Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Acessos
Acessos
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares em
SciELO
Similares em
SciELO -
 Similares em Google
Similares em Google
Compartilhar
Revista colombiana de Gastroenterología
versão impressa ISSN 0120-9957
Rev Col Gastroenterol vol.34 no.1 Bogotá jan./mar. 2019
https://doi.org/10.22516/25007440.356
Case report
Lemmel’s Syndrome Documented with Endoscopic Ultrasound
1Internista gastroenterólogo. Profesor asociado de medicina, Universidad Nacional de Colombia. Hospital Universitario Nacional, Unidad de Gastroenterología y Ecoendoscopia (UGEC). Hospital Fundación Santa Fe de Bogotá. Bogotá D. C., Colombia
2Especialista en Gastroenterología, Universidad Nacional de Colombia. Especialista en Medicina Interna, Hospital Occidente de Kennedy, Hospital Universitario Nacional. Bogotá D. C., Colombia
3Especialista en Gastroenterología, Universidad Nacional de Colombia. Especialista en Medicina Interna, Universidad Nacional de Colombia, Hospital Universitario Nacional. Bogotá D. C., Colombia
Obstructive jaundice is a frequent for patients to come to emergency services. Lemmel’s syndrome is an obstructive biliary syndrome secondary to a papillary duodenal diverticulum for which other causes of obstructive jaundice have been ruled out. We describe a case of obstructive jaundice in an 84-year-old patient who underwent magnetic resonance imaging and biliopancreatic endosonography to rule out biliary lithiasis. Subsequently, the patient underwent ERCP where the papillary diverticulum was evident and without choledocholithiasis. A papillotomy was performed. Afterwards, the patient’s clinical evolution was favorable.
Keywords: Jaundice; Lemmel’s syndrome; abdominal pain; ERCP
La ictericia obstructiva es una causa frecuente de consulta en los servicios de urgencias. El síndrome de Lemmel se describe como un síndrome biliar obstructivo secundario a un divertículo duodenal perpipapilar en el que se han descartado otras causas de ictericia obstructiva. Se describe un caso de ictericia obstructiva en una paciente de 84 años, en la que se realiza resonancia magnética y endosonografía biliopancreática que descartan litiasis biliar; posteriormente, es llevada a colangiopancreatografía retrógrada endoscópica (CPRE), en la que se evidencia divertículo peripapilar sin coledocolitiasis, y se realiza papilotomía, luego de la cual la paciente presenta una evolución clínica favorable.
Palabras clave: Ictericia; síndrome de Lemmel; dolor abdominal; CPRE
Case presentation
We present the case of an 84-year-old patient who came to the emergency department after three days of pain in the right hypochondrium and epigastrium which radiated to the back and was associated with nausea but not vomiting. Jaundice without systemic inflammatory response or peritoneal irritation was evident in the clinical assessment. Biochemical tests showed a cholestatic pattern with direct hyperbilirubinemia. Total bilirubin was 2.70 mg/dL, direct bilirubin was 2.40 mg/dL, his alkaline phosphatase level was 265 IU/L, alanine aminotransferase (ALT) was 122 U/L, and aspartate aminotransferase (AST) was 105. Abdominal ultrasonography found that common bile duct measured 7 mm. In light of intermediate probability of choledocholithiasis, magnetic resonance cholangiography was ordered. It found postcholecystectomy syndrome, a bile duct that measured 11 mm, but not stones within the duct (Figure 1). Given that magnetic resonance cholangiography did not establish a diagnosis, it was decided to perform biliopancreatic ultrasonography. During endoscopy, a peripapillary duodenal diverticulum was evident. Ultrasound showed a dilated bile duct without calculi (Figure 2, Video 1).

Figure 1 Magnetic resonance cholangiography. A. Dilated bile duct is observed, without filling defects inside. B. A duodenal diverticulum can be seen along with the absence of a gall bladder due to surgical history.
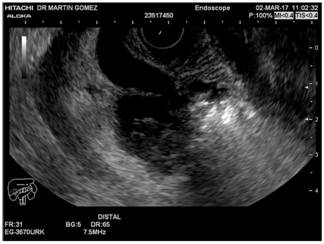
Figure 2 Biliopancreatic endoscopic ultrasound. Dilation of the extrahepatic bile duct with duodenal diverticulum compressing the bile duct can be seen.
