Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Acessos
Acessos
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares em
SciELO
Similares em
SciELO -
 Similares em Google
Similares em Google
Compartilhar
Revista colombiana de Gastroenterología
versão impressa ISSN 0120-9957versão On-line ISSN 2500-7440
Rev. colomb. Gastroenterol. vol.35 no.4 Bogotá out./dez. 2020 Epub 12-Jul-2021
https://doi.org/10.22516/25007440.408
Case report
Black esophagus as a cause of upper gastrointestinal bleeding: a case report
1Departamento de Medicina, Servicio de Gastroenterología, Hospital Cayetano Heredia. Universidad Peruana Cayetano Heredia. Lima, Perú.
Acute necrotizing esophagitis is a rare entity that affects mainly elderly patients. The most common clinical presentation is upper gastrointestinal bleeding. The prognosis depends on the underlying diseases, with a mortality of up to 50%. This is the case of a 77-year-old male patient who presented with melena, three episodes of hematemesis, and epigastric pain for a week. Upper endoscopy revealed mucosa with spotty necrosis and fibrin in the middle and distal esophagus. Esophageal biopsy was compatible with mucosal necrosis.
Keywords: Necrotizing esophagitis; Black esophagus; Acute esophageal necrosis
La esofagitis necrotizante aguda es una entidad poco común que afecta sobre todo a ancianos. La presentación clínica más común es hemorragia digestiva alta. El pronóstico depende de las enfermedades de base con una mortalidad de hasta el 50 %. Se presenta el caso de un varón de 77 años con historia de una semana de melena, 3 episodios de hematemesis y epigastralgia. La endoscopia digestiva alta reveló una mucosa con necrosis en parches y fibrina en el esófago medio y distal. La biopsia de esófago fue compatible con necrosis de mucosa.
Palabras clave: Esofagitis necrotizante; esófago negro; necrosis esofágica aguda
Introduction
Acute esophageal necrosis (AEN), also known as black esophagus, is a rare condition with few cases reported in the medical literature1-3. It mostly affects the elderly, and the most common clinical presentation is upper gastrointestinal bleeding in more than 70 % of cases1-3. Its pathophysiology is unknown; however, AEN cases secondary to ischemic involvement, malnutrition, and obstruction of the upper digestive tract have been described4. Endoscopic findings show a blackish discoloration of the esophageal mucosa ending at the level of the gastroesophageal junction. Prognosis depends on underlying diseases, with a mortality rate of up to 50%2,4.
Clinical case
This is the case of a 77-year-old male with a 1-week history of melena, 3 episodes of hematemesis and epigastric pain. The patient had a history of ischemic stroke and reported he had high blood pressure and used aspirins daily. Upon admission, he was hypotensive and the only relevant finding on physical examination was a mild left hemiparesis due to his history of stroke. Additional tests showed mild anemia, leukocytosis, hypoalbuminemia, and impaired renal function (hemoglobin: 12.4 mg/dL; leukocytes: 18 000, urea: 141, creatinine: 1.9 and albumin: 2.5). No alterations were reported in the coagulation profile and liver function tests. In addition, a chest X-ray showed a widened mediastinum and gave the impression of pneumomediastinum; however, this condition was ruled out after performing a thoracic CT scan.
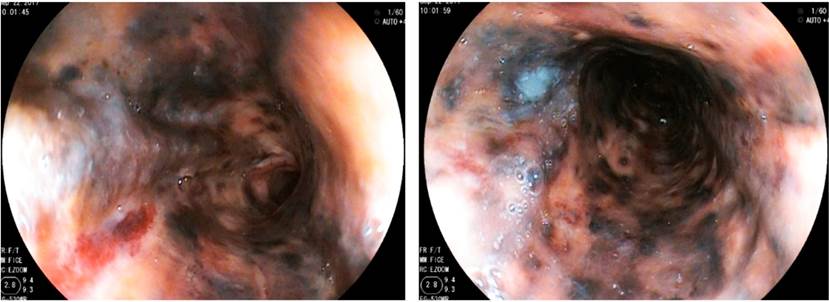
Upper gastrointestinal endoscopy revealed mucosa with patchy necrosis and fibrin in the lower half of the esophagus (Figure 1).
