Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Acessos
Acessos
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares em
SciELO
Similares em
SciELO -
 Similares em Google
Similares em Google
Compartilhar
Revista colombiana de Gastroenterología
versão impressa ISSN 0120-9957
Rev Col Gastroenterol vol.32 no.1 Bogotá jan./mar. 2017
https://doi.org/ https://doi.org/10.22516/25007440.131
A Case of Lemmel's Syndrome: A Rare Cause of Non-Neoplastic Obstruction of the Biliary Tract
Roberto Rodriguez F. MD (1), Héctor Polanía L. MD (2), Gabriela Evers S. MD. (3)
(1) General Surgery Resident at Universidad Surcolombiana in Neiva, Colombia
(2) Clinical and Surgical Gastroenterologist at the Universidad de Caldas and Chief of Clinical Sciences at Universidad Surcolombiana in Neiva, Colombia
(3) Physician at the Universidad Libre de Cali in Cali, Colombia
Received:Â Â Â 18-03-16Â Accepted:Â Â Â 16-12-16
Abstract
We report the case of a 77-year-old woman with jaundice but no evidence of choledocholithiasis or other alterations of the biliary tree except for a duodenal diverticulum. Lemmel's syndrome was diagnosed and an endoscopic sphincterotomy with stenting was performed. Lemmel's syndrome is a rare disease that must be considered as a cause of obstructive jaundice.
Keywords
Lemmel syndromes, duodenal diverticulum, obstructive jaundice.
INTRODUCTION
Although the most frequent duodenal diverticula is in the colon, the duodenum is their second most frequent location, (1-10) and 5% and 10% of the general population may develop them. Their prevalence increases with age to the point that they may affect 15% to 20% of all people at 80 years of age. Nevertheless, since most are asymptomatic, they are usually found incidentally. Of these diverticula, 75% are found around the ampulla of Vater. Those located at 2-3 cm above the ampulla are known as juxtapapillary duodenal diverticula. (2) Patients rarely have symptoms, but when they do they can include abdominal pain, steatorrhea, gastrointestinal bleeding, perforations, intestinal obstructions, diverticulitis and pathologies of the biliary tract such as obstructive jaundice, cholangitis and pancreatitis. (3)
Lemmel's syndrome, also known as intermittent obstructive jaundice, was first described in 1934. Lemmel observed duodenal diverticula near the ampulla of Vater favored the development of pancreatobiliary diseases. Nevertheless, there are very few published cases, and this pathology has yet to be thoroughly studied. It is defined as hyperbilirubinemia at the expense of direct bilirubin and is secondary to the relationship of a juxtapapillary diverticulum with biliary tree alterations but without evidence of choledocholithiasis or other direct causes of hyperbilirubinemia. (4-13) Although choledocholithiasis commonly occurs in 20% to 40% of patients with periampullary duodenal diverticula, 41% of patients with juxtapapillary diverticula and symptoms secondary to biliary obstruction have normal bile and pancreatic ducts in imaging studies. (2)
