Introduction
High blood pressure (HBP) is a highly prevalent disease in Western countries and is considered the most prevalent risk factor for cardiovascular disease.1 The use of new technologies in the diagnosis and treatment of patients with HBP may be of significant benefit since it has been shown, for example, that antihypertensive therapy via teleconsultation and telemonitoring of blood pressure (BP) at home can achieve better BP control than conventional care and, consequently, reduce the risk of cardiovascular disease.2
During the mandatory social isolation (lockdown) adopted as a preventive measure during the COVID-19 pandemic, health policy strategies changed radically at the global level.3 During this period, priority was given to the care of patients infected with COVID-19 and the diagnosis and follow-up of prevalent chronic conditions, such as HBP, was pushed to the background.4 In addition, many patients refused to go to hospitals for fear of contracting the virus.5 In order to respond adequately to this situation, the institutions defined new strategic axes of care in which available technological tools, like telemedicine,6,7were adapted.
Telemedicine is a modality of care that avoids exposure to contagion and reduces the need for human and financial resources. However, its main drawback, among others, is the impossibility of performing a physical examination and complementary explorations; furthermore, its main limitation is the lack of generalized access by patients.8
In Argentina, telemedicine began to be used in 1999, but the results were not very favorable at the time.9 However, the COVID-19 pandemic demonstrated, among other things, that a considerable number of patients can be treated remotely and that the necessary logistics can be developed rapidly.10 In the case of the province of Tucumán (Argentina), there was already a telemedicine service operating from the headquarters of the Servicio Provincial de Salud (SIPROSA for its acronym in Spanish) before the COVID-19 pandemic. Furthermore, in response to the measures to contain the spread of SARS-CoV-2 (the virus that causes COVID-19), the SIPROSA designed a user-friendly strategy to provide virtual care using WhatsApp video calls, a free application widely used by the general population. To this end, the SIPROSA IT team trained a group of physicians from different specialties with a high demand for telemedicine consultations to offer this service, which led to the creation of the SIPROSA Virtual Cardiology Clinic.
The measurement of elevated BP values is a frequent reason for consultation in face-to-face medical services, which could be extrapolated to telemedicine consultations. In view of the above, the objective of this study was to describe the characteristics of patients with or without a previous diagnosis of HBP (HBP and non-HBP, respectively) who were assessed via teleconsultation by the Virtual Cardiology Clinic of the SIPROSA during the COVID-19 pandemic due to elevated BP values.
Materials and methods
Study design and type
Descriptive cross-sectional study carried out in patients with or without a previous diagnosis of HBP (HBP and non-HBP, respectively) residing in Tucumán.
Study location
Tucumán is a province located in northwestern Argentina with an area of 22 525km2 and a population of 1 703 186 inhabitants according to the 2022 census.11 There are no recent data on the prevalence of HBP in Tucumán, but it is estimated that in Argentina it is 36.3% among the general population.12 Although several health systems coexist in Tucumán, both public and private, the SIPROSA, a dependency of the Ministry of Public Health, is in charge of planning and executing the healthcare promotion, protection, repair and rehabilitation strategies targeted to most of the inhabitants of this province.13
Study population and sample
The study population included all patients over 18 years of age who contacted the SIPROSA Virtual Cardiology Clinic for the first time between July and September 2021 due to elevated BP values (N=415). A patient was considered to have elevated BP if their systolic BP (SBP) was ≥140 mmHg and/or their diastolic BP (DBP) was ≥90 mmHg.
It should be noted that only BP readings obtained under the conditions specified by the Argentine Consensus on Arterial Hypertension14 with a sphygmomanometer (aneroid or digital) validated at http://www.dableducational.org 13 were taken into account for the present study. Patients who had infectious diseases at the time of consultation and pregnant women were excluded, so the final sample consisted of 275 patients (HBP=167; non-HBP=108).
Procedures
Once the teleconsultation appointment was scheduled through the SIPROSA website or through the call center, the doctor in charge made a video call via WhatsApp using a computer integrated into the SIPROSA information system, so that it could be logged in the patient's digital medical record. Physicians had access to the patients' digital medical records at all times and could access their personal health history and enter the data obtained during the teleconsultation in real time.
