What do we know about this problem?
Restricted cervical mobility is a common occurrence in trauma patients. The C-MAC D-blade eliminates the need to align the oral, pharyngeal, and laryngeal axes in patients with restricted cervical mobility, providing a better glottic view. However, intubation is difficult but can be managed with the help of intubating aids.
What does this study contribute?
In a simulated scenario, a 60o angled stylet or a bougie may be used to facilitate intubation, with the stylet being a better aid in terms of ease and intubation time.
INTRODUCTION
A C-MAC D-blade with a highly angulated video laryngoscopy blade was introduced into the C-MAC system for management of extremely difficult airway scenarios with an alternative blade. 1 Despite an enhanced glottic view, it was still difficult to introduce the endotracheal tube into the trachea, due to the increased blade curvature. 2 A review of the literature showed that intubating aids like a stylet or a bougie helps to circumvent this laryngoscopy paradox, shortening intubation time and reducing the hemodynamic stress response. 3-6 However, very few human trials have compared these intubation aids with the C-MAC D-blade in terms of ease of intubation, which is crucial in case of a difficult airway.
The decision was made to conduct a prospective, randomized, controlled, single center trial intended to compare the ease of intubation between the 60° angled C-MAC stylet and a bougie while using the C-MAC D-blade, in patients with simulated restricted cervical mobility.
METHODS
A prospective, randomized, controlled, single center study was conducted, following the approval of the Institutional Ethics committee (IEG766/2019) and upon registration at the Clinical Trials Registry of India (CTRI), India. (CTRI/2020/09/027672). A total of 48 patients, American society of Anesthesiologists physical status (ASA PS) I and II, aged between 18-65 years requiring general anesthesia and endotracheal intubation for elective surgery were included in the study. Anticipated difficult airway and patients requiring rapid sequence intubation were excluded from the study.
After a detailed pre-anesthesia assessment, the informed consent was obtained, and the patients were randomly assigned to group S (Stylet) and group B (Bougie), based on computer generated random number sequences. oral Alprazolam 0.25 to 0.5 mg was administered on the previous night and morning of the surgery to manage anxiety. on arrival to the theatre, baseline vitals were recorded with standard monitors. A peripheral intravenous access was secured and pre-oxygenation was administered for 3 minutes. Then, the patients received an induction with IV propofol 2-2.5 mg/kg, fentanyl 2 μg/kg and were paralyzed with vecuronium 0.img/kg after confirming the ability to ventilate with bag and mask. Anesthesia was maintained with 1 MAC of isoflurane with oxygen.
Once complete muscle relaxation was achieved, manual in-line cervical stabilization was provided and patients were intubated by a skilled anesthesiologist with prior experience in the C-MAC D-blade video laryngoscope with the help of stylet in group S and bougie in group B. The endotracheal tube position was confirmed by lung auscultation and capnography, followed by mechanical ventilation under anesthesia.
Ease of intubation and a reduced number of attempts were noted. Ease of intubation was scored by the practitioner performing the intubation as good if successful in the first attempt without any manipulation; satisfactory, if intubation was successful in the first attempt requiring manipulation; poor, if intubation was successful in a second attempt with or without manipulation.
Intubation attempt was defined as each approach of the endotracheal tube from the tongue to the glottic entrance after visualization of the glottis. The manipulations employed to assist intubation were external laryngeal maneuver, tube rotation, partial withdrawal of the blade. The time needed to visualize the vocal cord was recorded; i.e., from the beginning of insertion of the video laryngoscope into the oral cavity until an optimal laryngeal view was obtained. Time to pass the endotracheal tube was measured from the start of insertion of the endotracheal tube into the oral cavity until visualization of the black line of the endotracheal tube above the vocal cords. The total time required for intubation was the sum of the above-mentioned two recordings. Any trauma during intubation was assessed based on the presence of blood on the endotracheal tube during extubation. Two attempts at intubation were permitted; however, if intubation failed (i.e. intubation not possible or required > 120 s or > two attempts), then the patients would be intubated using a Macintosh laryngoscope.
Hemodynamic parameters, both heart rate and blood pressure at baseline, 1 min, 3 min, 5 min, 10 min, 15 min after intubation were also recorded. Any increase in heart rate or mean arterial pressure at the time of intubation beyond 30% of the baseline, was treated by deepening the plane of anesthesia.
STATISTICAL ANALYSIS
The sample size was estimated using the GPower software version 3.1.9.4 (Franz Faul, Universltat Kiel, Germany). The sample size was calculated taking ease of intubation as the primary outcome at an effect size(d) measured at 73% for comparison between the two groups, based on a study conducted by Tosh P et al. 5 With a 95% confidence interval (level of significance at 5%) and an 80% power of the study, the total sample size estimated was 48 with 24 in each group. The Mann-Whitney U test was used for analyzing numerical values (age, Body mass index (BMI), Percentage of Glottic Opening (POGO) score, mean time for intubation). Gender, number of attempts required for intubation and ease of intubation were analyzed using the Chi-square test. The statistical analysis used SPSS version 22.0 with a level of significance of p < 0.001.
