Remark
| 1) Why was this study conducted? |
| The country needs data with international standards on the behavior of the risk of develop cancer and dying from cancer. Population-based cancer registries offer reliable estimates of cancer incidence and mortality and their behavior over time. |
| 2) What were the most relevant results of the study? |
| Incidence and mortality decreased in women, due to a significant decrease in cervical, stomach, and lung cancers. In men, both incidence and mortality remained stable. |
| 3) What do these results contribute? |
| Progress in the fight against cancer is still discrete and has been concentrated mainly in women, which makes it imperative to strengthen a differential approach by sex when planning strategies for cancer control. It is necessary to extend surveillance over a longer period of time to obtain more stable estimates of trends. |
Introduction
Cancer is one of the leading causes of morbidity and mortality worldwide 1. Cancer incidence has increased considerably in most countries 2, and is projected to increase 47% by the year 2040, taking 2020 as the baseline 1. Cancer causes a high mortality rate yearly, particularly in low- and middle-income countries. Also, deaths in these countries are expected to increase as a result of aging populations and declines in deaths from other causes 3.
The burden of cancer represents an important challenge for Latin American countries, including Colombia, which face an increase in incidence and mortality 4, in the context of insufficient population-level interventions to control this disease 5. In this sense, population-based cancer registries (PCRs) are fundamental inputs for designing cancer control strategies; PCRs allow the monitoring and evaluating the event over time in geographically defined populations 6. In Colombia, progress has recently been made in the quality of the PCRs, as evidenced by the inclusion of the PCRs of Bucaramanga, Cali, Manizales and Pasto in the most recent volume of Cancer Incidence in Five Continents (CI5-XI) 7,8. Based on the information provided by the RPCs, it has been established, for example, that prostate, breast, stomach and cervical cancers are responsible for more than 50% of the burden of this disease in Colombia 9.
The Population-Based Cancer Registry of Manizales (PCRM) has operated since 2002, generating comparable, reliable and valid information on the epidemiological behavior of cancer in the city 10. Thus, in Manizales, patterns of incidence and mortality of cancer for the five years of 2003-2007 have been previously analyzed 11, and a general incidence rate lower than that estimated for Colombia and a mortality rate higher than the national estimate stand out. In analyzing these rates, one element that has acquired relevance is the evaluation of changes in their trends 12. This allows, among other things, to identify priority areas for intervention and evaluate the impact of cancer control programs.
It is necessary to analyze the cancer situation in Manizales with updated data and complementary statistical methods. This research aimed to describe trends in cancer incidence and mortality in Manizales between 2008 and 2017, based on data from the ' 'city's PCR.
Materials and Methods
Type of study
A population-based descriptive study on trends in cancer incidence and mortality in Manizales, Colombia, from 2008-2017.
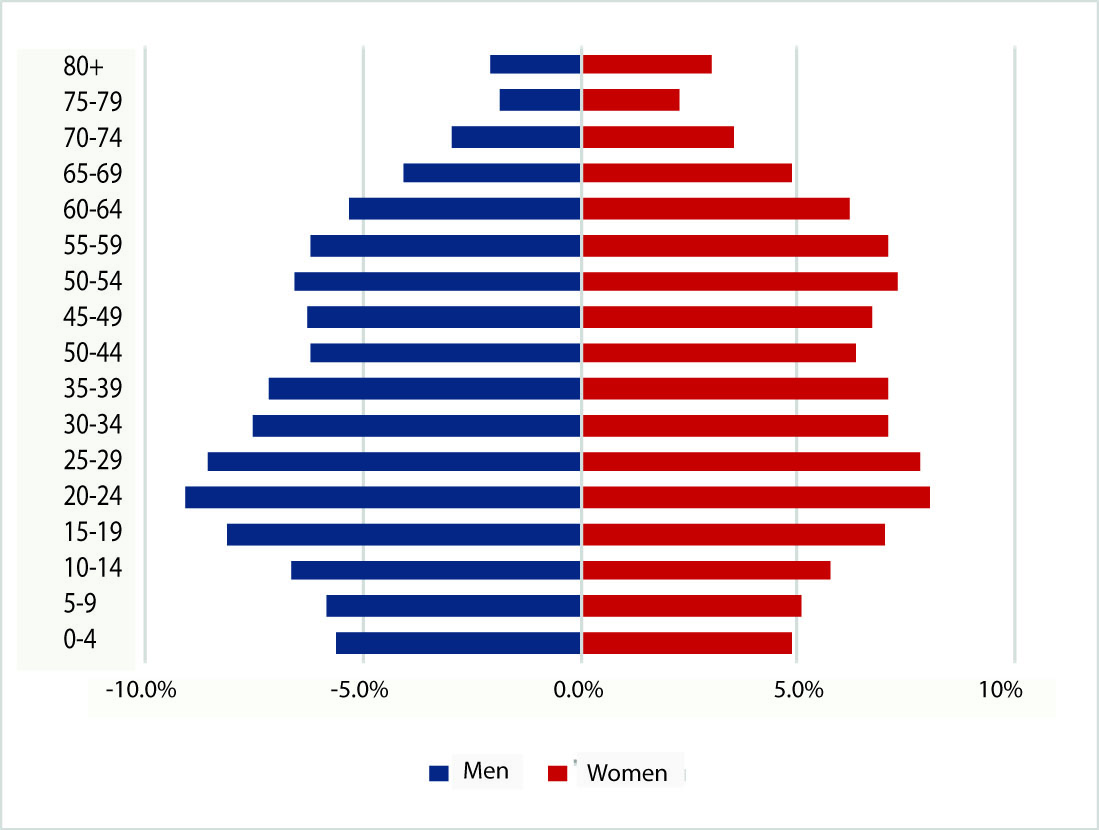
The PCRM covers the urban and rural areas of Manizales. The city has 434,403 inhabitants, according to the 2018 National Population and Housing Census (CNPV) 13. The population structure of Manizales is of regressive type (Figure 1), with an aging index of 79 older adults for every 100 children under 15 years old 14.
Case definition
The incident cases recorded to correspond to primary malignant tumors in all anatomical sites. Primary cancer is defined as cancer originating from a tissue or organ that does not correspond to extension, recurrence, or metastasis of another primary tumor. Basal cell tumors of the skin, tumors of uncertain or unknown behavior (defined according to the International Classification of Diseases for Oncology - 3rd edition, ICD-O3 15) are not included. Since 2013, benign tumors of the central nervous system (CNS) and tumors of uncertain behavior of the urinary tract were included. The unit of analysis of the Registry is the tumor, not the patient.
Data extraction
The PCRM actively searches for new cases in the city's health institutions through direct consultation of medical records and review of electronic databases of pathology laboratories, imaging centers, clinics, hospitals, and outpatient centers. Data capture is performed by trained personnel, and information on each case is consolidated from all available sources of information. The municipal health authority periodically provides data on cancer deaths in the city, which is an additional source for identifying incident cases from death certificates.
Case classification and coding
The PCRM collects information on patient and tumor variables according to the rules of the International Agency for Research on Cancer (IARC) (16). Topographical and morphological coding followed ICD-O3 rules 16. The database was reviewed according to the quality assessment procedures usually applied to PCRs by IARC. All cases reported as inconsistent were reviewed in the data sources and the pertinent corrections and confirmations were made. Cases obtained through hospital discharge and death certificate were verified through medical records when possible. Cases reported by death certificate for which no other source of information could be found were included as cases detected by death certificate only (DCO). These procedures are similar to those applied by other PCRs in Colombia and in the world 16.
