Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO -
 Access statistics
Access statistics
Related links
-
 Cited by Google
Cited by Google -
 Similars in
SciELO
Similars in
SciELO -
 Similars in Google
Similars in Google
Share
Revista colombiana de Gastroenterología
Print version ISSN 0120-9957
Rev Col Gastroenterol vol.30 no.4 Bogotá Oct./Dec. 2015
Literature Review: A Surgeon's View of Recurrent Hiatal Hernia
Cáterin Arévalo MD. (1), Rubén D. Luna MD. (2), Carlos A. Luna-Jaspe MD.(3), Felipe Bernal MD.3, Bernardo A. Borráez Segura MD. (4)
(1) General Surgery Resident at the University of Sinu in Cartagena de Indias, Colombia.
(2) Department of General Surgery at Fundación Clínica Shaio in Bogotá, Colombia.
(3) Department of General Surgery at Universidad El Bosque in Bogotá, Colombia.
(4) Gastrointestinal Surgery in the Department of General Surgery of the University of Chicago and at Fundación Clínica Shaio in Bogotá, Colombia. bborraez@hotmail.com
Received: 16-01-15 Accepted: 20-10-15
Abstract
Recurrent hiatal hernias are a common pathology that generate a diagnostic and therapeutic challenge for surgeons and gastroenterologists. They are generally asymptomatic or present with atypical symptoms and are associated with the patient's own physiological factors and the surgical technique. Treatment is complex and, depending on the cause of the symptoms, will require either medical or surgical management. This article starts from a surgical approach to define guidelines for identification and management of this condition and to establish keys to treatment.
Keywords
Hiatal hernia, recurrent hiatal hernia, laparoscopy
INTRODUCTION
Surgery for treatment of hiatal hernias is a challenge for the surgeon that requires extensive knowledge of the anatomy of the gastroesophageal junction and the esophageal hiatus. Laparoscopic repair is the standard treatment, but it demands a wide esophageal dissection, adequate hiatal closure and an anti-reflux mechanism. Physiological factors associated with conditions of the patient, the surgical technique used, and the surgeon's experience all play important roles in the high rate of recurrence.
Treatment of recurrent hernias generates a challenge. Treatment can include methods with many possible complications that can lead to esophageal or gastric perforation and that can even require more complex procedures such as esophagogastrectomies.
This article's aim is to define guidelines for identifying and managing this disease and to establish treatment options from the point of view of laparoscopic and gastrointestinal surgeons.
SEARCH STRATEGIES
Literature found in Infomed was reviewed. Infomed includes Scielo, MEDLINE, LILACS, Hinari, Pubmed, PubMed Central and Virtual Health Library. The following keywords were used: recurrence, hiatal hernia, para-esophageal hernia, reoperation, surgical techniques, scientific journals, scientific publications, guides, tools, scientific communication. In addition, the Boolean operators "and" and "or" were used. EndNote was used as the library manager.
CLASSIFICATION AND DEFINITION
Unlike primary hiatal hernias, recurring hernias do not have clear and uniform classifications. In their absence, several points should be considered (1):
- Primary hernias differ in anatomical terms and clinical presentation from recurrent hernias with similar characteristics (2-4).
- Surgical repair of primary hernias requires releasing attachments associated with the formation of postoperative adhesions that can cause slippage of the gastroesophageal junction through the hiatus. This slippage can be evident in an esophagogram but without evident symptoms or with minimal symptoms (5).
- When repairing a primary hiatal hernia, fundoplication, usually 360 degree, is commonly performed. If correctly done, it should involve the gastric fundus. Thus, any slippage of the gastroesophageal junction through the hiatus involves the stomach and causes a para-esophageal hiatal hernia (6).
- Some authors define recurrent hiatal hernias as those that appear to over 2 cm in radiological studies (7).
- According to the literature, the size of primary hiatal hernias can be classified as large when they are indirectly measured through radiology as being larger than 5cm or when the mediastinum contains more than one third or half of the stomach. When measured by endoscopy, hiatal hernias are classified as large when they are over 6 cm (8-10).
Given these considerations, even though recurrent hiatal hernias are not equivalent to primary hiatal hernias, treatment of them requires extrapolation of the characteristics of primary hiatal hernias. For practical purposes, we define recurrent hiatal hernias as any hernia that occurs after the repair of a primary hiatal hernia. Recurrent hiatal hernias are not all the same. There are four types (I-IV), and the size and symptoms of each can vary. Also volvulus may or may not be present. All of these factors must be taken into account in the establishment of treatment guidelines (11).