RESULTS
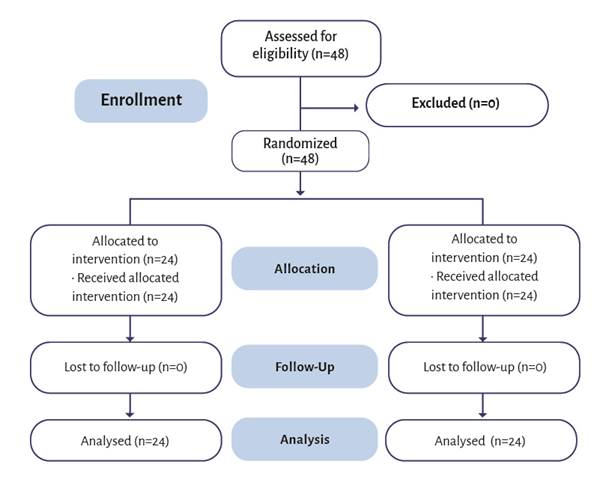
A total of 48 patients were recruited for the study. The flow of participants is illustrated on a CONSORT flow diagram (Figure 1) (source: as per CONSORT 2010 guidelines). The demographics of the participants in both groups was comparable.
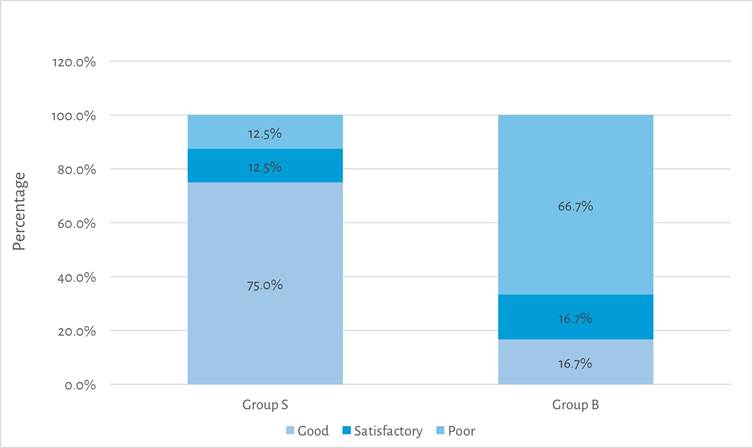
The mean POGO score for the two groups was similar (Table 1). In 75% of the patients in Group S intubation was completed in a single attempt, without any manipulations required; hence, the ease of intubation was good, in contrast to 66.7% of the patients in Group B in which another attempt - with or without manipulations -was required, resulting in poor intubating conditions.
Table 1 Demographics and POGO Scores of patients included.
| Variable | Group S (n=24) Mean ± SD | Group B (n=24) Mean ± SD | |
|---|---|---|---|
| Age (years ) | 41.96 ± 11.34 | 40.33 ± 13.83 | |
| Sex | Males | 16 | 14 |
| Females | 8 | 10 | |
| BMI (Kg/m2) | 26.87 ± 3.59 | 26.30 ± 3.76 | |
| POGO Score (%) | 89.58 ± 20.74 | 81.25 ± 24.73 | |
Source: Authors.
Figure 2 presents the comparison of ease of intubations between groups. The mean total time taken for intubation was shorter in Group S (26.83 ± 8.61s) as compared to Group B (47.18 ± 16.46 s). The total time required for intubation did not exceed 120s in either group (Table 2).
Table 2 Mean time required for intubation between groups.
| Time taken (sec) | Group S (n=24) Mean ± SD | Group B (n=24) Mean ± SD | p value |
|---|---|---|---|
| To visualize vocal cords | 9.36 ± 2.69 | 11.51 ± 5.76 | 0.03 |
| To pass the endotracheal tube | 17.44 ± 9.15 | 35.60 ± 11.74 | <0.001 |
| Total time | 26.83 ± 8.61 | 47.18 ± 16.46 | <0.001 |
Source: Authors.