Data quality criteria
The PCRM applies standardized procedures for data quality validation using the IARC/IACR Cancer Registry Tools10. For the most frequent locations, the percentages of morphological verification, DCO cases and cases with unknown age, and the mortality-incidence ratio were calculated. Regarding mortality, in Manizales, death certification coverage is considered exhaustive (~99%), all deaths are certified by physicians, and the accuracy of certification is 96.4% for all deaths and 93.2% for cancer deaths 17.
Incidence and mortality estimates
For incidence estimates, all new cancer cases that occurred in people residing in Manizales between January 1, 2008 and December 31, 2017, were considered; new case collection was expanded for the period 2008-2012, and additional DCO cases were included through vital statistics databases recently provided by the local health authority that were not available in previous years.
For mortality, all deaths that occurred during the same period with ICD-10 codes corresponding to malignant neoplasia were included, according to the databases published by the National Administrative Department of Statistics (DANE, by its acronym in Spanish) 18; cases residing abroad, cases without age information, and cases without sex information were excluded.
For calculating the denominators (population at risk), Manizales age- and sex-specific population per year was obtained from DANE population estimates databases based on the CNPV 2018 19, collapsing the data into 18 five-year age groups up to 85 years and older, and by sex. Specific incidence and mortality rates were estimated by sex, age (18 quinquennial groups) and cancer site, and standardized using the direct method, using the SEGI world standard population as reference. Rates were expressed per 100,000 person-years. Age-standardized rates were corrected for cases of unknown age according to procedures defined by IARC C 8. In addition, incidence and mortality data were grouped and analyzed according to ICD-O3 topographic codes (or standardized ICD-10 codes) for comparability purposes. Statistical analysis was performed in Stata 14.2® (StataCorp, College Station, Texas, USA).
Trends
Trends in incidence and mortality rates were analyzed by sex and cancer site for the period 2008-2017 using the U.S. National Cancer ' 'Institute's publicly accessible Joinpoint Regression Program, Version 4.9.0.0 15. This non-linear regression model assesses trends changes by fitting a series of joined lines to age-standardized rates. The Program determines the optimal number of joinpoints through a grid search method and establishes significance with a Monte Carlo permutation test. Trends are described as increasing or decreasing when the annual percentage change (APC) for the specified period is statistically significant (p-value <0.05); otherwise, the APC is described as stable. The APC represents the average percentage increase or decreases in cancer rates per year over a specified period, in this case, 2008-2017.
Results
Incidence and mortality by all cancer sites
A total of 11,188 incident cases were recorded, 56.7% (n= 6,348) in women. The median age at diagnosis was 66 years (IQR= 19 years) for men and 61 years (IQR= 23 years) for women. 0.8% of cases occurred in the pediatric population (under 15 years of age). Figure 2 summarizes the incidence rates and the distribution of cases by age group in men and women; as expected, it was observed that the older the age, the greater the cancer burden. It is noteworthy that in women,, the incidence rises at an earlier age than in men.
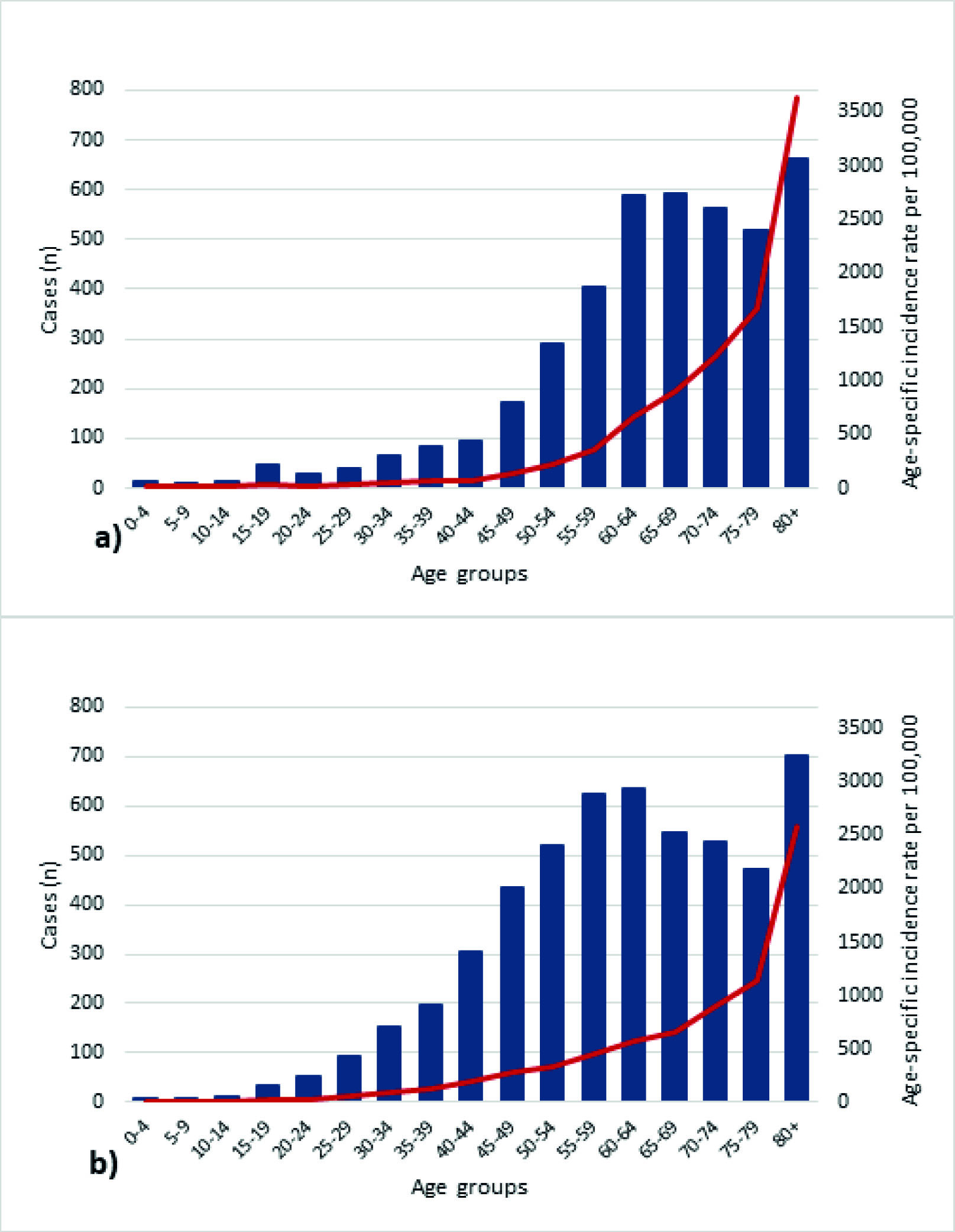
Figure 2 Cancer incidence rates and distribution of cases by age groups in (a) men and (b) women, Manizales, 2008-2017. Blue columns represent the number of cases, and red lines represent age-specific incidence rates. Note: cases with unknown ages were excluded from the graph.