Taking into account the SBP and DBP values provided by the patient during the consultation, differential pressure (DP) and mean arterial pressure (MAP) values were calculated using the following formulas: DP=SBP-DBP and MAP=DBP+DP/3. In addition, during the video call, patients were asked about their age, sex, weight, and height. Body mass index (BMI) was calculated using the weight/height2 formula and patients were categorized as underweight (BMI <18.5), normal weight (BMI ≥18.5 and <25), overweight (BMI >25 and <30), obese (BMI ≥30 and <35), severely obese (BMI ≥35 and <40), or morbidly obese (BMI ≥40).15
During the consultation, the presence of risk factors (RF) for heart disease (diabetes, dyslipidemia, or smoking) was also documented and a score was assigned based on the number of RFs observed (0 to 3). Finally, the patient was asked about the regular usage of antihypertensive medication and whether they were following a low-sodium diet.
Statistical analysis
Once collected, data were entered into a Microsoft Excel 2010 spreadsheet. For descriptive analysis, percentages and absolute frequencies were calculated for categorical variables, and means and standard errors (±) were calculated for quantitative variables. Regarding inferential analysis, to identify differences between groups (HBP vs. Non-HBP) according to sex, bivariate analyses were performed using, depending on the nature of the variables and the distribution of the data, analysis of variance (ANOVA), t-Student test, and X2 test. Moreover, Pearson's correlation coefficient (r) was used to establish the correlation between age and BMI, on the one hand, and SBP, DBP and DP values and the number of antihypertensive drugs used, on the other. All statistical tests were performed in GraphPad Prism 5.0 and a significance level of p<0.05 was considered.
Ethical considerations
The study was approved by the Research Ethics Committee of the Ministry of Health Research Directorate of the Province of Tucumán in accordance with Opinion No. 33 of 2021 and followed the ethical principles for biomedical research involving human subjects established in the Declaration of Helsinki.16 Confidentiality and anonymity of the data were preserved.
Results
Of the 275 patients, 69.45% were women and the mean age was 48.02±0.82 years, being higher in the HBP group for both men and women, with statistically significant differences (Table 1). On the other hand, regardless of sex, no significant differences were observed in SBP, DBP, DP and MAP values between the HBP and non-HBP groups (Table 1).
Table 1 Mean values of the variables analyzed in the patients studied according to sex and the presence of high blood pressure.
| Variable | Total | non-HBP | HBP | p-value (ANOVA) | ||
|---|---|---|---|---|---|---|
| (n=275) | Female (n=69) | Male (n=39) | Female (n=122) | Male (n=45) | ||
| Age (years) | 48.02±0.85 | 42.8±1.4 | 41.1±2.21 | 51.27±1.15 * | 53.16±2.06 * | <0.0001 |
| Body mass index | 32.24±0.40 | 32.37±0.90 | 31.83±1.07 | 32.22±0.66 | 32.45±0.88 | 0.98 |
| Systolic blood pressure (mmHg) | 162.37±1.21 | 163.36±2.81 | 160.46±2.90 | 162.77±1.76 | 161.40±2.76 | 0.88 |
| Diastolic blood pressure (mmHg) | 96.06±0.84 | 95.55±1.69 | 98.06±1.99 | 95.66±1.37 | 96.31±1.80 | 0.82 |
| Differential pressure (mmHg) | 65.28±1.27 | 66.97±2.72 | 60.32±2.80 | 66.02±1.92 | 64.62±3.05 | 0.45 |
| Mean arterial pressure (mmHg) | 117.82±0.84 | 117.87±1.81 | 118.17±2.20 | 117.67±1.29 | 117.85±1.71 | 0.99 |
HBP: high blood pressure; ANOVA: analysis of variance. * p<0.001 vs. non-HBP.
Source: Own elaboration.
Regarding blood pressure, there were no significant differences according to the type of sphygmomanometer used for SBP (aneroid: 162.56±1.56; n=143 vs. digital: 162.16±1.87 mmHg; n=132; p: not significant (NS), t-Student test) and for DBP (aneroid: 96.12±1.07; n=143 vs. digital: 95.99±1.31 mmHg; n=132; p: NS, t-Student test).