In general, most patients not only have jaundice due to direct bilirubin but also have other symptoms such as acute abdominal pain and cholangitis. Characteristically, patients present postprandial epigastric pain and a sensation of fullness. (2) Although the exact mechanism has not yet been precisely defined, it is postulated that it is related to increased pressure, mechanical obstruction, distortion of the distal portion of the common bile duct and the pancreatic duct or to dysfunction or spasms of the sphincter of Oddi. All this favors reflux of the duodenal contents and intestinal bacteria into the common bile duct and the pancreatic duct and to biliary stasis which ultimately produces the symptoms caused by obstructive pathology of the intraduodenal distal third of the bile duct. (3)
CASE DESCRIPTION
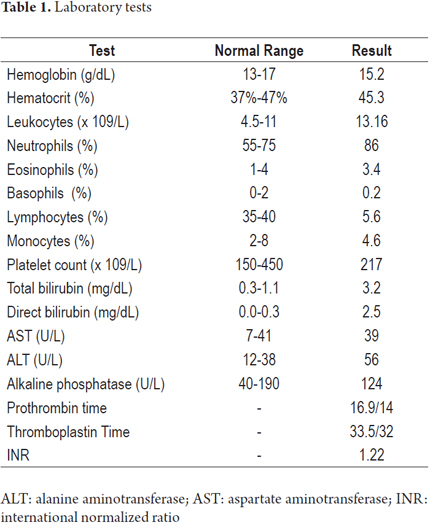
The patient was a 77-year-old unemployed rural woman who sought medical treatment after suffering epigastric pain for one month. The pain radiated towards the right lumbar region and was associated with a sensation of postprandial abdominal distension. She reported that one week prior to the visit jaundice had begun and progressively affected her mucosa and intermittent patches of skin and was associated with unquantified febrile episodes. She had no relevant medical history. Physical examination upon admission showed normal vital signs and no fever or jaundice. Upon palpation, she felt pain in the epigastrium but without signs of peritoneal irritation. The CBC from the initial paraclinical studies showed leukocytosis, neutrophilia, and direct hyperbilirubinemia but no other liver alterations. (Table 1)
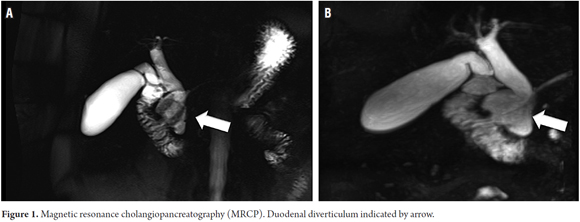
Hepatobiliary ultrasonography showed a âthin-walled, distended gallbladder, with no stones inside and a normal bile duct with a normal diameter.â Given the paraclinical and sonographic findings, it was considered that the patient had jaundice with hyperbilirubinemia due to direct bilirubin probably resulting from an obstructive process. Magnetic resonance cholangiopancreatography (MRCP) showed bloating of the gallbladder, no images of calculi, dilatation of the extrahepatic bile duct to the distal bile duct, and slight dilatation of the pancreatic duct which had smooth appearing contours. Immediately prior to the junction of these ducts with the duodenum, a saclike formation was identified that was considered to correspond to a duodenal diverticulum. (Figure 1).
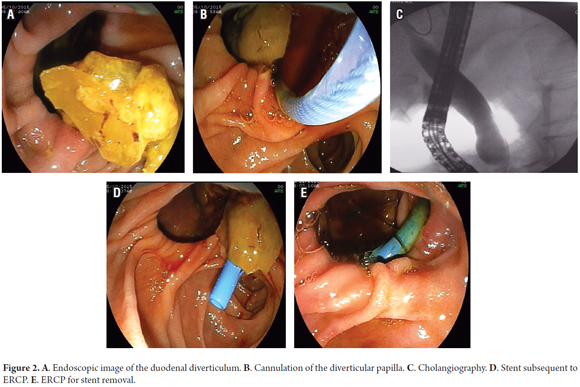
Due to the persistence of the obstructive liver profile, an endoscopic retrograde cholangiopancreatography (ERCP) plus papillotomy was performed. A 15 mm extrahepatic biliary tract without filling defects was found along with abundant alimentary remains in the cavity of the duodenal diverticulum. It was removed with a Dormia, and a 10 x 10 mm biliary stent was placed (Figure 2) prior to papillotomy. After developing post-ERCP pancreatitis, the patient improved and was discharged. The stent was removed 10 weeks later without complications.