EPIDEMIOLOGY
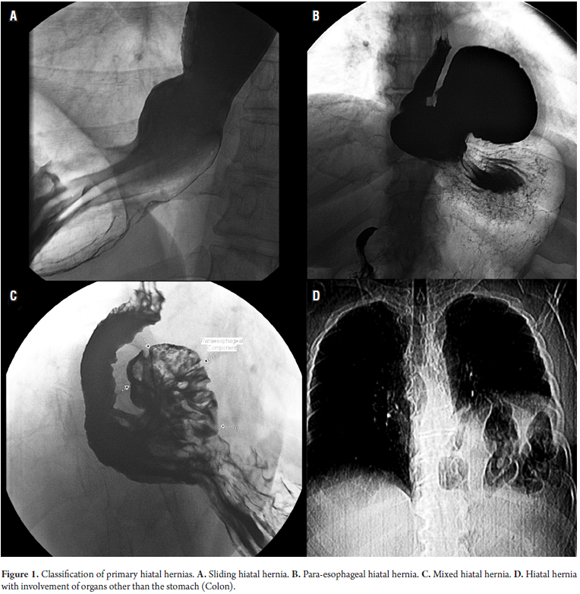
More than 95% of primary hiatal hernias are Type I sliding hernias. Types II, III and IV are grouped as para-esophageal hernias. Of these, over 90% are type III. Type II is the least common (Figure 1) (12).
In general terms, postoperative symptoms of primary Type I hiatal hernias must be distinguished as resulting from:
- Failure of an anti-reflux procedure. Fundoplication may fail in 25% to 35% of cases due to incorrect construction (13).
- Recurrence of a hiatal hernia (2-4).
The incidence of recurrence of hiatal hernia after repair of a primary sliding hiatal hernia in patients with gastroesophageal reflux is difficult to determine since not all patients who have undergone anti-reflux surgery have had esophagograms prior to the procedure, and since sometimes patients develop sliding hiatal hernias as the result of the release of attachments during surgery (5). Contrast radiology following these procedures has demonstrated a rate of recurrence over 50% in generally asymptomatic patients (1).
Rates from 2% to 42% have been reported for recurrence of para-esophageal hiatal hernias, but the types of procedures performed and the follow-up times vary widely (6). Papasavas et al. have reported on 120 patients who underwent surgery for para-esophageal hiatal hernias and whose average follow-up time was 15 months. They reported that thirty of these patients (25%) suffered recurrences, but only four, thirteen percent of the patients whose hernias recurred and 3% of the patients who had undergone surgery, required new procedures (14).
A study by White et al. of 31 patients with an average 11.3 years follow-up found that the hiatal hernias of 10 patients (32%) recurred according to radiological recurrence but that only two patients (6.5%) required another procedure to repair their hernias (15). A study by Oelschlager et al. of 60 patients with average follow-ups of 58 months (4.8 years) reported that 34 patients (57%) had radiological evidence of recurrence, but only two of these (3%) had to be reoperated (5). These studies suggest a high rate of relapse with a direct relationship to the length of time after the original procedure, but also suggest that very few patients require a new procedure.
ETIOPATHOGENESIS
The pathophysiologies of primary hiatal hernias and recurrent hiatal hernias are not entirely clear. Although the molecular and cellular bases have not been fully described, differences among patients with hiatal hernias point to either congenital or acquired defects (16). There are several factors that influence recurrence (16, 17).
Patient factors
- Negative pressure in the chest and positive pressure in the abdomen.
- Intra-abdominal pressure (associated comorbidities: pulmonary diseases and being overweight)
- Patient age (young patients = prolonged exposure).
Factors related to the hernia itself and to the gastroesophageal junction
- Size of the esophageal hiatus (difficult to approach pillars of tendon).
- Fibrous scar tissue from previous procedure.
- A short esophagus.
Factors related to surgical technique
- Inadequate dissection of the esophagus at the time of primary repair.
- Incomplete release of the hernia sac.
- Inadequate closure and low hiatal pressure (4, 13, 18-24).
PRESURGICAL EVALUATION
Clinical presentation
As the stomach moves into the chest, respiratory symptoms may predominate as a result of a lung compression and decreased forced vital capacity (FVC) (25, 26). Dysphagia and postprandial fullness occur as the result of esophageal compression and expansion of the herniated stomach as it moves into the chest (27).
Clinical presentation varies, but symptoms include epigastric pain, chest pain, dysphagia, early satiety and regurgitation. These symptoms result from compromised volume of the stomach and the anatomical orientation it adopts within the mediastinum. In addition, a long lasting hernia may lead to development of obstruction, volvulus and strangulation (10).
The risk that an asymptomatic para-esophageal hernia will become symptomatic is about 14% per year with an annual incidence of acute obstruction of 1.1% (10).