The mean BMI value of the participants was 32.24±0.40 (non-HBP: 32.18±0.70 vs. HBP: 32.29±0.48; p: NS, t-Student t-test). In addition, 12.73% had normal weight, 25.45% were overweight, and 61.82% had some degree of obesity (33.09% obese, 15.27% severely obese, and 13.45% morbidly obese). It should be noted that none of the patients were underweight and there were no significant differences in the proportion of normal weight, overweight or any degree of obesity between the two groups according to sex (x2: 5.61; p: NS). On the other hand, 22.91% of the patients were on a low-sodium diet, 41.45% did not know if they were on a low-sodium diet, and 35.64% were not on a low-sodium diet. Figure 1 shows compliance with a low-sodium diet in both groups according to sex, showing that the HBP group had a higher percentage of patients who followed a low-sodium diet, with significant differences.
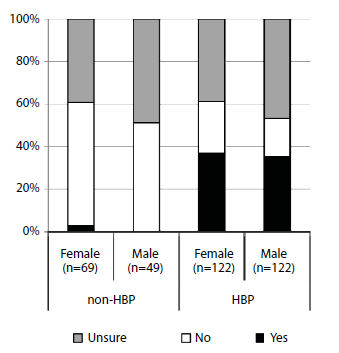
Source: Own elaboration.
Figure 1 Proportion of patients on a low-sodium diet according to sex and presence of hypertension. Non-HBP vs. HBP: X2: 53.71; p<0.001. Non-HBP: female vs. male: X2: 0.72; p: NS. HBP: female vs. male: X2: 0.54; p: NS.
Almost half of the patients (48.36%) presented at least one of the RFs considered (25.09% dyslipidemia, 22.55% diabetes, and 13.82% smoking) and the mean RF score was 0.61±0.04 (females: 0.56±0.05 vs. males: 0.74±0.08; p<0.05, t-Student test). Regarding the number of RFs for cardiovascular disease, 37.09% reported 1, 9.45% had 2, and 1.82% presented with 3. Figure 2 shows the average number of RFs, indicating that men with HBP have the highest average. Figure 3 shows the proportion of patients with RFs in both groups according to sex, showing that the prevalence of both diabetes and dyslipidemia was higher in men with HBP, while the frequency of smoking was higher in men who did not have HBP.
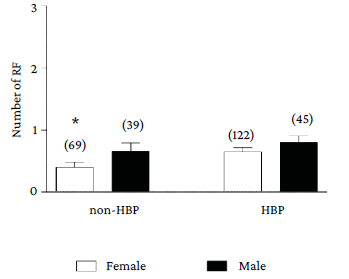
* p<0.05 non-HBP women vs. HBP men (ANOVA).
Source: Own elaboration.
Figure 2 Average number of risk factors in both groups analyzed according to sex. HBP: high blood pressure.
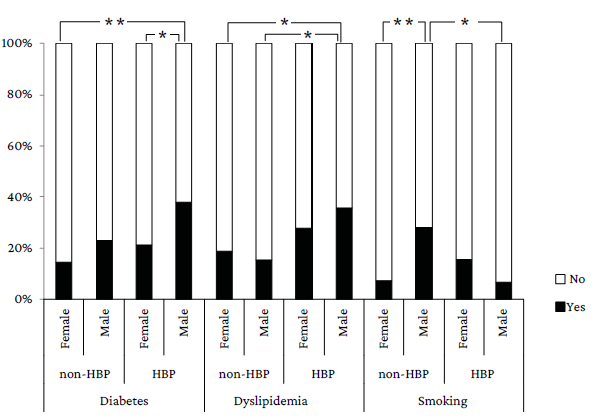
*p<0.0S, **p<0.001;X2.
Source: Own elaboration.
Figure 3 Frequency of patients with risk factors in both groups analyzed according to sex.
