Introduction
Esophagogastroduodenoscopy (EGD) serves as a pivotal diagnostic and therapeutic tool for various upper gastrointestinal tract disorders. It plays an essential role in the educational foundation and training of gastroenterology fellows, emphasizing the cultivation of skills necessary for its safe, effective, and efficient execution with thorough technical proficiency1,2.
This involves nurturing both cognitive and psychomotor abilities, alongside temporal-spatial correlation skills, which are applied to three-dimensional spaces for examination or intervention3. Currently, a standardized methodology for EGD training is absent, leading to significant variability across adopted educational frameworks1,2,4.
The conventional training model is built around two core principles: the first advocates for observing procedures performed by experts, engaging in supervised practice, and subsequently gaining experience, encapsulated by the “see, do, and teach” mantra2,4. Although this approach has merits, it has also introduced challenges in learning customization and the depth of knowledge acquired3. The second principle focuses on the volume of EGD procedures as a metric for procedural proficiency, yet this is subject to debate among scientific societies over the optimal procedure count, highlighting that such metrics serve merely as benchmarks rather than guarantees of comprehensive learning1,2,4. This method of instruction should not be perceived as deficient; rather, both principles are seen as mutually enriching.
It is advocated that the EGD training regimen should be meticulously structured and evaluated at each stage to ensure superior quality and safety, urging a collective effort towards the establishment of a standardized protocol1. In response, there is a movement towards integrating alternative educational strategies, such as skill-based pedagogy. This approach leverages didactic and cognitive resources combined with practical instruction3, aiming to foster competencies, namely a foundational level of knowledge, skill, and experience derived from training, alongside the essential ability to perform interventions with confidence and effectiveness3. This methodology promotes individualized learning trajectories, acknowledging the variability in learning styles and speeds among students5.
A proposed strategy to enhance training frameworks and align them with the expectations of new generations of gastroenterologists includes the adoption of innovative approaches inspired by educational theory, incorporating online learning, digital technologies, and social networking tools2,6. This leads to the recommendation of conducting a review that delves into the core aspects of learning, offering an integrated approach to maximize the efficacy of the EGD training process.
Traditional approaches to esophagogastroduodenoscopy education
The educational methods for instructing fellows in the performance of EGD exhibit a considerable range of variability4. Historically, endoscopy education has taken place within the clinical setting, primarily relying on a mimicry-based learning system. This approach posits that hands-on patient experience is paramount, as it allows for direct engagement with procedures in the “real world”1,2. However, this traditional model is inherently flawed due to its lack of standardization, potentially leading to poor decision-making and the formation of inappropriate practices1. Additional limitations include extended duration of procedures, dependency on a patient population willing to undergo procedures by students, and an increased risk to patient safety1. These concerns underscore the significance of incorporating observation phases into the EGD training, preceding any hands-on patient experiences.
Within this traditional framework, the transfer of knowledge occurs as educators relay their expertise. Yet, it is critical to acknowledge that not all endoscopists are equipped with teaching skills, and extensive experience does not automatically equate to effective instructional capabilities2. To address these gaps, a variety of methodologies have been proposed to enhance the learning process. Among these is an active learning approach, emphasizing competency-based education-a model that shifts focus from the educator to the learner, aligning with adult learning principles7. This strategy advocates for a move from mimicry-based to competency-focused learning, tailored to the individual’s intrinsic attributes, prior knowledge and experience, exposure to varying pathologies, and access to resources3.
Training objectives in endoscopic procedures
The core objectives of endoscopic procedure training encompass both the acquisition of theoretical knowledge and the honing of technical skills. Despite being a generally safe practice, the inherent risk of complications necessitates the ability to perform procedures with high quality and minimal patient risk1. These objectives constitute fundamental pillars for training programs in digestive endoscopy, as the proficient and secure execution of EGD, coupled with an adept mastery of the technique, stands as a central goal for fellows in gastroenterology during their training trajectory2.