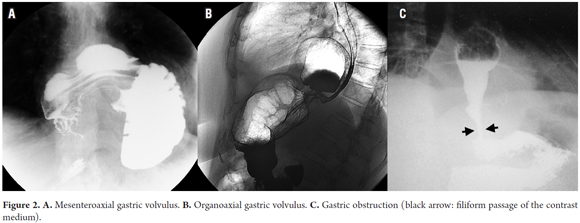
Meanwhile volvulus is a rare condition that is characterized by twisting of the stomach. It is associated with para-esophageal hiatal hernias and is most frequently diagnosed in older adults. It has progressive symptoms such as chest pain, severe vomiting and epigastric bloating. Other symptoms resulting from total obstruction can occur in what is called Borchardt's triad. They consist of severe epigastric pain, retching without vomiting, and inability to pass a nasogastric tube (Figure 2).
Diagnosis
Radiological studies are done first in patients suspected of recurrence (1).
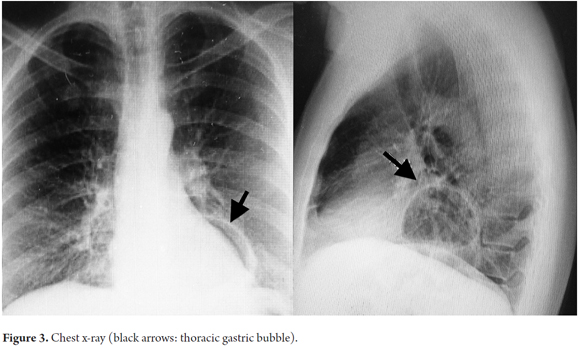
- Chest x-ray opacity is a pathognomonic sign for para-esophageal hernias that is evidence of retrocardiac air corresponding to the gastric bubble. In cases of intestinal hernias and the presence of the colon you can see visceral gas and layers of intestine with unusual patterns in the hernia sac (Figure 3) (29).
- An esophagram is a basic contrast study that has fallen into disuse. Nevertheless, it is a necessary tool for gastroesophageal and hiatal diseases and disorders. It can be used to measure the size and morphology of the hernia and to determine whether or not there is an obstruction. In addition, it can show the location of the gastroesophageal junction in relation to the esophageal hiatus.
- It should be noted that the risk of aspiration of the contrast medium is high when there is an obstruction (15).
- CT scans can show the hernia and the involvement of other organs within the chest cavity. If there is obstruction, fluid levels can be observed within the abdominal and thoracic cavities (30).
- Endoscopy provides additional information about the size, characteristics and type of hernia. Difficulty of reaching the duodenum combined with stomach orientation can suggest volvulus. Endoscopy also allows evaluation of the esophagogastric junction and determination whether there are concomitant diseases secondary to reflux.
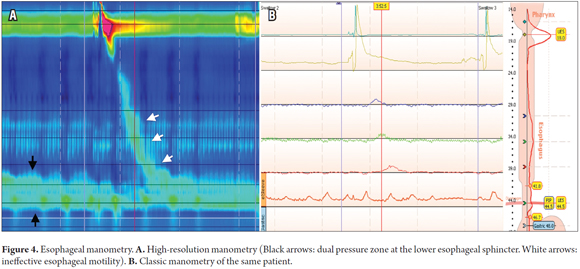
- High resolution esophageal manometry can show a double zone of pressure zone on the lower esophageal sphincter and can provide information on esophageal motility in patients with ineffective esophageal motility (Figure 4) (31, 32).
- pH monitoring is not relevant for diagnosis of hiatal hernias, but it can confirm acid exposure in patients who could benefit from medical management or who may require a new procedure.
TREATMENT
Treatment of recurrent hiatal hernias is a challenge for gastroenterologists and surgeons that requires evaluation of multiple factors.
The first factors that require consideration are the severity of symptoms and the time of presentation. In patients with severe acute or progressive symptoms associated with signs of obstruction, incarceration, ischemia and necrosis should be suspected. In these cases urgent surgical management is the treatment of choice given the high risk of perforation. Complementary studies should be limited since they delay treatment (33).
Laparoscopy is also the approach of choice in patients with acute symptoms. Parker and colleagues reported that patients with acute and severe para-esophageal hiatal hernias have similar results in terms of mortality with zero cases requiring open surgery. Patients treated were older people with multiple comorbidities that could influence hospital stays and morbidity (34).
In patients with acute symptoms with small hiatal hernias it is necessary to rule out other types of pathologies with differential diagnosis.
The factors to consider include anatomy, size of the hernia and the disposition of the stomach (presence or absence of gastric volvulus).
In patients with small asymptomatic hernias, one must consider the possibility that images show postoperative changes. We consider it necessary to monitor symptoms in order to define whether additional tests and studies are needed.