DISCUSSION
Intermittent obstructive jaundice due to direct hyperbilirubinemia produces Lemmel's syndrome's which is related to diverticula in the area of the Ampulla of Vater and biliary tract disorders such as recurrent lithiasis, cholangitis, and pancreatitis. Diagnosis may be difficult, but clinical suspicion of this pathology in patients with direct hyperbilirubinemia without choledocholithiasis is of utmost importance to avoid making inappropriate decisions. Diagnosis should start with identification of whether or not a periampullary diverticulum is present. (5) It is confirmed by imaging studies including biliopancreatic endoscopic ultrasonography, ERCP, abdominal computed tomography (CT), and magnetic resonance cholangiopancreatography. (9) Any of these can demonstrate lateral compression in the common bile duct as the cause of the presence of the diverticulum. (4) In addition, abdominal imaging studies of this type have been reported as useful diagnostic tools for identifying duodenal pathologies, improving difficulties and clarifying clinical and ultrasound findings. (6)
According to the literature, the best way to see whether these diverticula are present is to use lateral endoscopic vision during ERCP. CT scans and MRIs of this type of diverticula show pocked lesions, usually containing gas, on the thin wall in the second portion of the duodenum. However, in some cases these periampullary diverticula are filled with fluid and can often be confused with pancreatic pseudocysts, cystic neoplasms at the head of the pancreas, or even metastatic lymphadenopathy. Therefore, imaging should not be used alone: to arrive at a correct diagnosis for these patients there must also be a high index of suspicion based on clinical history, symptoms and paraclinical findings. (5)
In the case we have reported, the clinical and paraclinical reports of the hepatic profile indicated that the patient had obstructive jaundice due to direct hyperbilirubinemia. Therefore, we performed a magnetic resonance cholangiopancreatography (MRCP) which described a saclike formation filled with liquid and in close contact with a liquid-air level in the second portion of the duodenum. At the junction of the common bile duct and the pancreatic duct, it was possible to approach the case with a specific diagnostic suspicion and to carry out the treatment indicated. In this case, we performed an ERCP that confirmed the presence of the diverticulum and the diagnosis of Lemmel's syndrome. Then, the patient underwent a papillotomy and placement of a bile stent. (14-17)
Currently the diagnosis of this syndrome is most often made during an ERCP or endoscopic ultrasonography, as both can confirm the diagnosis, exclude other possible causes such as choledocholithiasis and tumors, and readily allow performance of an endoscopic sphincterotomy. (4)
Treatment of asymptomatic patients is generally not recommended. However, since almost all patients with this syndrome have symptoms including jaundice, abdominal pain and cholangitis that are related to obstruction and extrinsic compression of the common bile duct, some type of treatment is likely to be necessary and should be performed. (5) Symptomatic periampullary diverticula can be treated conservatively, endoscopically or surgically. (8) The aim of treatment in these cases is to relieve biliopancreatic obstruction, either by surgical or endoscopic resection of the diverticulum, endoscopic sphincterotomy, by implanting a biliary stent or by simply removing the contents of the diverticulum. This contents may be an enterolith or to the remains of impacted food. In the literature it has been reported that endoscopic treatment has a high success rate. (6) Surgical treatment is reserved for severe complications such as perforations, severe hemorrhaging and conditions that occur with sepsis. (6-12) ERCP with sphincterotomy is preferable in cases of pancreatobiliary disorders. (1) This procedure is indicated because not all forms of Lemmel's syndrome are caused by extrinsic compression (distension of the periampullary diverticulum) of the common bile duct. It has been proposed that dysfunction of the Sphincter of Oddi or chronic fibrosis of the papilla may also cause this pathology. In these cases, ERCP with sphincterotomy is simplest and most practical procedure for resolving the problem. (5)