Video 1. The first part of the video shows the endoscopic view of a large peripapillary diverticulum which is corroborated in the second part of the video which also shows detritus in the duct. https://youtu.be/1bjkFFDgCHE
While hospitalized, the patient suffered persistent abdominal pain with elevated bilirubin, so we decided to perform diagnostic and therapeutic endoscopic retrograde cholangiopancreatography (ERCP). During ERCP, a large peripapillary diverticulum was seen. Selective cannulation of the bile duct and a subsequent median papillotomy were performed which resulted in abundant bile output, without biliary sludge or stones (Figure 3).
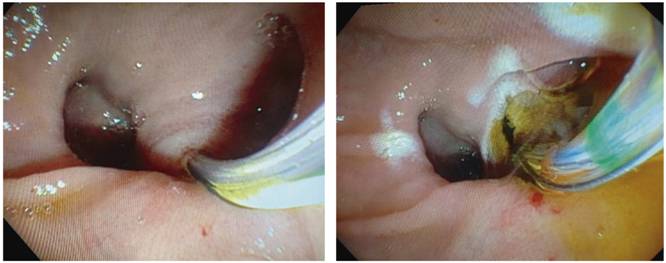
Figure 3 ERCP. A. Diverticular papilla, cannulation with arch papillotome. B. Medium papillotomy with abundant bile output.
After ERCP, the patient’s jaundice and episodes of abdominal pain resolved, the patient’s evolution was favorable, and the patient was discharged with outpatient follow-up.
Discussion
Obstructive jaundice is a frequent reason for consultation in emergency services. First described in 1934 by Lemmel, diagnosis is based on observation of a papillary duodenal diverticulum which can cause obstructive biliary syndrome. 1 Lemmel’s syndrome is defined as obstructive jaundice in a patient for whom choledocholithiasis and other causes of biliary obstruction have been ruled out and who has a peripapillary diverticulum. The clinical picture associated with Lemmel’s syndrome can range from obstructive jaundice with abdominal pain to acute cholangitis, and can sometimes mimic periampullary tumors. 2
Due to the infrequent occurrence of the condition, there is no clarity about the pathophysiological mechanisms that lead to appearance of symptoms. Nevertheless, multiple theories have been proposed. It is believed that the appearance of diverticulitis or irritation in the direct mechanics of the periampullary diverticulum can cause chronic inflammation of the papilla. This later leads to fibrosis, a condition known as chronic fibrous papillitis. 3 Another theory is that Lemmel’s syndrome is caused by dysfunction of the sphincter of Oddi secondary to the presence of the diverticulum. 4 Recently, compression of the distal bile duct or ampulla by a periampullary diverticulum occupied by an enterolith or bezoar has been proposed as the probable etiology. 5,6 In the case of our patient, neither bezoars nor enteroliths were found within the diverticulum, but the diverticulum was found to be compressing the distal common bile duct in a manner similar to that described in the world literature. This was demonstrated by magnetic resonance cholangiography and endoscopic biliopancreatic ultrasonography. However, it is not possible to rule out the presence of a previously existing enterolith or bezoar, since the wide mouth of the diverticulum could have allowed evacuation of the diverticulum before endoscopic evaluation. This could also explain the intermittency of the patient’s symptoms which led to his rehospitalization.
Diagnosis of Lemmel’s syndrome is a real challenge since it is necessary to rule out other more prevalent etiologies first. The first step is identification of a duodenal diverticulum two to five cm from the papilla. This is usually done with a lateral view duodenoscope during ERCP. Imaging studies such as computerized axial tomography (CAT) and magnetic resonance imaging (MRI) show duodenal diverticula as thin-walled gas-filled cavitations in the wall of the second portion of the duodenum. However, when these are filled with fluid they can sometimes be confused with pseudocysts, pancreatic abscesses, metastatic adenopathies or cystic neoplasms in the head of the pancreas. 7,8 The recommendation for asymptomatic patients is to avoid all kinds of treatment while for oligosymptomatic patients, conservative management is recommended. For patients who are clearly symptomatic who have pain or cholangitis, extraction or destruction of an enterolith or bezoar might be attempted, 9,10 although it is usually enough to perform a papillotomy since most cases are secondary to chronic fibrous papillitis or sphincter of Oddi dysfunction as demonstrated in a recent case published in the Colombian Review of Gastroenterology. 11,12,13
Although Lemmel’s syndrome occurs rarely, it should be considered in all patients who present with obstructive jaundice and a periampullary diverticulum for whom other causes of obstruction have been ruled out. Management of Lemmel’s syndrome depends to a great extent on findings from imaging and endoscopy as well as on the symptoms presented by the patient. Endoscopic management is preferred because surgical options have higher morbidity and mortality rates.
