
The mean abdominal circumference was 109.29 cm ± 12.10. The abdominal circumferences of 79% of the patients was above normal. This included 32% of the women and 58% of the men (Table 6).
GOT and GPT were within normal values ââin 94% of the subjects, while GGT was elevated in 66.6% of the subjects.
Of the patients with normal GOT and GPT, 72% had different degrees of hepatic steatosis as did 63.3% of the patients with normal levels of GGT.
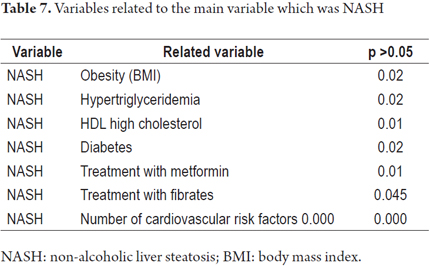
Statistical correlation of variables showed (Table 7):
- Obesity, mainly measured through BMI, was closely related to NASH (p = 0.02).
- Lipid parameters, especially hypertriglyceridemia (p = 0.02), were related to NASH. The protective role of HDL was also demonstrated (p = 0.01). Thus, the higher it is, the less frequent it is.
- Diabetes also showed a b relationship with the onset of NASH (p = 0.02).
- Treatment with metformin showed a weaker relation with the appearance of NASH (p = 0.01).
- Treatment with fibrates also demonstrated a relationship with the onset of NASH (p = 0.045).
- Appearance of metabolic criteria also demonstrated a relationship with NASH (p = 0.000); Thus, the greater the number of criteria, the greater the probability of occurrence of the disease.
Discussion
NASH is a chronic inflammatory liver disease of great relevance because of its b association with increasingly prevalent diseases such as obesity and Type 2 diabetes. Our results confirm this through the b relationship between NASH onset and these pathologies (p = 0.02). (1-5)
Metabolic syndrome is an association of risk factors with a high prevalence, especially in patients with some cardiovascular disease. The majority of studies agree that its prevalence in the general population is around 24% and is about 50% among patients with ischemic heart disease or some other vascular condition. Prevalence increases with age and weight. Prevalence in Spain has not been fully analyzed, but the first studies indicate prevalences of metabolic syndrome similar to those found in international studies. (6-11)
In our study, 46% of subjects met the criteria for metabolic syndrome. The prevalence of steatosis was 72%, with 34% of these patients suffering from obesity. We found a close relationship between the onset of NASH and the number of metabolic syndrome criteria (p = 0.000).
Obesity is the main cause of this liver disease. One study showed that among people who did not have known liver disease, 76% of those who did not drink alcohol, but who were obese, had a fatty liver. This proportion was only 16% among people whose weight was normal. These data demonstrate the importance of obesity as a cause of fatty liver. Seventy percent of the obese patients in our study have steatosis, and the degree of steatosis is related to BMI: the higher the BMI, the higher the degree of steatosis. (12-18)
Adult diabetes (Type 2 diabetes) is the second most frequent cause of NASH. Between 34% and 75% of diabetic patients develop NASH, and Type 2 diabetes is frequently associated with obesity. Patients with Type 2 diabetes and obese patients have a common metabolic disorder, known as insulin resistance, which may predispose them to the occurrence of hypertension and alterations in blood fats, such as cholesterol and triglycerides. Metabolic syndrome is the term currently used for simultaneous Type 2 diabetes, abdominal obesity, hypertension, alterations of blood fats and dyslipidemia. It is considered to be the main cause of fatty liver throughout the developed world. Metabolic syndrome contributes decisively to the accumulation of fat within the liver. (19-23)
NASH is related to cardiac and metabolic risk factors associated with insulin resistance and metabolic syndrome. About half develop liver fibrosis and 17% progress to cirrhosis in periods of up to 7 years, and 71%, progress to diabetes over a period of 13.7 years. (22, 23)
Randomized studies of NASH diagnosed by liver biopsies have been evaluated in which the effects of metformin were associated with improved hepatic function as measured by GPT-GOT, insulin sensitivity, C-peptide, plasma glucose, BMI and plasma cholesterol. Our study also confirms that patients treated with metformin are less likely to develop NASH than those who are not treated. (24-28)
Lipid-lowering therapy with statins and fibrates has shown mixed results although patients are more likely than not to benefit from them. Two small studies have evaluated the effects of fibrates in these patients. Gemfibrozil reduced transaminases and clofibrate reduced alkaline phosphatase, although neither drug improved the histological appearance of steatosis. These results do not allow wide recommendation of these drugs as therapeutic options for hepatic steatosis. Our study shows a statistically weak relationship between the intake of fibrates and the onset of NASH. (26-29)
In this study we used ultrasound as a method for diagnosing NASH, since there is evidence that, together with a good clinical history, it is a good diagnostic technique for hepatic steatosis.
With the results of our study, we can recommend that a study should be done to rule out NASH in all of our patients with several cardiovascular risk factors and even in patients with some criteria for metabolic syndrome. This should be evaluated early. (21)
Financing
This study was partly funded by the Research Commission of the Integrated Management of Albacete.
Conflicts of interest
The authors have no conflicts of interest.