Because only a few cases have been reported in the literature, we do not have a clear understanding of the true incidence of Lemmel's syndrome. In spite of this, its existence must be taken into account in the differential diagnosis of intermittent obstructive jaundice. It is necessary to understand the few case reports published in the medical literature which support the appropriate diagnostic and therapeutic management that was given to our patient in addition to posing new challenges to the approach and treatment of future cases. (17)
CONCLUSION
When an elderly patient has a clinical picture compatible with obstructive jaundice, but lithiasis in the common bile duct (choledocholithiasis) is absent, and there is no tumor mass, the possibility that a periampullary diverticulum is causing the symptoms should always be considered. Conservative management with imaging studies should always be the first option for diagnosing these patients, and surgical or endoscopic surgery should be used with caution to provide safe and effective treatment of this syndrome. (7)
REFERENCES
1. Wang Y, Liu K, Yang J. A rare cause of obstructive jaundice. Clin Gastroenterol Hepatol. 2013;11(7):A31. [ Links ]
2. Musumba C, Britton E, Smart H. A man presenting with severe postprandial epigastric pain, jaundice, and pyrexia: more than the usual suspects? Gastroenterology. 2013;144(2):274-469. [ Links ]
3. Gómez Espín R, Sánchez Quiles I, Hallal H, et al. Lesión hepatocelular aguda tras exposición sucesiva a clozapina y olanzapina en un paciente con hepatitis crónica C. Gastroenterol Hepatol. 2010;33(2):150-2. [ Links ]
4. Rouet J, Gaujoux S, Ronot M, et al. Lemmels syndrome as a rare cause of obstructive jaundice. Clin Res Hepatol Gastroenterol. 2012;36(6):628-31. [ Links ]
5. Kang HS, Hyun JJ, Kim SY, et al. Lemmels syndrome, an unusual cause of abdominal pain and jaundice by impacted intradiverticular enterolith: case report. J Korean Med Sci. 2014;29:874-8. [ Links ]
6. Perdikakis E, Chryssou EG, Karantanas A. Diagnosis of periampullary duodenal diverticula: the value of new imaging techniques. Ann Gastroenterol Q Publ Hell Soc Gastroenterol. 2011;24(3):192-9. [ Links ]
7. Karayiannakis AJ, Bolanaki H, Courcoutsakis N, et al. Common bile duct obstruction secondary to a periampullary diverticulum. Case Rep Gastroenterol. 2012;6:523-9. [ Links ]
8. Beisani M, Espin F, Dopazo C, et al. Therapeutic management of juxtapapillary duodenal diverticulum]. Cir Esp. 2013;91(7):463-5. [ Links ]
9. Ono M, Kamisawa T, Tu Y, et al. MRCP and ERCP in Lemmel syndrome. Jop. 2005;6(3):277-8. [ Links ]
10. Oukachbi N, Brouzes S. Management of complicated duodenal diverticula. J Visc Surg. 2013;150(3):173-9. [ Links ]
11. Wiesner W, Beglinger C, Oertli D, et al. Juxtapapillary duodenal diverticula: MDCT findings in 1010 patients and proposal of a new classification. Clin Imaging. 2010;34(2):161. [ Links ]
12. Bittle MM, Gunn ML, Gross J, et al. Imaging of duodenal diverticula and their complications. Curr Probl Diagn Radiol. 2012;41(1):20-9. [ Links ]
13. Alventosa E, Gonzalez CG, Perdomo A, et al. Ictericia obstructiva con nombre propio: síndrome de Lemmel. Objetivos Material y Método; 2012. [ Links ]
14. Fujita N. ERCP for intradiverticular papilla: two- devices-in-one-channel method. Gastrointest Endosc 1998;48(5):0-3.
15. Lobo DN, Balfour TW. ERCP for intradiverticular papilla: not the latest trick. Gastrointest Endosc. 1999;50(1):144. [ Links ]
16. Tajima A, Kurata H. Elderly patient with Lemmel syndrome. JSM Gastroenterol Hepatol. 2014;2(1):1010. [ Links ]
17. Rouet J, Gaujoux S, Ronot M, et al. Lemmels syndrome as a rare cause of obstructive jaundice. Clin Res Hepatol Gastroenterol. 2012;36(6):628-31. [ Links ]











 texto em
texto em