Regarding the reason for consultation, 79 patients (28.73%) reported an increase in SBP, 8 (2.90%) presented with an increase in DBP, and 188 (68.36%) reported an increase in both. Furthermore, when the population was divided into groups (non-HBP and HBP), no differences were observed in this item between men and women (X2: 1.25; p: NS).
In the non-HBP group, none of the patients were taking antihypertensive medication on a regular basis. In the HBP group, most patients took <2 drugs (mean: 1.2±0.1 drugs), with no differences between women and men (p: NS), including angiotensin-converting enzyme inhibitors (ACE inhibitors), angiotensin II receptor blockers (ARA II), beta-blockers (ßB), calcium channel blockers (Ca antag), and diuretics.
It should be noted that in the HBP group, 11.98% of patients took no antihypertensive drugs (14 women and 6 men), 57.48% took 1 drug (71 women and 25 men), 25.75% (30 women and 13 men) took 2 drugs, 4.19% (7 women) took 3 drugs, and only 1 patient (male) took 4 drugs. Figure 4 depicts the usual antihypertensive medication of the patients in the HBP group who used 1 or 2 drugs, as well as the combination of drugs in the latter case; it also shows that the most frequent drugs used in monotherapy were ACE inhibitors (53 patients) and ARA II (38 patients). Diuretics were not used as monotherapy in any case and the 3-drug combinations found were: ACE + ßB + diuretics or ARA II (2 patients); ARA II + Ca antag + ßB or diuretics (3 patients), and Ca antag + diuretics + ACE or ßB (2 patients).
Figure 5 shows the correlation between patient age and SBP and DBP values in each group according to sex. In the non-HBP group, no significant correlation was observed between BP values and age, both in women and men (Figure 5A and 5B, respectively). In the HBP group, patient age correlated significantly with SBP values, being positive in females (Figure 5C) and negative in males (Figure 5D).
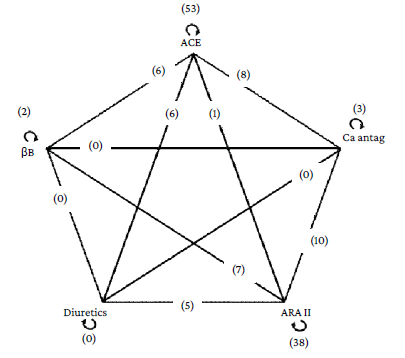
Circular arrow: monotherapy; straight line: 2-drug combination; ACE: angiotensin-converting enzyme inhibitors; ARA II: angiotensin II receptor blockers; ßB: beta-blockers; Ca antag: calcium channel blockers.
Source: Own elaboration.
Figure 4 Antihypertensive medication in patients in the group with high blood pressure and on mono-therapy or a combination of two drugs.
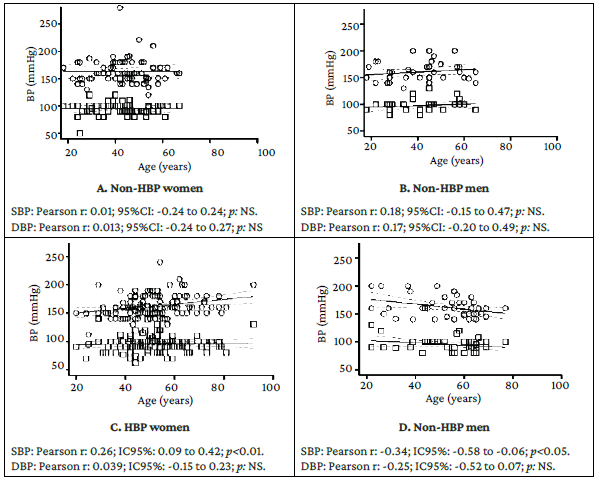
O: systolic blood pressure.
□ : diastolic blood pressure.
Source: Own elaboration.
Figure 5 Correlation between age and systolic blood pressure and diastolic blood pressure in each group according to sex.