Referencias
1. Lemmel G. Die Klinische Bedeutung der Duodenal Divertikel. Arch Verdauungskrht. 1934;56:59-70. doi: 10.1159/000196978. [ Links ]
2. Mallappa S, Jiao LR. Juxtapapillary duodenal diverticulum masquerading as a cystic pancreatic neoplasm. JRSM Short Rep. 2011;2(11):89. doi: 10.1258/shorts.2011.011082. [ Links ]
3. Manabe T, Yu GS. Duodenal diverticulum causing intermittent- persistent cholestasis. Associated with papillitis chronica fibrosa. N Y State J Med. 1977;77(13):2132-6. [ Links ]
4. Tomita R, Tanjoh K. Endoscopic manometry of the sphincter of Oddi in patients with Lemmel’s syndrome. Surg Today. 1998;28(3):258-61. doi: 10.1007/s005950050117. [ Links ]
5. Rouet J, Gaujoux S, Ronot M, Palazzo M, Cauchy F, Vilgrain V, et al. Lemmel’s syndrome as a rare cause of obstructive jaundice. Clin Res Hepatol Gastroenterol. 2012;36(6):628-31. doi: 10.1016/j.clinre.2012.05.002. [ Links ]
6. Nishida K, Kato M, Higashijima M, Takagi K, Akashi R. A case of Lemmel’s syndrome caused by a large diverticular enterolith at the peripapillary portion of the duodenum. Nihon Ronen Igakkai Zasshi. 1995;32(12):825-9. [ Links ]
7. Macari M, Lazarus D, Israel G, Megibow A. Duodenal diverticula mimicking cystic neoplasms of the pancreas: CT and MR imaging findings in seven patients. AJR Am J Roentgenol. 2003;180(1):195-9. doi: 10.2214/ajr.180.1.1800195. [ Links ]
8. Kim SY, Kim JN, Kwon SO, Cha IH, Ryu SH, Kim YS, et al. A case of duodenal diverticulum mimicking a peripancreatic abscess. Korean J Med, 2013;84(2):249-53. doi: 10.3904/kjm.2013.84.2.249. [ Links ]
9. Nonaka T, Inamori M, Kessoku T, Ogawa Y, Imajyo K, Yanagisawa S, et al. Acute obstructive cholangitis caused by an enterolith in a duodenal diverticulum. Endoscopy. 2010;42 Suppl 2:E204-5. doi: 10.1055/s-0030-1255704. [ Links ]
10. Yoneyama F, Miyata K, Ohta H, Takeuchi E, Yamada T, Kobayashi Y. Excision of a juxtapapillary duodenal diverticulum causing biliary obstruction: report of three cases. J Hepatobiliary Pancreat Surg. 2004;11(1):69-72.10.1007/s00534-003-0854-7. [ Links ]
11. Chiang TH, Lee YC, Chiu HM, Huang SP, Lin JT, Wang HP. Endoscopic therapeutics for patients with cholangitis caused by the juxtapapillary duodenal diverticulum. Hepatogastroenterology. 2006;53(70):501-5. [ Links ]
12. Rizwan MM, Singh H, Chandar V, Zulfiqar M, Singh V. Duodenal diverticulum and associated pancreatitis: case report with brief review of literature. World J Gastrointest Endosc. 2011;3(3):62-3. doi: 10.4253/wjge.v3.i3.62. [ Links ]
13. Lobo DN, Balfour TW, Iftikhar SY, Rowlands BJ. Periampullary diverticula and pancreaticobiliary disease. Br J Surg. 1999;86(5):588-97. doi: 10.1046/j.1365-2168.1999.01121.x. [ Links ]
Received: January 29, 2018; Accepted: June 02, 2018











 texto em
texto em 