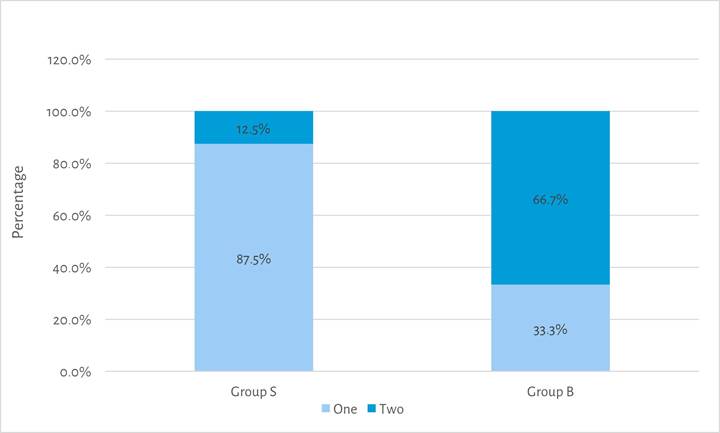
Fewer intubation attempts were required in Group S as compared to Group B (Figure 3). The maximum number of attempts in either group was two; consequently there was no need to switch over to the Macintosh blade in any of the cases.
Heart rate and blood pressure were recorded at baseline and at regular intervals after intubation; the results were comparable for both groups with no significant differences identified (Table 3).
Table 3 Hemodynamic parameters over time between groups.
| Time (min) | Group S (n =24) Mean ± SD | Group B (n =24) Mean ± SD | Pvalue |
|---|---|---|---|
| HEART RATE (bpm) | |||
| Baseline | 78.83 ± 13.35 | 82.67 ± 11.31 | 0.32 |
| 1 | 84.08 ± 13.73 | 86.71 ± 10.86 | 0.24 |
| 3 | 78.21 ± 10.15 | 80.83 ± 10.26 | 0.23 |
| 5 | 72.71 ± 9.22 | 78.88 ± 9.89 | 0.04 |
| 10 | 70.96 ± 10.55 | 76.63 ± 10.43 | 0.04 |
| 15 | 68.63 ± 7.77 | 76.04 ± 8.72 | 0.006 |
| SYSTOLIC BLOOD PRESSURE (mmHg) | |||
| Baseline | 134.92+/- 15.98 | 129.00 +/-10.39 | 0.27 |
| 1 | 137.33 +/-15.95 | 135.67 +/-16.78 | 0.80 |
| 3 | 120.67 +/-11.79 | 119.17 +/-14.19 | 0.76 |
| 5 | 110.88 +/-13.10 | 109.79 +/-10.28 | 0.84 |
| 10 | 106.33 +/-9.42 | 109.04 +/-12.48 | 0.33 |
| 15 | 105.96 +/- 9.99 | 108.58 +/-15.85 | 0.84 |
| DIASTOLIC BLOOD PRESSURE (mmHg) | |||
| Baseline | 72.04+/- 11.09 | 75.00 +/-12.79 | 0.52 |
| 1 | 75.29+/- 11.17 | 80.54+/-13.16 | 0.15 |
| 3 | 65.88 +/-6.58 | 69.96 +/-13.17 | 0.45 |
| 5 | 61.88 +/-9.39 | 65.38+/-8.84 | 0.14 |
| 10 | 64.04 +/-7.95 | 65.54+/-8.40 | 0.51 |
| 15 | 61.58+/- 7.25 | 67.04 +/-8.61 | 0.04 |
Source: Authors.
DISCUSSION
The C-MAC Macintosh blade video laryngoscopes are recognized as a valuable tool for both direct and indirect laryngoscopy in difficult airway scenarios such as limited cervical mobility 1,7-9. The D-blade with a higher angulation of 60° in contrast to the 18o original C-MAC Macintosh blade was designed as an alternative blade to address extremely difficult airway situations 1. Under such circumstances, the D-Blade can be quickly attached to the existing C-MAC system.
Cavus E et al., in their preliminary study of the C-MAC D-blade laryngoscope in routine and difficult airway situations reported the impossibility to achieve direct view of the glottis using the D-Blade. 1 An indirect view of the larynx may give optimal glottic visualization but may not always allow for the smooth advancement of the tube into the trachea, since the wider D-blade angle is not compatible with the endotracheal tubes used routinely. Hence, the authors concluded that while the C-MAC D-blade is excellent in extremely difficult airway conditions, a semi-flexible tube guide is required for successful intubation. 1
The reusable C-MAC stylet was introduced with an angle adapted to the blade shape of the D-blade to enable optimum placement of endotracheal tubes with the C-MAC D-blade video laryngoscopes. According to the literature, the use of a styletted endotracheal tube significantly reduces the intubation difficulty, especially in patients with cervical spine immobilization. 4,7-9
A gum elastic bougie is an inexpensive endotracheal tube introducer brought into clinical practice by Macintosh in 1949 and widely available 10. A bougie is reserved for difficult airway anatomy as a railroad for entry of the endotracheal tube into the trachea. 6 Studies have shown that the bougie improves the chances of first attempt intubation success even when compared to a stylet guide. 11
Few trials have studied the outcomes of the use of the two intubating aids with the C-MAC D-blade laryngoscope. One of such studies was conducted by Batuwitage B et al., in a SimMan 3G manikin, and suggested that the introducer strategy was favorable for intubation with the C-MAC D-blade laryngoscope. However, they found that stylets and bougies performed similarly in both easy and difficult airway simulations. 6 Another study by Tosh P et al., in surgical patients found that the 60° angled stylet was better than a bougie as an intubating aid. (5_) Hence, we decided to compare the 60° angled stylet with a gum elastic bougie while intubating with a C-MAC D-blade in patients undergoing elective surgery under general anesthesia. Since the C-MAC D-blade is designed for managing difficult airways, we simulated a difficult airway by manual in-line cervical stabilization.