Age was significantly correlated with DP values in women in the HBP group (Pearson r 0.25; 95%CI: 0.07-0.42;p<0.01), but not in men (Pearson r -0.13; 95%CI: [-0.43]-[0.19];p: NS). On the other hand, in the non-HBP group, the correlation was not significant either in women (Pearson r: -0.07; 95%CI: [-0.32]-[0.19];p: NS) or in men (Pearson r: 0.33; 95%CI: [-0.023]-[0.62]; p: NS). Furthermore, with regard to the regular use of antihypertensive drugs, a significant correlation between age and the number of antihypertensive drugs was observed in the HBP group among women (Pearson r: 0.27; 95%CI: 0.09-0.42; p<0.01), but not among men (Pearson r: 0.01; 95%CI: [-0.29]-[0.31]; p: NS). Finally, no significant correlation was observed between BMI and SBP, DBP and DP values in any group, regardless of sex.
Discussion
This study indicates that the population treated at the Virtual Cardiology Clinic of the SIPROSA for increased BP values were in the middle adulthood stage (mean age: 48.02±0.82 years) and that the majority of patients were female (n=191, of whom 122 had HBP) and were overweight or obese.
The mean age of the patients in the present study could be explained by a confluence of 2 factors: on the one hand, younger people (young adulthood: <40 years) may not give relevance to BP values and cardiovascular risk, or may not be concerned about measuring their BP, so they may not feel the need to seek medical care17 and, on the other hand, it is likely that older people (late adulthood: >60 years) do not have sufficient knowledge on how to use new technologies appropriately and therefore cannot easily access services such as telemedicine. The latter point has already been discussed in studies that have established that older patients have less access to this technological tool.18,19
In the present study, most patients were female (69.45%), which is consistent with what has been observed in studies on face-to-face consultations, both in nursing20 and medicine,21 where 56.6% and 53.8% of patients, respectively, were female. This suggests that, regardless of the channel of care (face-to-face or virtual), women are more likely to seek medical care.
The prevalence of obesity, reflected in the mean BMI of the population (32.2±0.4) and the percentage of obese patients (61.81%), was high. This is important because obesity is associated with potentially serious health complications15,22and can even have an effect on vascular function from an early age.23 It should be pointed out that the present study was conducted in a telemedicine service, so some negative biases of this modality of care cannot be ruled out, such as the difficulty in accessing the WhatsApp video call application (because the application and/or internet access are not available) and positive biases such as the fact that obese patients feel more comfortable receiving online care than face-to-face care. This is consistent with what has been reported in several studies such as the one conducted by Sadeghian et al.24 in 30 obese pediatric patients, which found that the majority of participants (>85%) were comfortable and satisfied with being cared for using telemedicine.
The high prevalence of obesity in the present study could be explained by the high prevalence of obesity among the general population of Tucumán. This had already been reported by Holownia et al.25 in a study conducted in a rural indigenous community in this province, where 36% of 202 participants were obese and 29% overweight. Corder & Cesani26 also found that 27.2% of the participants were obese and 23.0% overweight in a study conducted in 666 schoolchildren aged 8 to 12 years, where 27.2% of the participants were obese and 23.0% overweight. It is also important to take into account the effect of the confinement implemented as a measure to contain the spread of SARS-CoV-2, since it has been proposed that these measures, although successful from an epidemiological standpoint, could promote obesity and associated metabolic diseases.27
It should be noted that obesity and high blood pressure lead to an increase in cardiovascular risk28 and the costs associated with the treatment of these patients,29 so this issue should be studied in greater detail in further studies.
The present study also found that a high percentage of participants (35.64%) did not follow a low-sodium diet. In this regard, it has been reported that this type of diet can decrease SBP by 4.8 mmHg30 since there is a linear correlation between SBP values and the decrease in sodium intake.31 Therefore, future measures for these patients should reinforce compliance with this diet. On the other hand, almost half of the patients presented at least one of the RFs considered (diabetes, dyslipidemia and smoking), with men with HBP having the highest average RF score. These data are similar to those described in other populations in Argentina.12,25
In the present study, the majority of consultations were required due to an increase in SBP and DBP values, which is of great relevance because it has been described that an increase in these values is associated with the development of cardiovascular events such as stroke and coronary artery disease.32
Considering that 60.72% of the patients had HBP, that 11.98% of them were not on medication, and that most of those who used antihypertensive therapy regularly took only one drug, mainly ACE inhibitors or ARA II, it can be assumed that most of the participants had uncontrolled HBP. Clinical practice guidelines on hypertension in Argentina recommend early prescription of at least two drugs as part of the antihypertensive treatment, since this therapeutic behavior is associated with greater adherence, which in turn helps to prevent target organ damage.14 Therefore, it can be assumed that insufficient medication, either due to inertia on the part of the treating physician or lack of patient adherence to treatment, plays an important role in the elevated BP values for which the patients consulted. This hypothesis is reinforced by the high prevalence of obesity and the absence of a low-sodium diet, as evidenced in the present study.