For the five-year period 2008-2012, there were 2,186 (41.6%) and 3,072 (58.4%) new cases in men and women, respectively. Between 2013 and 2017, 3,276 (55.2%) new cases occurred in women and 2,654 (44.8%) in men. The age-standardized incidence rate in both periods was slightly higher in females, with male-to-female incidence rate ratios of 0.89 (95% CI= 0.867-0.914) and 0.99 (95% CI= 0.985-0.995) for the five-year periods 2008-2012 and 2013-2017, respectively
Regarding mortality, between January 1, 2008, and December 31, 2017, 4,996 cancer deaths occurred in people residing in Manizales, 52.6% (n= 2,628), 2,260 in women in the first five-year period, and 2,736 in the second. During the five years 2008-2012, there were 1,219 deaths (53.9%) from cancer in women and 1,041 (46.1%) in men. Between 2013 and 2017, the sex distribution was 1,409 (51.5%) and 1,327 (48.5%) deaths in women and men, respectively. Of all deaths during the decade, 0.9% occurred in children under 15.
Quality indicators
Table 1 presents the quality indicators for the five main locations by sex and period of diagnosis. For 2008-2012, we reviewed data from sources that were not accessible in previous years, particularly official data on deaths, which were only accessible in 2021; therefore, the percentages of DCO cases and cases with microscopic verification and unknown age are suboptimal. Nevertheless, the indicators for the most recent period are comparable to those presented for the period 2003-2007. In neither period were there cases with unknown sex or unknown diagnostic basis.
Table 1 Quality indicators by period and sex for the five most common cancers in Manizales
| Site | 2008-2012 | 2013-2017 | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| n | MV | DCO | M:I | UA | n | MV | DCO | M:I | UA | |
| Men | ||||||||||
| Prostate | 504 | 80.6 | 11.5 | 0.19 | 8.7 | 662 | 83.7 | 8.3 | 0.20 | 3.8 |
| Stomach | 290 | 62.1 | 29.7 | 0.63 | 26.2 | 284 | 78.5 | 14.4 | 0.77 | 2.1 |
| Lung | 189 | 39.7 | 50.3 | 0.76 | 44.4 | 218 | 53.7 | 35.3 | 1.05 | 1.4 |
| Colon | 125 | 61.6 | 28.8 | 0.54 | 27.2 | 133 | 84.2 | 5.3 | 0.55 | 6.0 |
| NHL | 89 | 83.1 | 16.9 | 0.41 | 16.9 | 92 | 93.5 | 6.5 | 0.52 | 10.9 |
| All | 2,186 | 66.9 | 25.1 | 0.46 | 22.4 | 2,654 | 77.4 | 13.5 | 0.48 | 4.9 |
| Women | ||||||||||
| Breast | 594 | 72.2 | 18.4 | 0.24 | 17.3 | 701 | 91.2 | 3.1 | 0.24 | 1.9 |
| Thyroid | 302 | 79.8 | 5.3 | 0.04 | 5.0 | 412 | 91.7 | 1.7 | 0.05 | 12.4 |
| Cervix | 273 | 70.0 | 19.4 | 0.34 | 17.9 | 174 | 74.7 | 9.2 | 0.41 | 6.3 |
| Stomach | 222 | 49.1 | 41.0 | 0.52 | 38.7 | 191 | 81.7 | 12.0 | 0.54 | 2.6 |
| Colon | 194 | 60.3 | 33.0 | 0.47 | 29.4 | 190 | 80.5 | 14.2 | 0.65 | 2.1 |
| All | 3,072 | 62.8 | 28.3 | 0.38 | 26.2 | 3,276 | 80.6 | 10.7 | 0.40 | 5.3 |
MV=Proportion of microscopically verified cases. DCO=Proportion of death certificate only cases. M:I=Mortality-to-incidence ratio. UA=Proportion of unknown age cases. NHL=Non-Hodgkin lymphoma
Incidence and mortality by specific cancer sites
Tables 2 and 3 present the age-standardized incidence and mortality rates with their respective 95% confidence intervals for the topographical groupings suggested by IARC. These tables also include the time trend analyses summarized as APCs during the ten years analyzed. Malignant neoplasms in breast, prostate, stomach, thyroid, lung and colon, accounting for 50% of all cancer cases in Manizales between 2008 and 2017.
Table 2 Incidence rates and trends by sex, period and cancer site. Manizales, 2008-2017.
| ICD-10 | Site | Age-standardized incidence rate (100,000 person-years) | Trends in incidence rates | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 2008-2012 | 2013-2017 | 2008-2017 | |||||||||||||
| Men | Women | Men | Women | Men | Women | ||||||||||
| ASR | 95% CI | ASR | 95% CI | ASR | 95% CI | ASR | 95% CI | APC | 95% CI | APC | 95% CI | ||||
| C00-C14 | Mouth and pharynx | 2.4 | 1.4-3.4 | 2.6 | 1.8-3.5 | 3.7 | 2.7-4.7 | 1.6 | 0.9-2.2 | 7.0 | -4.9 | 20.5 | -9.2 | -17.3 | -0.2 |
| C15 | Esophagus | 3.3 | 2.1-4.5 | 2.2 | 1.4-3.1 | 2.3 | 1.5-3.1 | 1.4 | 0.8-2.0 | -8.6 | -15.6 | -1.0 | -7.1 | -14.1 | 0.6 |
| C16 | Stomach | 24.8 | 21.4-28.2 | 15.2 | 12.6-17.8 | 20.4 | 18.0-22.9 | 9.9 | 8.4-11.3 | -3.9 | -8.0 | 0.4 | -7.9 | -11.0 | -4.7 |
| C17 | Small intestine | 0.8 | 0.3-1.3 | 0.6 | 0.3-1.0 | 0.8 | 0.3-1.3 | 1.1 | 0.5-1.7 | ~ | ~ | ~ | ~ | ~ | ~ |
| C18 | Colon | 10.6 | 8.4-12.8 | 13.0 | 10.8-15.3 | 9.7 | 8.0-11.4 | 10.3 | 8.8-11.8 | -1.8 | -6.1 | 2.6 | -2.5 | -7.1 | 2.3 |
| C19-C20 | Rectum | 6.2 | 4.7-7.8 | 5.2 | 3.9-6.5 | 5.9 | 4.6-7.3 | 5.0 | 3.9-6.1 | 2.7 | -4.5 | 10.4 | -1.4 | -9.2 | 7.1 |