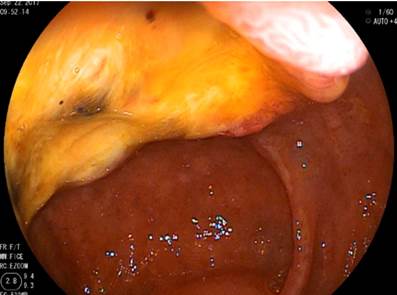
In addition, two ulcers were observed in the second portion of the duodenum measuring 30x25 and 20x20 mm with a fibrin base (Figure 2). The esophageal biopsy was compatible with mucosal necrosis.
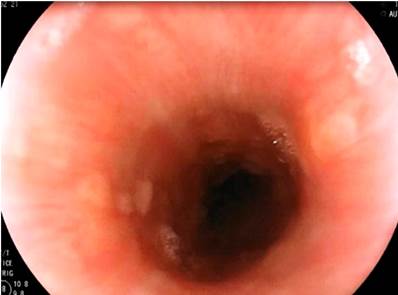
The patient was treated with intravenous fluids, gastric rest for 72 hours, parenteral proton-pump inhibitors, antiemetics and sucralfate. His clinical progress was favorable. Regeneration of the esophageal mucosa was observed after 5 days (Figure 3). At 6 weeks, he experienced esophageal dysphagia, so the endoscopic study was repeated, and a 20 cm esophageal stricture from the dental arch preventing the passage of the equipment was identified (Figure 4). He underwent 2 sessions of balloon dilatation, experiencing an improvement in relation to his symptoms.
Discussion
AEN was first described in 1967 by Brennan during a necropsy, and it was later described it in 1990 by Goldenberg during an endoscopy3. Its incidence in endoscopic studies is less than 0.3 % and contrasts with the 10.3 % described in autopsies5.
Since the distal esophagus is the least vascularized portion of the esophagus, necrosis is usually circumferential. Furthermore, it normally ends abruptly at the gastroesophageal junction3,5. AEN pathophysiological processes include hypoperfusion, a weakened gastric mucosal barrier, and the presence of gastroesophageal reflux4-6.
Its etiology is multifactorial and is described in patients with risk factors for ischemia and low blood flows. It occurs more frequently in men, especially in the elderly, and it is associated with thromboembolic events and malignancy7,8. The patient reported in this case is an elderly man with hypertension and a history of a stroke as predisposing factors.
Upper gastrointestinal bleeding, as in this case, is the most common clinical presentation of this condition9. Other symptoms such as epigastralgia, emesis, dysphagia, and fever have also been reported8,9.
Endoscopy is the test of choice for diagnosis purposes, which is also based on the medical history of the patient, biopsies are not indispensable and must be performed with caution because of the risk of perforation5-9. Necrotic tissue is observed in pathology reports7. Differential diagnoses include melanosis, pseudomelanosis, malignant melanoma, acanthosis nigricans, charcoal deposits, caustic ingestion, and infections5.
Duodenal bulb ulcers, erosions, and inflammation commonly seen in these patients are caused by vascular involvement of the branches of the celiac trunk, which supply common blood to the distal esophageal and duodenal tissue2.
Treatment includes hemodynamic support, proton-pump inhibitors, and management of comorbidities, which affect prognosis1,6. Bowel rest is recommended in the first 24-48 hours. The use of a nasogastric tube is recommended if there is concomitant bowel obstruction or persistent vomiting1,6. High-dose omeprazole is recommended, and sucralfate is used as a cytoprotector of the esophageal mucosa once tolerance to the oral route has been established3,4. When endoscopy is repeated 48-72 hours later, esophageal mucosal regeneration is normally visible1. In our case, the endoscopic study was repeated after 5 days and regeneration was verified.