REFERENCES
1. Martín-Domínguez V, González-Casas R, Mendoza-Jiménez -Ridruejo J, et al. Etiopatogenia, diagnóstico y tratamiento de la enfermedad del hígado graso no alcohólico. Rev Esp Enferm Dig. 2013;105(7):409-20. [ Links ]
2. Milié S, Lulié D, Stimac D. Non alcoholic fatty liver disease and obesity: biomechical, metabolic an clinical presentations. Worl J Gastroenterology. 2014;20(28):9330-7. [ Links ]
3. do S Alves de Carvalho M, Coelho Cabral P, Kruze Grande de Arruda I, et al. Risk factors associated with hepatic steatosis: a study in patients in the Northeast Brazil. Nutr Hosp. 2012;27(4):1344-50. [ Links ]
4. Loureiro C, Martínez A, Campino C, et al. Esteatosis hepática: ¿preludio de diabetes tipo 2 en población pediátrica? Nutr Hosp. 2014;29(2):350-8. [ Links ]
5. Buqué X, Aspichueta P, Ochoa B. Fundamento molecular de la esteatosis hepática asociada a la obesidad. Rev Esp Enferm Dig (Madrid). 2008;100(9):565-8. [ Links ]
6. Powell EE, Cooksley WGE, Hanson R, et al. The natural history of nonalcoholic steatohepatitis: a follow-up study of forty-two patients for up to 21 years. Hepatology. 1990;11:74-80. [ Links ]
7. Ludwig J, Viggiano RT, McGill DB. Non-alcoholic steatohepatitis: Mayo Clinic experiences with a hitherto unnamed disease. Mayo Clin Proc. 1980;55:342-8. [ Links ]
8. Bellentani S, Saccoccio G, Masutti F, et al. Prevalence of and risk factors for hepatic steatosis in northern Italy. Ann Intern Med. 2000;132:112-7. [ Links ]
9. Jick SS, Stender M, Myers MW. Frequency of liver disease in type 2 diabetic patients treated with oral antidiabetic agents. Diabetes Care. 1999;2:1067-71. [ Links ]
10. Hulcranzt R, Glaumann H, Lindberg G, et al. Liver investigation in 149 asymptomatic patients with moderately elevated activities of serum aminotransferases. Scand J Gastroenterol. 1986;21:109-13. [ Links ]
11. Rosety-Rodríguez M, Fornieles G, Rosely I, et al. Central obesity measurements predict metabolic syndrome in a retrospective cohort study of postmenopausal women. Nutr Hosp. 2013;28(6):1912-7. [ Links ]
12. Dixon JB, Bhathal PS, O´Brien PE. Nonalcoholic fatty liver disease: predictors of nonalcoholic steatohepatitis and liver fibrosis in the severely obese. Gastroenterology. 2001;121:91-100. [ Links ]
13. Kemmer NM, McKinney KH, Xiao SY, et al. High prevalence of NASH among Mexican American females with type II diabetes mellitus (Abstract). Gastroenterology. 2001;120:A117. [ Links ]
14. Vilchez López FJ, Campos Martín C, Amaya García MJ, et al. Las dietas de muy bajo valor calórico (DMBVC) en el manejo clínico de la obesidad mórbida. Nutr Hosp. 2013;28(2):275-85. [ Links ]
15. Kopelman PG. Obesity as a medical problem. Nature. 2000;404:635-43. [ Links ]
16. Matteoni CA, Younossi ZM, Gramlich T, et al. Nonalcoholic fatty liver disease: a spectrum of clinical and pathological severity. Gastroenterology. 1999;116:1413-9. [ Links ]
17. Lee RG. Non-alcoholic steatohepatitis: a study of 49 patients. Hum Pathol. 1989;20:594-8. [ Links ]
18. Dyson JK, Anstee QM, McPherson S. Non alcoholic fatty liver disease: a practical approach to treatment. Frontline Gastroenterol. 2014;5(4): 277-86. [ Links ]
19. Gómez Rubio M, Cuenca Morón B. Hepatopatía difusa e hipertensión portal. En: Ecografía digestiva. José María Segura Cabral; 2011. p. 93-8. [ Links ]
20. El-Hassan AY, Ibrahim EM, Al-Mulhim FA, et al. Infiltration of the liver: analysis of prevalence, radiological and clinical features and influence of patients management. Br Radiology. 1992;65:774-8. [ Links ]
21. Martín Algíbez A, Castellano Tortajada G. Seguimiento ecográfico de los pacientes con hepatopatía crónica. Rev Esp Ecograf Dig. 2006;8e(1). [ Links ]
22. Terán A, Crespo J. Cribado de la enfermedad hepática por depósito de grasa: cómo y a quién. Gastroenterol Hepatol. 2011;34(4):278-88. [ Links ]
23. Moreno Martínez A, Baluja Pino R. Síndrome metabólico. Edu Cont Lab Clin. 2009;12:36-46. [ Links ]
24. Alegría E, Cordero A, Laclaustra M, et al. Prevalencia del síndrome metabólico en población laboral española: registro MESYAS. Rev Esp Cardiol. 2005;58(7):797-806. [ Links ]
25. Pérez-Aguilar F, Benlloch M, Berenguer B, et al. Non-alcoholic steatohepatitis: physiopathological, clinical and therapeutic implications. Rev Esp Enferm Dig (Madrid). 2004;96(9):628-48. [ Links ]
26. Lazo M, Hernaez R, Bonekamp S, et al. Non-alcoholic fatty liver disease and mortality among US adults: prospective cohort study. BMJ. 2011;343:d6891. [ Links ]
27. Gill HK, Wu GY. Non-alcoholic fatty liver disease and the metabolic syndrome: effects of weight loss and a review of popular diets. Are low carbohydrate diets the answer? World J Gastroenterol. 2006;12(3):345-53. [ Links ]
28. Uygun A, Kadayifci A, Isik AT, et al. Metformin in the treatment of patients with non-alcoholic steatohepatitis. Aliment Pharmacol Ther. 2004;19(5):537-44. [ Links ]
29. Malnick SD, Beergabel M, Knobler H. Non-alcoholic fatty liver: a common manifestation of a metabolic disorder. QJM. 2003;96:699-709. [ Links ]











 texto em
texto em