| C21 | Anus | 0.6 | 0.2-1.0 | 1.1 | 0.5-1.6 | 1.2 | 0.6-1.8 | 0.8 | 0.4-1.2 | 7.8 | -11.7 | 31.6 | -2.9 | -20.5 | 18.6 |
| C22 | Liver | 4.0 | 2.0-6.0 | 3.9 | 1.8-6.1 | 2.8 | 1.8-3.7 | 2.2 | 1.5-2.9 | -1.9 | -10.0 | 6.8 | ~ | ~ | ~ |
| C23-C24 | Gallbladder | 2.2 | 0.9-3.5 | 5.1 | 3.6-6.5 | 3.0 | 2.1-4.0 | 3.3 | 2.5-4.1 | 4.3 | -7.4 | 17.4 | -8.2 | -14.0 | -2.1 |
| C25 | Pancreas | 3.1 | 1.9-4.4 | 4.5 | 3.0-6.1 | 3.8 | 2.8-4.8 | 3.8 | 2.8-4.7 | 9.4 | -5.4 | 26.5 | -1.5 | -13.7 | 12.5 |
| † | Unspecified | 8.9 | 6.6-11.2 | 8.8 | 6.8-10.8 | 10.3 | 8.5-12.1 | 8.6 | 7.2-10.0 | 0.9 | -4.9 | 7.0 | -3.7 | -10.9 | 4.1 |
| C30-C31 | Nose and ear | 0.3 | 0.0-0.6 | 0.3 | 0.0-0.5 | 0.3 | 0.0-0.6 | 0.1 | 0.0-0.2 | ~ | ~ | ~ | ~ | ~ | ~ |
| C32 | Larynx | 4.1 | 2.7-5.4 | 1.3 | 0.6-2.0 | 2.1 | 1.3-2.9 | 0.7 | 0.2-1.1 | -12.0 | -20.1 | -3.2 | -10.3 | -23.6 | 5.2 |
| C33-C34 | Lung | 16.7 | 13.5-20.0 | 11.7 | 9.2-14.1 | 14.7 | 12.7-16.7 | 7.3 | 6.0-8.6 | -2.2 | -5.9 | 1.7 | -8.6 | -13.0 | -4.1 |
| C37-C38 | Other thoracic org. | 0.4 | 0.0-0.8 | 0.7 | 0.0-1.4 | 0.8 | 0.3-1.2 | 0.5 | 0.2-0.8 | ~ | ~ | ~ | ~ | ~ | ~ |
| C40-C41 | Bone | 1.7 | 0.6-2.8 | 0.9 | 0.2-1.5 | 1.6 | 0.9-2.4 | 0.9 | 0.3-1.5 | ~ | ~ | ~ | ~ | ~ | ~ |
| C43 | Melanoma | 2.1 | 1.1-3.0 | 2.5 | 1.6-3.4 | 0.6 | 0.2-1.0 | 0.7 | 0.3-1.1 | ~ | ~ | ~ | ~ | ~ | ~ |
| C44 | Skin non-melanoma | 7.4 | 5.8-9.0 | 6.0 | 4.7-7.3 | 12.0 | 10.0-14.0 | 8.7 | 7.2-10.2 | 6.4 | -2.4 | 16.0 | 3.8 | -4.5 | 12.7 |
| C45 | Mesothelioma | 0.1 | 0.0-0.2 | 0.2 | 0.0-0.4 | 0.1 | 0.0-0.2 | 0.4 | 0.1-0.7 | ~ | ~ | ~ | ~ | ~ | ~ |
| C46 | Kaposi sarcoma | 0.4 | 0.0-0.8 | 0.1 | 0.0-0.2 | 0.0 | 0.0-0.0 | 0.0 | 0.0-0.0 | ~ | ~ | ~ | ~ | ~ | ~ |
| C47-C49 | Connective tissue | 2.3 | 1.3-3.3 | 1.6 | 0.7-2.5 | 2.0 | 1.2-2.7 | 2.2 | 1.2-3.1 | -2.2 | -18.8 | 17.9 | 6.4 | -10.4 | 26.3 |
| C50 | Breast | 0.3 | 0.0-0.6 | 42.0 | 38.2-45.7 | 0.4 | 0.1-0.7 | 42.3 | 39.0-45.5 | ~ | ~ | ~ | -0.7 | -3.2 | 1.8 |
| C51 | Vulva | - | - | 0.7 | 0.3-1.1 | - | - | 0.4 | 0.1-0.7 | ~ | ~ | ~ | ~ | ~ | ~ |
| C52 | Vagina | - | - | 0.5 | 0.1-0.9 | - | - | 0.8 | 0.4-1.2 | ~ | ~ | ~ | ~ | ~ | ~ |
| C53 | Cervix | - | - | 20.0 | 17.3-22.7 | - | - | 11.1 | 9.4-12.8 | ~ | ~ | ~ | -9.3 | -13.6 | -4.9 |
| C54 | Uterus (corpus) | - | - | 6.8 | 5.2-8.3 | - | - | 6.8 | 5.5-8.1 | ~ | ~ | ~ | -1.3 | -5.8 | 3.4 |
| C55 | Uterus (unspecified) | - | - | 1.5 | 0.6-2.3 | - | - | 2.2 | 1.4-2.9 | ~ | ~ | ~ | ~ | ~ | ~ |
| C56 | Ovary | - | - | 7.4 | 5.5-9.3 | - | - | 7.2 | 5.8-8.6 | ~ | ~ | ~ | 0.1 | -4.3 | 4.7 |
| C57 | Other female org. | - | - | 0.3 | 0.0-0.6 | - | - | 0.1 | 0.0-0.2 | ~ | ~ | ~ | ~ | ~ | ~ |
| C58 | Placenta | - | - | 0.1 | 0.0-0.2 | - | - | 0.0 | 0.0-0.0 | ~ | ~ | ~ | ~ | ~ | ~ |
| C60 | Penis | 1.0 | 0.4-1.6 | - | - | 0.7 | 0.2-1.2 | - | - | -16.2 | -31.4 | 2.5 | ~ | ~ | ~ |
| C61 | Prostate | 44.4 | 40.2-48.5 | - | - | 46.5 | 42.7-50.2 | - | - | 0.6 | -2.7 | 4.0 | ~ | ~ | ~ |
| C62 | Testicle | 4.5 | 3.1-5.8 | - | - | 4.7 | 3.5-6.0 | - | - | 0.9 | -8.9 | 11.6 | ~ | ~ | ~ |
| C63 | Other male org. | 0.1 | 0.0-0.2 | - | - | 0.0 | 0.0-0.0 | - | - | ~ | ~ | ~ | ~ | ~ | ~ |
| C64 | Kidney | 4.3 | 2.9-5.8 | 1.5 | 0.9-2.2 | 4.8 | 3.5-6.0 | 3.8 | 2.6-4.9 | 2.1 | -4.6 | 9.1 | 14.6 | 2.7 | 27.8 |
| C65 | Renal pelvis | 0.0 | 0.0-0.0 | 0.0 | 0.0-0.0 | 0.1 | 0.0-0.2 | 0.0 | 0.0-0.0 | ~ | ~ | ~ | ~ | ~ | ~ |
| C66 | Ureter | 0.0 | 0.0-0.0 | 0.0 | 0.0-0.0 | 0.1 | 0.0-0.2 | 0.0 | 0.0-0.0 | ~ | ~ | ~ | ~ | ~ | ~ |
| C67 | Bladder | 4.2 | 3.0-5.4 | 2.3 | 1.5-3.2 | 5.4 | 4.1-6.7 | 2.2 | 1.4-2.9 | 5.6 | -4.3 | 16.5 | 0.1 | -7.5 | 8.2 |
| C68 | Other urinary org. | 0.0 | 0.0-0.0 | 0.0 | 0.0-0.0 | 0.1 | 0.0-0.2 | 0.0 | 0.0-0.0 | ~ | ~ | ~ | ~ | ~ | ~ |
| C69 | Eye | 0.9 | 0.1-1.8 | 0.3 | 0.0-0.6 | 0.6 | 0.1-1.1 | 0.2 | 0.0-0.4 | ~ | ~ | ~ | ~ | ~ | ~ |
| C70-C72 | CNS | 5.6 | 3.5-7.7 | 4.0 | 2.1-5.9 | 6.6 | 5.0-8.2 | 5.9 | 4.7-7.1 | 2.7 | -5.0 | 11.0 | 8.2 | 2.4 | 14.4 |
| C73 | Thyroid | 4.8 | 3.5-6.2 | 22.8 | 20.2-25.5 | 6.6 | 5.1-8.1 | 27.5 | 24.7-30.4 | 3.1 | -4.6 | 11.4 | 2.4 | -4.2 | 9.5 |
| C74 | Adrenal gland | 0.4 | 0.0-0.8 | 0.0 | 0.0-0.0 | 0.4 | 0.0-0.8 | 0.0 | 0.0-0.0 | ~ | ~ | ~ | ~ | ~ | ~ |
| C75 | Other endocrine org | 0.2 | 0.0-0.4 | 0.3 | 0.0-0.6 | 0.9 | 0.4-1.4 | 1.6 | 0.8-2.3 | ~ | ~ | ~ | ~ | ~ | ~ |
| C81 | Hodgkin lymphoma | 1.8 | 1.0-2.6 | 2.1 | 1.2-3.1 | 2.0 | 1.1-3.0 | 1.0 | 0.4-1.5 | -4.8 | -19.6 | 12.9 | -11.9 | -20.1 | -2.8 |
| C82-6,C96 | NHL | 8.1 | 6.3-9.9 | 7.4 | 5.7-9.2 | 7.0 | 5.4-8.5 | 5.6 | 4.3-6.9 | -3.3 | -13.2 | 7.8 | -8.0 | -17.0 | 1.8 |
| C88 | MID | 0.3 | 0.0-0.6 | 0.4 | 0.0-0.7 | 0.3 | 0.0-0.6 | 0.4 | 0.1-0.7 | ~ | ~ | ~ | ~ | ~ | ~ |