Historically, the objective assessment of skill acquisition in endoscopic procedural training has been delineated by a prescribed minimum quantity of procedures, theoretically culminating in technical mastery1,2,4. However, inherent and cultivated skill disparities amongst students engender an asymmetrical progression in this process3. The attainment of requisite competencies upon the culmination of the training process is defined by the American Society for Gastrointestinal Endoscopy (ASGE) as the “minimal level of skills, knowledge, or expertise derived from training and experience that is necessary to execute a procedure safely and competently”4.
While these mandated minimal standards in procedural volume are pertinent, they emanate from expert consensus or the deliberations of prominent scientific societies and should merely serve as guidelines, given that they do not ensure competence acquisition, which can vary contingent upon the assessed skill (both technical and cognitive)2,8. Thus, this parameter ought to be construed as a surrogate for competency attainment, coalescing with milestone evaluations, endoscopic findings interpretation, and their integration into holistic patient care2,8.
Traditionally, the requisites for conducting endoscopic procedures have been dichotomized into two fundamental skill domains: technical and cognitive, crucial for furnishing quality care. Nonetheless, these are deemed inadequate, prompting the emergence of integrative skills, deemed indispensable and recognized for their role in mitigating the risk of adverse events, as deficiencies in behavior and communication may yield a greater propensity for errors when juxtaposed against technical knowledge deficits9.
A lucid comprehension of the minimal competencies requisite for executing high-quality endoscopic procedures is imperative for delineating an evaluative framework. It necessitates conceptualization within the purview of three cardinal competency domains: technical, cognitive, and integrative, with the primary domains expounded upon in Figure 1 9.
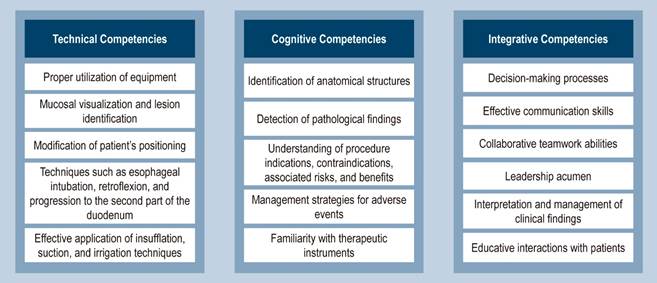
Figure 1 Core Competency Domains. Adapted from: Walsh CM. Best Pract Res Clin Gastroenterol. 2016;30(3):357-3749.
The role of simulation in EGD educational and learning processes
In the realm of medical education, simulation-based learning caters specifically to adult education, utilizing audiovisual aids, such as multimedia and clinical case resolution, along with technological tools4.
The introduction of simulation models before patient engagement, coupled with the systematic approach to EGD instruction and learning in clinical phases, serves a supplementary function. This approach contributes to mitigating the risks or unwarranted discomfort that patients might otherwise endure10; it also allows fellows to concentrate on mastering technical skills, expedite the learning trajectory, and assimilate various requisite skills for procedural execution, encompassing technical, cognitive, methodological, and communicative abilities2. Furthermore, simulation aids in the assessment of integrative competencies like communication and teamwork9, and it provides a structured platform for the diversification of clinical scenarios11.
The advantages of simulation-based training for EGD are most pronounced when employed early in the training sequence. However, these benefits diminish after the completion of about 50 EGD procedures12. An array of simulators exists, including mechanical models featuring obstacles and tasks of differing complexities, live animals, ex vivo organs from animal cadavers, and virtual simulators13. These simulators have been effective in enhancing skill acquisition for colonoscopies and the execution of hemostatic procedures, though the consistency of these outcomes across various studies remains debatable. Furthermore, the definitive impact on clinical practice, patient safety, and the health care cost-benefit analysis is yet to be fully established1. Notwithstanding this limitation, initiating any potentially risky learning process with simulation is considered prudent1.
The ASGE, in 2012, underscored the importance of embracing simulation, stressing two pivotal considerations: first, simulation has the potential to reduce by 25% the number of cases that trainee gastroenterologists must undertake to achieve essential EGD competencies; second, performance metrics derived from simulation activities can exhibit a correlation with actual minimum competency standards (kappa of 0.7 or higher)14. Despite the clear benefits, the efficacy of simulation-based education is not universally acknowledged. Its utility diminishes, for instance, when conducted in the absence of feedback from instructors, signifying that its integration into training programs must be deliberate, reflective10, and evidence-based to optimize the learning benefits while justifying the related expenses10.