The high percentage of patients without HBP (39.27%) might be attributable to the modality of care provided by the SIPROSA Virtual Cardiology Clinic, since the convenience of video call via WhatsApp could have led to an increase in the demand for consultations by patients without HBP who otherwise would not have attended a cardiology service. Thus, based on what is described in the current national guidelines on HBP,14 the question is whether these individuals are newly discovered patients with HBP, or whether they did not really have HBP and their BP levels increased due to the stress caused by the pandemic. Although in the present study the presence of white coat HBP could be ruled out because the BP measurements were taken at the patients' homes, it should be borne in mind that since it is a medical consultation, regardless of the modality, there could also be a stress reaction even if the BP is not measured by a physician or a nurse. This particular point should be studied in greater depth later on.
Likewise, it was observed that the mean age of patients in the non-HBP group was significantly lower than in the HBP group, raising the question of whether these patients might develop HBP in the future, if they are not already patients with new-onset HBP. This statement would be supported by the positive correlation between age and SBP and DP values observed in the women in the HBP group, although it should be noted that this correlation was negative among the men in this group. In this regard, it has been reported that men have lower adherence to antihypertensive treatment,33,34so it can be hypothesized that the younger the age, the lower the adherence to medication and the lower the hygienic-dietary measures, with the subsequent increase in BP values. However, this correlation should be studied in more detail in future studies.
Several studies on the use of telemedicine in developed countries have demonstrated its advantages8,35,36and indicated that it could be key for the initial assessment of patients in different specialties, such as ophthalmology37 or cardiology,38 and for the follow-up of different types of patients, such as obese patients and those with HBP.35,36,39However, literature on this subject is scarce in developing countries, where its massive implementation could pose several difficulties to be overcome, such as the training of qualified professionals, patient access to the platform, and payment for the software.
The Virtual Cardiology Clinic could be used as a gateway to the cardiology service for patients in Tucumán, since this tool is intended to be used in all cases (HBP and non-HBP) to follow up each subject individually, assess their cardiovascular risk, and adjust their medication if necessary. In this regard, in a meta-analysis that included five studies conducted in the United States and Canada in adult patients with HBP and diabetes, Zhang et al.40 demonstrated that telemedicine has great potential to improve the quality of care.
Finally, the present study suggests that health policies in Tucumán should focus on eating habits, and for this purpose the SIPROSA telemedicine service can be used as a tool for patient admission and follow-up and thus control of RFs.
The limitations of the present study include: 1) the fact that the reason for consultation was high BP values, which could lead to a bias in the selection of the sample, since more people with HBP (known or not) could be included as these patients have a greater tendency to self-monitor BP, and 2) that there are no data available on the expertise of the participants when taking the BP readings that led to the consultation.
Conclusions
In the present study, a high prevalence of obesity was observed and almost half of the participants had at least one associated RF (diabetes, dyslipidemia, and smoking). In the HBP group, most patients used only one antihypertensive drug and did not follow or did not know whether they were following a low-sodium diet. The percentage of patients with no history of HBP was high. In this sense, it is hypothesized that the convenience of the teleconsultation system implemented (video call via WhatsApp) could have increased the demand for consultations by patients without HBP.
Based on the results obtained, it is possible to state that the Virtual Cardiology Clinic of the SIPROSA was able to consolidate itself as a useful tool for the evaluation and follow-up of HBP and non-HBP patients in Tucumán.