| C90 | Multiple myeloma | 2.0 | 0.7-3.3 | 2.0 | 0.9-3.1 | 1.8 | 1.1-2.5 | 1.3 | 0.7-1.9 | ~ | ~ | ~ | -4.8 | -13.4 | 4.6 |
| C91 | Lymphoid leukemia | 4.6 | 2.8-6.4 | 2.7 | 1.5-4.0 | 2.7 | 1.6-3.8 | 1.8 | 1.0-2.6 | -5.6 | -15.5 | 5.6 | -3.3 | -17.3 | 13.2 |
| C92-C94 | Myeloid leukemia | 2.2 | 1.0-3.3 | 3.2 | 1.6-4.8 | 3.1 | 2.0-4.2 | 1.6 | 0.9-2.3 | 3.3 | -7.8 | 15.7 | -10.0 | -24.3 | 7.0 |
| C95 | Leukemia (unspecif) | 1.0 | 0.1-1.9 | 1.0 | 0.2-1.8 | 0.4 | 0.0-0.8 | 0.6 | 0.1-1.1 | ~ | ~ | ~ | ~ | ~ | ~ |
| D46 | MDS | 0.6 | 0.0-1.2 | 0.3 | 0.0-0.6 | 0.7 | 0.2-1.2 | 0.5 | 0.2-0.8 | ~ | ~ | ~ | ~ | ~ | ~ |
| All cancer sites | 193.6 | 143.3-243.9 | 217.1 | 166.3-267.8 | 193.9 | 153.5-234.4 | 194.0 | 156.8-231.2 | -5.7 | -243.3 | 262.7 | -77.0 | -294.9 | 167.0 | |
| All cancer sites without C44 | 186.2 | 137.5-234.8 | 211.1 | 161.6-260.5 | 181.9 | 143.5-220.4 | 185.3 | 149.6-221.0 | -12.1 | -240.9 | 246.7 | -80.8 | -290.4 | 154.3 | |
ASR=age-standardized rate. APC=annual percent change. 95% CI=95% confidence intervals. APC in bold=significantly different from zero (p<0.05). ~APC could not be calculated. †C26,C39,C48,C76,C80. CNS=central nervous system. NHL=non-Hodgkin lymphoma. MID=malignant immunoproliferative diseases. MDS=myelodysplastic syndromes
Table 3 Mortality rates and trends by sex, period and cancer site. Manizales, 2008-2017.
| ICD-10 | Site | Age-standardized mortality rate (100,000 person-years) | Trends in mortality rates | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 2008-2012 | 2013-2017 | 2008-2017 | |||||||||||||
| Men | Women | Men | Women | Men | Women | ||||||||||
| ASR | 95% CI | ASR | 95% CI | ASR | 95% CI | ASR | 95% CI | APC | 95% CI | APC | 95% CI | ||||
| C00-C14 | Mouth and pharynx | 1.1 | 0.5-1.7 | 0.8 | 0.3-1.2 | 1.7 | 1.0-2.4 | 0.7 | 0.3-1.1 | 11.8 | 0.4 | 24.6 | ~ | ~ | ~ |
| C15 | Esophagus | 2.3 | 1.5-3.2 | 2.0 | 1.3-2.7 | 2.1 | 1.3-2.8 | 0.9 | 0.5-1.3 | -5.6 | -14.6 | 4.2 | -12.7 | -17.9 | -7.2 |
| C16 | Stomach | 15.6 | 13.3-17.9 | 7.9 | 6.5-9.4 | 15.8 | 13.6-17.9 | 5.6 | 4.5-6.7 | -1.1 | -4.8 | 2.8 | -6.0 | -8.8 | -3.1 |
| C17 | Small intestine | 0.1 | 0.0-0.3 | 0.2 | 0.0-0.5 | 0.4 | 0.1-0.8 | 0.5 | 0.1-0.8 | ~ | ~ | ~ | ~ | ~ | ~ |
| C18 | Colon | 5.7 | 4.3-7.1 | 6.1 | 4.8-7.3 | 5.3 | 4.1-6.5 | 6.4 | 5.2-7.6 | -0.5 | -7.6 | 7.2 | 1.0 | -4.0 | 6.2 |
| C19-C20 | Rectum | 2.7 | 1.7-3.7 | 1.5 | 0.9-2.2 | 2.4 | 1.6-3.3 | 2.1 | 1.4-2.8 | 0.7 | -6.1 | 7.9 | 1.7 | -7.0 | 11.1 |
| C21 | Anus | 0.1 | 0.0-0.2 | 0.1 | 0.0-0.3 | 0.2 | 0.0-0.5 | 0.0 | 0.0-0.0 | ~ | ~ | ~ | ~ | ~ | ~ |
| C22 | Liver | 3.8 | 2.6-5.0 | 3.6 | 2.6-4.6 | 3.8 | 2.8-4.9 | 3.1 | 2.3-3.9 | -0.7 | -6.4 | 5.3 | -3.6 | -13.2 | 7.0 |
| C23-C24 | Gallbladder | 1.3 | 0.6-1.9 | 2.8 | 2.0-3.7 | 1.7 | 1.0-2.4 | 2.8 | 2.0-3.5 | 4.0 | -9.5 | 19.4 | 0.6 | -6.6 | 8.4 |
| C25 | Pancreas | 3.7 | 2.6-4.8 | 3.4 | 2.4-4.3 | 3.4 | 2.4-4.4 | 3.8 | 3.0-4.7 | -0.2 | -4.5 | 4.3 | 3.5 | -2.6 | 9.9 |
| † | Unspecified | 5.4 | 4.0-6.7 | 4.3 | 3.3-5.4 | 5.1 | 3.9-6.3 | 4.8 | 3.7-5.8 | -3.2 | -10.3 | 4.5 | -1.1 | -7.5 | 5.9 |
| C30-C31 | Nose and ear | 0.3 | 0.0-0.6 | 0.1 | 0.0-0.2 | 0.0 | 0.0-0.0 | 0.1 | 0.0-0.1 | ~ | ~ | ~ | ~ | ~ | ~ |
| C32 | Larynx | 1.7 | 1.0-2.5 | 0.6 | 0.2-1.0 | 1.5 | 0.8-2.1 | 0.4 | 0.1-0.7 | -5.8 | -16.6 | 6.3 | ~ | ~ | ~ |
| C33-C34 | Lung | 13.3 | 11.2-15.5 | 7.5 | 6.1-9.0 | 15.5 | 13.5-17.6 | 7.9 | 6.6-9.2 | 1.3 | -2.8 | 5.6 | -1.5 | -8.4 | 6.0 |
| C37-C38 | Other thoracic org. | 0.5 | 0.1-0.9 | 0.5 | 0.1-0.9 | 0.3 | 0.0-0.6 | 0.4 | 0.1-0.7 | ~ | ~ | ~ | ~ | ~ | ~ |
| C40-C41 | Bone | 0.9 | 0.3-1.5 | 0.3 | 0.0-0.6 | 0.8 | 0.3-1.5 | 0.8 | 0.2-1.3 | -0.2 | -14.3 | 16.2 | ~ | ~ | ~ |
| C43 | Melanoma | 0.9 | 0.3-1.5 | 0.5 | 0.2-0.9 | 1.5 | 0.8-2.1 | 0.7 | 0.3-1.0 | 11.6 | 1.7 | 22.5 | ~ | ~ | ~ |
| C44 | Skin non-melanoma | 0.9 | 0.4-1.4 | 0.4 | 0.1-0.7 | 0.7 | 0.2-1.1 | 0.4 | 0.1-0.6 | -0.9 | -12.5 | 12.3 | 0.2 | -12.8 | 15.0 |
| C45 | Mesothelioma | 0.0 | 0.0-0.0 | 0.2 | 0.0-0.4 | 0.1 | 0.0-0.2 | 0.2 | 0.0-0.4 | ~ | ~ | ~ | ~ | ~ | ~ |
| C46 | Kaposi sarcoma | 0.0 | 0.0-0.0 | 0.0 | 0.0-0.0 | 0.0 | 0.0-0.0 | 0.0 | 0.0-0.0 | ~ | ~ | ~ | ~ | ~ | ~ |
| C47-C49 | Connective tissue | 1.3 | 0.6-2.0 | 0.8 | 0.3-1.3 | 0.8 | 0.3-1.3 | 0.5 | 0.1-0.9 | -11.5 | -21.0 | -0.8 | -14.8 | -26.9 | -0.8 |
| C50 | Breast | 0.0 | 0.0-0.0 | 10.2 | 8.5-11.8 | 0.1 | 0.0-0.2 | 10.3 | 8.8-11.9 | ~ | ~ | ~ | 1.5 | -2.6 | 5.8 |
| C51 | Vulva | - | - | 0.1 | 0.0-0.3 | - | - | 0.3 | 0.0-0.6 | ~ | ~ | ~ | ~ | ~ | ~ |
| C52 | Vagina | - | - | 0.2 | 0.0-0.4 | - | - | 0.2 | 0.0-0.4 | ~ | ~ | ~ | ~ | ~ | ~ |