Our study found that intubation was easier in 75% of patients in group S compared to only 16.7% of patients in group B. The success rate on the first attempt was 87.5% in group S compared to 33.3% in group B and the total time for intubation was lower in group S versus group B. Similarly, Tosh P et al. compared 60° angled stylet versus bougie with the C-MAC D-blade video laryngoscope and showed that intubation was substantially easier with the stylet (88.6%) versus a bougie (25.7%). (5) The intubation procedure was shorter with the stylet than with a bougie and the success rate on the first attempt was 94.3% with stylet versus 5.7% with bougie. The ease of intubation and first attempt success rate was better with stylet compared to bougie mostly because the stylet curvature is designed specifically for the C-MAC D-blade video laryngoscope, so that the endotracheal tube passes easily into the glottis with minimal manipulations. The bougie used in the study was only angulated at the tip, with the remainder of the body being linear; therefore, the tip of the bougie was frequently posterior to the arytenoid cartilage during laryngoscopy, making it difficult and time consuming to manipulate it into the glottis. In our experience, the use of maneuvers such as external laryngeal manipulation and partial withdrawal of the D-blade video laryngoscope helps to accomplish a faster intubation with a bougie.
Batuwitage B et al., found that even though stylet introducers shorten intubation times, this difference was not clinically significant as compared to a bougie introducer and hence they inferred that both stylet and bougie are comparable in their performance as intubating aids in easy and difficult laryngoscopy conditions. 6 This difference in the outcomes may be due to the fact that the study was conducted on manikins while our study and the study by Tosh P et al., were in surgical patients.
In the study by Tosh P et al., the stylet resulted in better attenuation of hemodynamic responses to intubation compared to a bougie 5. There were no differences in terms of hemodynamic responses to intubation between the two groups in our study. This may be because although the bougie-guided intubation took longer, none of the intubations exceeded 120s and no more than two attempts were used in any patient. Hence, in the absence of a 60° angled stylet to aid intubation via the C-MAC D-blade video laryngoscope, a bougie is a good option to consider. According to Tosh P et al., there may be a risk of losing the airway when a styletted endotracheal tube is used while pulling out the stylet with just the tip of the tube inside the larynx (5!; however, we did not experience such challenges in our study with the use of the styletted endotracheal tube. They also referred to the potential risk of damage or perforation of the trachea, bronchi or even the esophagus when a bougie is used because of its stiffness; nonetheless, we did not experience any of those complications in our study.
Although it is acceptable to extrapolate this study to individuals with cervical spine instability, that subgroup of patients should be further evaluated considering that our study was based on patients with normal cervical anatomy. Another limitation of our study is that the procedure was performed by an anesthesiologist previously trained with the C-MAC D-blade video laryngoscope. Hence, the results may differ in the hands of inexperienced anesthesiologists.
In conclusion, it is possible to intubate using the C-MAC D-blade video laryngoscope in 120 s in anesthetized paralyzed adults, with simulated restricted cervical mobility using intubating aids like the 60° angled stylet or bougie. The stylet results in easier and faster intubation and requires less intubation attempts as compared to the bougie.
ETHICAL DISCLOSURES
Ethics committee approval
This study was started only after approval from the Institutional Ethics Committee (Kasturba Medical College and Kasturba Hospital on 10/08/2019 as recorded in act no. IEC:766/2019.The study was also registered under Clinical trial registration of India (CTRI/2020/09/027672).
Protection of human and animal subjects
The authors declare that no experiments were performed on animals for this study. The authors declare that the procedures followed were in accordance with the regulations of the relevant clinical research ethics committee and with those of the Code of Ethics of the World Medical Association (Declaration of Helsinki).
Confidentiality of data
The authors declare that they have followed the protocols of their work center on the publication of patient data.
Right to privacy and informed consent
The authors declare that no patient data are disclosed in this article.
Contributions by the authors
NSM: Conception of the original project, study planning, data collection and analysis.
NV: Literature search, initial writing of the manuscript, final writing of manuscript, review of final manuscript.
RRK: Conception of the original Project, Study planning, data collection and analysis interpretation of results and final writing of the manuscript.











 text in
text in