As detailed in the review by Khan and colleagues10, simulation-based education centers on four principal practices, delineated in Figure 2. In conclusion, incorporating a blended training model that includes observation, clinical practice, and simulation represents the optimal strategy for learning the intricacies of performing an EGD2.
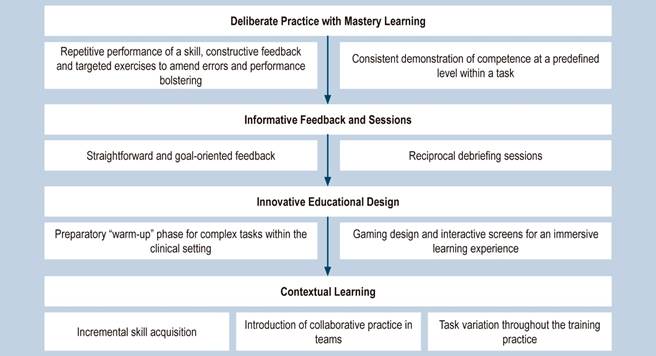
Figure 2 Simulation-Based Education. Adapted from: Khan R, et al. World J Gastrointest Endosc. 2019;11(3):209-21810.
Recommendations from international scientific societies
Building upon the aforementioned premise concerning the significance of both the quantity of endoscopic procedures conducted and the acquisition of competencies, there exists variability in the recommendations provided by various scientific societies in gastroenterology and digestive endoscopy regarding the “optimal” quantity of procedures necessary to fulfill minimum requirements and attain requisite skills1,2. Table 1 delineates the extant guidelines.
Table 1 Required Number of EGD Procedures for Skills Acquisition as Recommended by Various Scientific Societies
| Organization | Number of EGDs |
|---|---|
| American Society for Gastrointestinal Endoscopy | 130 |
| British Society of Gastroenterology | 300 |
| European Union of Medical Specialists | 300 |
| Korean Society of Gastrointestinal Endoscopy | 1000 |
| Gastroenterological Society of Australia | 200 |
Adapted from: Kim JS, et al. Clin Endosc. 2017;50(4):318-3212.
How to evaluate performance?
The role of evaluation transcends merely cataloging what has been learned; it should also act as a catalyst for transformation, serving as a critical source of feedback for educators, programs, and students alike. This evaluative process aims to gauge the effectiveness of educational initiatives, pinpointing strengths and identifying weaknesses among all involved parties, thus paving the way for dynamic, progressive, and systematic enhancements that align with established learning objectives3.
Furthermore, evaluation constitutes a key component of the instructional process across various disciplines. To execute this, a diversity of models or strategic approaches may be employed. When these are applied in a complementary manner to an individual student, they afford a more nuanced appreciation of their skillset and highlight areas ripe for improvement15. Integral to this assortment is Miller’s model, which delineates a structure for appraising competency-based education, presuming predictive capability for performance across four dimensions: “knows”, “knows how”, “shows how,” and “does”15. However, while offering a comprehensive framework for evaluation, it does not account for the interplay between performance and competence, prompting the introduction of the Cambridge model, which contemplates the impacts of systemic and individual influences15.
Conclusions
Competence assessment must be an integral element of the training regime for gastroenterology fellows, not limited to considering the quantitative metrics of procedures performed. While these figures hold significance, they should not be the sole determinant of competence.
The pedagogy of EGD should be inherently motivating rather than punitive for fellows, offering educators a dynamic platform to disseminate their expertise in an engaging and interactive fashion.
Acknowledging that each student assimilates skills (technical, cognitive, and integrative) at their own pace, personalized guidance and constructive feedback become indispensable.
We stand before a generation characterized by learning styles distinct from traditional norms, necessitating continual professional development and instructional renewal for endoscopists who teach. Embracing a multifaceted training strategy that blends observation, clinical practice, and simulation emerges as the optimal pathway for mastering both diagnostic and therapeutic EGD, potentially hastening the progression of learning trajectories.











 texto em
texto em 