| C53 | Cervix | - | - | 6.7 | 5.3-8.0 | - | - | 4.6 | 3.5-5.6 | ~ | ~ | ~ | -5.9 | -11.0 | -0.5 |
| C54 | Uterus (corpus) | - | - | 1.9 | 1.2-2.6 | - | - | 2.0 | 1.4-2.7 | ~ | ~ | ~ | -0.1 | -9.8 | 10.6 |
| C55 | Uterus (unspecificied) | - | - | 1.0 | 0.5-1.6 | - | - | 0.7 | 0.3-1.1 | ~ | ~ | ~ | ~ | ~ | ~ |
| C56 | Ovary | - | - | 4.3 | 3.2-5.4 | - | - | 4.0 | 3.1-5.0 | ~ | ~ | ~ | 0.5 | -5.2 | 6.5 |
| C57 | Other female org. | - | - | 0.1 | 0.0-0.2 | - | - | 0.2 | 0.0-0.3 | ~ | ~ | ~ | ~ | ~ | ~ |
| C58 | Placenta | - | - | 0.0 | 0.0-0.0 | - | - | 0.0 | 0.0-0.0 | ~ | ~ | ~ | ~ | ~ | ~ |
| C60 | Penis | 0.5 | 0.1-0.9 | - | - | 0.2 | 0.0-0.5 | - | - | ~ | ~ | ~ | ~ | ~ | ~ |
| C61 | Prostate | 8.5 | 6.8-10.1 | - | - | 9.4 | 7.8-10.9 | - | - | 0.0 | -4.8 | 5.0 | ~ | ~ | ~ |
| C62 | Testicle | 0.9 | 0.4-1.5 | - | - | 0.6 | 0.2-1.1 | - | - | ~ | ~ | ~ | ~ | ~ | ~ |
| C63 | Other male org. | 0.0 | 0.0-0.0 | - | - | 0.0 | 0.0-0.0 | - | - | ~ | ~ | ~ | ~ | ~ | ~ |
| C64 | Kidney | 2.2 | 1.3-3.1 | 0.8 | 0.2-1.4 | 2.4 | 1.5-3.2 | 0.9 | 0.4-1.4 | 0.4 | -8.2 | 9.9 | ~ | ~ | ~ |
| C65 | Renal pelvis | 0.0 | 0.0-0.0 | 0.0 | 0.0-0.0 | 0.0 | 0.0-0.0 | 0.0 | 0.0-0.0 | ~ | ~ | ~ | ~ | ~ | ~ |
| C66 | Ureter | 0.0 | 0.0-0.0 | 0.0 | 0.0-0.0 | 0.0 | 0.0-0.0 | 0.0 | 0.0-0.0 | ~ | ~ | ~ | ~ | ~ | ~ |
| C67 | Bladder | 1.0 | 0.4-1.6 | 0.5 | 0.2-0.9 | 1.3 | 0.7-1.8 | 0.9 | 0.4-1.3 | ~ | ~ | ~ | ~ | ~ | ~ |
| C68 | Other urinary org. | 0.0 | 0.0-0.0 | 0.0 | 0.0-0.0 | 0.0 | 0.0-0.0 | 0.1 | 0.0-0.2 | ~ | ~ | ~ | ~ | ~ | ~ |
| C69 | Eye | 0.2 | 0.0-0.6 | 0.0 | 0.0-0.0 | 0.4 | 0.0-1.0 | 0.2 | 0.0-0.4 | ~ | ~ | ~ | ~ | ~ | ~ |
| C70-C72 | CNS | 3.3 | 2.2-4.5 | 2.3 | 1.4-3.1 | 3.7 | 2.6-4.9 | 2.1 | 1.3-2.8 | 4.4 | -5.2 | 14.9 | 1.2 | -8.2 | 11.6 |
| C73 | Thyroid | 1.1 | 0.5-1.7 | 1.0 | 0.5-1.5 | 0.4 | 0.0-0.7 | 1.5 | 0.9-2.1 | ~ | ~ | ~ | 0.5 | -10.2 | 12.5 |
| C74 | Adrenal gland | 0.2 | 0.0-0.4 | 0.2 | 0.0-0.5 | 0.3 | 0.0-0.8 | 0.0 | 0.0-0.0 | ~ | ~ | ~ | ~ | ~ | ~ |
| C75 | Other endocrine org. | 0.0 | 0.0-0.0 | 0.0 | 0.0-0.0 | 0.0 | 0.0-0.0 | 0.0 | 0.0-0.0 | ~ | ~ | ~ | ~ | ~ | ~ |
| C81 | Hodgkin lymphoma | 0.8 | 0.3-1.4 | 0.5 | 0.1-0.8 | 0.6 | 0.2-1.0 | 0.3 | 0.0-0.6 | ~ | ~ | ~ | ~ | ~ | ~ |
| C82-6,C96 | NHL | 3.3 | 2.2-4.4 | 2.4 | 1.6-3.2 | 3.6 | 2.6-4.6 | 1.6 | 1.0-2.3 | 2.7 | -5.5 | 11.5 | -6.5 | -13.2 | 0.8 |
| C88 | MID | 0.0 | 0.0-0.0 | 0.1 | 0.0-0.2 | 0.0 | 0.0-0.0 | 0.0 | 0.0-0.0 | ~ | ~ | ~ | ~ | ~ | ~ |
| C90 | Multiple myeloma | 1.6 | 0.8-2.3 | 1.3 | 0.7-1.9 | 1.5 | 0.8-2.1 | 0.7 | 0.3-1.1 | -6.9 | -16.2 | 3.4 | -7.1 | -16.8 | 3.7 |
| C91 | Lymphoid leukemia | 1.7 | 0.9-2.6 | 1.3 | 0.6-2.0 | 2.1 | 1.1-3.0 | 1.4 | 0.8-2.0 | -1.5 | -14.0 | 12.8 | ~ | ~ | ~ |
| C92-C94 | Myeloid leukemia | 1.7 | 0.9-2.6 | 1.6 | 0.9-2.3 | 2.4 | 1.5-3.4 | 1.3 | 0.7-1.9 | -1.2 | -14.2 | 13.7 | -7.2 | -21.4 | 9.6 |
| C95 | Leukemia (unspecif.) | 0.4 | 0.0-0.7 | 0.6 | 0.2-1.0 | 0.7 | 0.2-1.2 | 0.5 | 0.2-0.9 | ~ | ~ | ~ | ~ | ~ | ~ |
| D46 | MDS | 0.3 | 0.0-0.6 | 0.4 | 0.1-0.7 | 0.8 | 0.4-1.3 | 0.5 | 0.2-0.9 | ~ | ~ | ~ | ~ | ~ | ~ |
| All cancer sites | 89.3 | 61.8-117.4 | 81.1 | 56.3-106.4 | 93.6 | 67.3-120.4 | 76.4 | 53.8-98.6 | -2.4 | -197.0 | 213.5 | -55.8 | -214.1 | 119.0 | |
| All cancer sites without C44 | 88.4 | 61.4-116.0 | 80.7 | 56.2-105.7 | 92.9 | 67.1-119.3 | 76.0 | 53.7-98.0 | -1.5 | -184.5 | 201.2 | -56.0 | -201.3 | 104.0 | |
ASR=age-standardized rate. APC=annual percent change. 95% CI=95% confidence intervals. APC in bold=significantly different from zero (p<0.05). ~APC could not be calculated. †C26,C39,C48,C76,C80. CNS=central nervous system. NHL=non-Hodgkin lymphoma. MID=malignant immunoproliferative diseases. MDS=myelodysplastic syndromes.
Breast cancer
This was the most frequent malignant neoplasm in women and, in turn, the leading cause of cancer mortality in women. During the period studied, this type of cancer was responsible for 20% of all cancer cases in women. Additionally, incidence and mortality rates trends were stable between 2008 and 2017.
Prostate cancer
By far, the most common malignant neoplasm in men was prostate cancer. Approximately 1 in 4 cases of cancer in men occurred in this organ. This cancer ranked third among causes of cancer mortality in men, second only to stomach and lung cancer. The trends in incidence and mortality did not change during this period.
Stomach cancer
The incidence decreased in both men and women, although only in women was there a statistically significant reduction. This was the leading cause of cancer mortality in men, with a stable mortality rate. In women, on the other hand, there was a significant decrease in mortality, from being the second cause of mortality for the five years 2008-2012 to be the fourth for 2013-2017.