Serious immediate complications include esophageal perforation and sepsis7. Mediastinitis and mediastinal abscesses due to esophageal rupture secondary to transmural involvement are rare6,8-10. Esophageal stricture is the most frequent late complication and occurs in 15% of AEN cases2,4. In the case reported here, the patient presented esophageal dysphagia 6 weeks after the event and esophageal stricture was verified by barium esophagogram and a new endoscopic study. The patient experienced an improvement in relation to its symptoms after two balloon dilatation sessions.
AEN is a rare serious disease and should be included in the list of differential diagnoses in elderly patients with multiple comorbidities and upper gastrointestinal bleeding. Its diagnosis requires a high suspicion rate in elderly people with poor general condition and some associated predisposing factors5,6.
REFERENCES
1. Ramírez-Quintero JD, Bernal-Sierra E, Gómez-Rueda NV. Necrosis esofágica aguda, esófago negro: reporte de un caso. IATREIA. 2016;29(4):493-7. https://doi.org/10.17533/udea.iatreia.v29n4a11 [ Links ]
2. Del Hierro PM. Acute Necrotizing Esophagitis Followed by Duodenal Necrosis. Gastroenterology Res. 2011;4(6):286-288. https://doi.org/10.4021/gr361w [ Links ]
3. Wallberg ME, Young P, Finn BC, Thomé M, Chueco AA, Villarejo F. Black esophagus due to acute necrotizing esophagitis: Report of one case. Rev Méd Chile. 2009;137(5):672-4. https://doi.org/10.4067/S0034-98872009000500011 [ Links ]
4. Gómez JL, Barrio J, Atienza R, Fernández-Orcajo P, Mata L, Saracíbar E, de la Serna C, Gil-Simón P, Vallecillo MA, Caro Patón A. Acute esophageal necrosis: An underdiagnosed disease. Rev Esp Enferm Dig. 2008;100(11):701-705. https://doi.org/10.4321/S1130-01082008001100006 [ Links ]
5. Galtés I, Gallego MA, Esgueva R, Martin-Fumadó C. Necrosis esofágica aguda (esófago negro). Rev Esp Enferm Dig . 2016;108(3):154-155. [ Links ]
6. Gómez AA, Guerrero D, Hani AC, Cañadas R. Esofagitis necrotizante aguda (esófago negro) con estenosis compleja secundaria. Rev Gastroenterol Perú. 2015;35(4):349-54. [ Links ]
7. Pineda Oliva OJ, Valencia Romero A, Valdivia Balbuena M, Soto Pérez JC, Díaz Oyola M, Cuevas Osorio V, Farell Rivas J, Gonzalez Villarello M, Lopez Acevedo H, Llamas Ceras ML, Paredes Mendoza BR, Toledo A. Esófago negro: reporte de un caso. Endoscopia. 2014;26(4):136-139. https://doi.org/10.1016/j.endomx.2014.10.002 [ Links ]
8. Day A, Sayegh M. Acute oesophageal necrosis: a case report and review of the literature. Int J Surg. 2010;8(1):6-14. https://doi.org/10.1016/j.ijsu.2009.09.014 [ Links ]
9. Gurvits GE. Black esophagus: acute esophageal necrosis syndrome. World J Gastroenterol. 2010;16(26):3219-25. https://doi.org/10.3748/wjg.v16.i26.3219 [ Links ]
10. Worrell SG, Oh DS, Greene CL, DeMeester SR, Hagen JA. Acute esophageal necrosis: a case series and long-term follow-up. Ann Thorac Surg. 2014;98(1):341-2. https://doi.org/10.1016/j.athoracsur.2013.09.023 [ Links ]
Citation: Carlin A, Bellido A, Gómez P, Valenzuela V, Pinto JL. Black esophagus as a cause of upper gastrointestinal bleeding: a case report. Rev Colomb Gastroenterol. 2020;35(4):533-536. https://doi.org/10.22516/25007440.408
Received: May 16, 2019; Accepted: August 04, 2019











 texto em
texto em