Lung cancer
In men, this neoplasm ranked third in incidence and was the second leading cause of cancer mortality; the trends in these rates did not show significant changes. On the other hand, in women, there was a substantial decrease in the incidence rate of this cancer, without a parallel reduction in the mortality rate. It is noteworthy that in women, this neoplasm oscillated between the sixth and eighth place in incidence during the period studied and was one of the main causes of cancer mortality in them.
Colon cancer
Colon cancer oscillated between the fourth and sixth position in incidence for men and women during 2008-2017, with no evidence of marked changes in its trends. Mortality in men remained stable during this decade; in women, although mortality also remained unchanged, colon cancer moved from fifth place in mortality between 2008-2012 to third place between 2013-2017, based on the drop in stomach and cervical cancer mortalities.
Thyroid cancer
This neoplasm was four times more frequent in women than in men. In women, this was one of the cancers with the highest incidence, second only to breast cancer, and although there was a slight increase in its trend, it was not significant. In men, this tumor was infrequent and its incidence did not change. The mortality rate for both men and women was low, and no changes in their trends were evident.
Cervical cancer
One of the most striking changes in this period was in cervical cancer: cervical cancer incidence and mortality rates decreased significantly, with APCs of -9.3 and -5.9, respectively.
Cancer of unspecified site
In incidence, unspecified cancers ranked fifth and seventh in men and women, respectively, and did not show significant variations in their trends. Mortality from these cancers remained unchanged.
Other findings
In women, a downward trend in incidence was observed in cancers of the lip, oral cavity and pharynx, gallbladder, and Hodgkin's lymphoma; in contrast, incidence increased considerably in CNS and kidney. In men, the incidence of esophageal and laryngeal cancers decreased significantly during this period. On the other hand, there was a marked decrease in mortality from esophageal and soft tissue cancers in women. In men, mortality rates increased significantly for cancers of the lip, oral cavity and pharynx and melanoma. As in women, mortality from soft-tissue cancer decreased.
Discussion
This study represents an update of previously published data 11 on the epidemiological behavior of cancer in Manizales, including a more extended period of incidence and mortality and a statistical analysis of trends. Taking the five-year period 2003-2007 as a baseline 11, a general increase in cancer incidence in the city was observed, a situation that is consistent with regional and national projections 4,20. This may be partly due to the observed aging of the population of Manizales 13. However, when scrutinizing the data for the decade 2008-2017 discriminated by sex, important differences were observed: at the end of the study period, the overall incidence rate in women decreased and equaled that of men, from a significant decrease in the rates of cervical, stomach, oral cavity, lung, gallbladder and Hodgkin's lymphoma cancers. Likewise, in the period studied, there was a slight decrease in cancer mortality for women, at the expense of lower mortality in cervix, stomach, esophagus, and connective tissue cancers. In contrast, overall cancer incidence and mortality did not decrease in men. This, together with the finding of a higher concentration of cases diagnosed at older ages in men compared to women, indicates the need to strengthen cancer control strategies with a differential approach by sex, in particular by promoting the participation of men in screening and early detection programs.
Breast, prostate, stomach, thyroid, lung, colon, and cervical cancers contributed more than half of all cancer cases in Manizales, which is why we will discuss them in depth below.
Regarding breast cancer, its incidence in Manizales is lower than that estimated by GLOBOCAN for South America (42.3 Vs. 56.4, respectively). Likewise, the figures are slightly lower than those estimated for Colombia (42.3 vs. 48.3) 1 and Cali (42.3 vs 48.0) 21, but higher than those for Pasto (42.3 vs 27.7) 22. The re-estimation of the incidence rate for the period 2008-2012 in Manizales is higher than that reported in CI5-XI, and is much closer to the figures reported by Bucaramanga and Cali for that period 8.
Despite the use of organized population-based screening for breast cancer in women since 2013, in this period, no significant achievements in the fight against this neoplasm are perceived: this remains the most frequent and deadly cancer in women. Contrary to what is expected for a tumor with an organized screening strategy, breast cancer mortality did not decrease between 2008 and 2017; even worse, it presented a slight increase compared to the mortality of 2003-2007 (10.3 Vs 8.3 respectively) 11. The non-reduction of mortality from this cancer in Colombia has been attributed to the low coverage of screening in the population, problems in the quality of mammography, and low access to diagnosis and timely treatment 23. Thus, it is a priority to address these problems and at the same time, strengthen health education, remove health system barriers, and investigate the particularities of this cancer in Colombian women.
Prostate cancer, the most frequent neoplasm in men, did not experience major changes in incidence and mortality during this period. However, regarding the 2003-2007 period, its incidence increased, possibly as a result of the screening activities initiated in 2013 in Colombia and the aging of the Manizales population 13. Interestingly, the incidence of this cancer in Manizales is lower than that reported in Cali (46.5 Vs 65.6) 21 and South America (46.5 Vs 62.5) 1, a phenomenon possibly attributable to a lower proportion of Afro-descendant population in Manizales; However, other factors, such as those related to screening coverage and case collection by the PCRM, could be related to this lower incidence, which merits further investigation. On the other hand, in Manizales there was no evidence of a decrease in mortality from this cancer, unlike what was found in Cali over a longer study period 24. Thus, it is a priority to consolidate screening activities, early detection and timely and comprehensive management of cases to achieve significant improvements in mortality from this cancer.
In Manizales, as in many regions of the world, a pronounced decrease in cases of stomach cancer has been observed in recent years, which has been attributed mainly to the decline in the prevalence of chronic Helicobacter pylori infection 25. However, the incidence and mortality of gastric cancer remain high in this population, mainly in men, in whom the incidence rate is twice that of women, and the mortality rate is three times that found in women, a difference that was accentuated in the period 2013-2017 from the decline in cases and deaths in women. Thus, it is of interest for future studies to analyze the possible differences by sex in exposure to risk factors of various kinds that could explain the differences observed: the significant decrease in incidence in women but not in men. The significant decline in mortality from this cancer in women but not in men could be related to the existence of cultural factors linked to differential knowledge, attitudes and practices about the disease that could favor earlier diagnosis or better adherence to treatment in women. In addition, the adoption of screening programs based on digestive endoscopy, implemented in countries with a high frequency of the disease, could be considered by Colombian health authorities to impact mortality and improve survival 26,27.
The incidence and mortality rates for cervical cancer showed a reduction of close to 50%, taking the period 2003-2007 as the baseline. This disease went from being the leading cause of death from cancer in women for 2003-2007 11 to the sixth for 2013-2017. This downward trend has also been observed in many Latin American countries 28, as well as in other regions of the world 1; However, its incidence is still above the elimination limit defined by the WHO (4 cases per 100,000 women). Such achievements could be related to improvements in the socio-economic conditions of the population, prevention and treatment of sexually transmitted infections and, above all, screening and timely management of pre-neoplastic lesions. The vaccination already implemented against HPV will further reduce incidence and mortality in the upcoming years.
Colon and rectal cancer have remained an important cause of morbidity and mortality in Manizales, without major variations in the studied period. In contrast to what has been evidenced in the world 1, women presented incidence rates slightly higher than men in the first five years of the study period, although not statistically significant. Promoting healthy lifestyle is a crucial element for the control of this disease since a sedentary lifestyle, overweight and obesity, excessive alcohol consumption, smoking and consumption of red meat and/or processed meats are recognized risk factors for the development of this cancer 29. It is expected that the screening activities recently adopted in Colombia may have an impact in the coming years, mainly in terms of mortality.
Lung cancer continues to be a very frequent and lethal neoplasm, particularly in men: for 2013-2017 the incidence and mortality rates in men were twice those of women. Smoking, responsible for 80% of lung cancer deaths in Colombia 30, has a high prevalence in the country, especially in men 31. This situation may be related to the differential affectation by sex observed in this research. This problem makes it necessary to strengthen preventive actions aimed at controlling smoking with a differential approach by sex, some of which are contained in the WHO MPOWER strategy 32.
Previous local research had already emphasized the high frequency of thyroid cancer, particularly in women 33. In the present investigation, the incidence rate of this cancer increased and doubled the rates observed in Pasto (22) and Cali 21. This increase, also observed in the world 1, has been attributed, in part, to overdiagnosis of this cancer due to greater availability of specialized personnel and an improvement in health technologies, specifically, ultrasound; this could result in interventions of limited benefit for patients 34. In Manizales, carcinogen emissions from industries have also been linked to a possible real increase in cancer incidence 35,36. However, despite the marked increase in incidence, mortality from this cancer remains low.
Lip, oral cavity, and pharyngeal cancer, another phenomenon related to smoking, also showed differential effects by sex, similar to those observed with lung cancer: while incidence and mortality increased in men, the incidence decreased in women. The increase in the incidence of CNS neoplasms is mainly due to the recent uptake of benign tumors by the PCRM.
The information presented here is expected to contribute to decision-making in clinical settings, to expanding knowledge of cancer epidemiology in Colombia and Latin America, and, above all, to prioritizing population-based interventions and the definition of public health policies for cancer control.
One of the limitations of this study is the considerable number of DCO cases for some types of cancer, probably explained by the late access to death data and the denial of access to data consultation by some sources consulted by the PCRM, such as IPS and diagnostic centers. These results call for additional efforts by the PCRM to improve this quality indicator through a "tracing back" strategy 37. Notably, for the five-year period 2013-2017 the percentage of DCO cases is lower, reflecting an improvement in the quality of the PCRM processes and establishing a favorable outlook concerning this topic.
On the other hand, the time considered for this study (10 years) may be still too short to detect significant changes in the rates of some cancers. In addition, changes in data quality indicators, specifically the decrease in DCO cases in the last period, may reflect an improvement in the completeness of the PCRM, which should lead to a cautious interpretation of trend results. DCO cases generally have less detail on tumor variables, so some common locations in DCO cases, such as lung, liver, or unspecified sites, may correspond to primary tumors in other locations. For example, concerning lung cancer in women, the significant decrease in the trend could be explained by a better specificity in topographic coding resulting from the reduction in the percentage of DCO cases between periods; that is, an overestimation of incidence could have been observed in the first period for some cancer sites that often correspond to DCO cases, especially for neoplasms with high lethality 37.
It is a priority to strengthen research on this topic, as there are still several gaps in knowledge in our context. In this sense, it is essential to work collaboratively with the different actors that are part of the health system because their human and documentary resources are essential for developing PCR research activities in Colombia.
Conclusions
The aging population of Manizales has contributed to an increased cancer burden in the city.
In terms of incidence and mortality, progress in the fight against cancer is still discrete and has been concentrated mainly in women, making it imperative to strengthen a differential approach by sex when planning strategies for cancer control.
It is a priority to consolidate screening actions for certain cancers, reinforce strategies to promote healthy lifestyles, advance in the effective control of smoking, emphasize early detection and timely management of cases, remove heath system access barriers, and encourage local cancer research.











 texto em
texto em