The clinical presentation of small hernias in symptomatic patients can vary. Patients with atypical symptoms should be studied to rule out heart diseases, pulmonary diseases and other diseases of the gastrointestinal tract. Esophageal manometry and 24 hour pH monitoring play important roles in assessment of esophageal motility disorders and reflux. For reflux, medical management with proton pump inhibitors constitutes the initial treatment of choice.
When medical management only poorly or partially controls symptoms in patients for whom other diagnoses have been excluded, the physician must whether or not reoperation is the correct management.
Large recurrent hiatal hernias are a topic of discussion because of the precept that all primary para-esophageal hiatal hernias, whether symptomatic or not, must be corrected. Oelschlager et al. reviewed 95 patients from four different medical institutions who had had hiatal hernias corrected. Radiology six months after surgery showed that 13 of these patients (14%) had had recurrences. Long term monitoring (58 months on average) found that found a recurrence rate of 57% verified by esophagrams.
Twenty of these patients with long-term follow-up (33%) had hernias larger than 4 cm and symptoms of heartburn that were more severe than those of the other patients. Only two patients required surgical repair on the basis of symptoms rather than on the size of the hernia. These findings confirm the exponential growth of the recurrence rate over time, but call into question the need for surgery in all patients with large recurrent hiatal hernias when gastric volvulus is not present (5). Despite this, the rate of exacerbation and the need for urgent surgery increases over the years. Because of this risk of exacerbation, we believe that surgical treatment, rather than merely treating the symptoms, is necessary for young patients.
Two types of populations require independent evaluations. The first group consists of elderly patients with multiple comorbidities.
Spaniolas et al. studied 2,681 patients who underwent elective laparoscopic surgical procedures. Three hundred and thirteen of these patients were 80 years old or over, but the study found no statistically significant differences in terms of morbidity or mortality (35). These results contrast with those of Parker et al. who reported longer hospital stays, more associated comorbidities and more acute interventions among elderly patients (34). We believe that asymptomatic elderly patients and those with mild symptoms who do not have significant comorbidities should be evaluated to define the possibility of surgery. Medical management is the right choice for patients with multiple comorbidities with criteria of inoperability and no signs of obstruction or worsening symptoms.
The second group that requires special considerations consists of obese patients. The reports of Che and colleagues about morbidly obese patients say that 37% of these patients had hiatal hernias and 40% had gastroesophageal reflux (36).
For patients who have had hiatal hernias corrected, increased abdominal pressure and fatty infiltration of the gastroesophageal junction are parts of the pathophysiology of relapse (37).
Initial treatment of overweight and obese patients with recurrent hiatal hernias who have mild or moderate symptoms is based on weight loss combined with medical management. Surgical treatment of these patients aims at correcting the hernia and treating obesity. Studies by Chaudhry et al. and Mahawar et al. show symptomatic improvement resulting from both gastric bypass and gastric sleeve procedures, the two most common procedures for managing obesity (38-40).
We consider gastric bypass to be the best procedure in terms of controlling symptoms because acid production is discontinuous and weight loss is greater. Nevertheless, regardless of the procedure chosen, it must produce a tension free closure of the hiatus with proper mobilization of the distal esophagus.
TECHNICAL CONSIDERATIONS AND AUTHORS' RECOMMENDATIONS
In general, surgical treatment of recurring hiatal hernias is similar to that for primary hernias but has some special considerations.
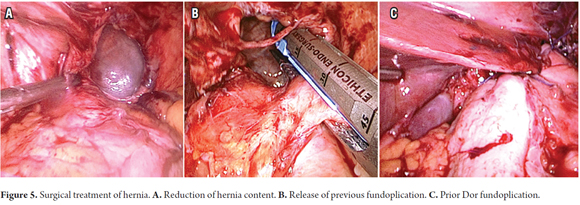
Returning hernia contents into the abdomen. Reducing the hernia contents must be done gently because of the risk of perforation. The herniated organ should be thoroughly reviewed in order to avoid overlooking areas of ischemia or necrosis (Figure 5).
Excision of hernia sac and release of adhesions. This critical step is misunderstood by some surgeons because many times the sack consists of mediastinal structures such as the pleura. Based on our combined personal experience, we consider that this step requires more than simply the excision of the sac. This must be done while completely disconnecting the abdominal structures to avoid pressure toward the mediastinum.
Undo previous fundoplication. Prior fundoplication may be associated with the patient's symptoms, so it is necessary to completely undo old procedures for proper mobilization of the esophagus and completion of a new anti-reflux procedure. It should be noted that some surgeons fix the fundoplication to the esophagus, so sometimes it is necessary to cut and staple to completely release the cover (Figure 5).
Mobilization of the Esophagus. At least 3cms below the esophageal hiatus without tension-must be obtained for maximum possibility of avoiding another relapse. This dissection should be done with caution given the high risk of esophageal perforation.
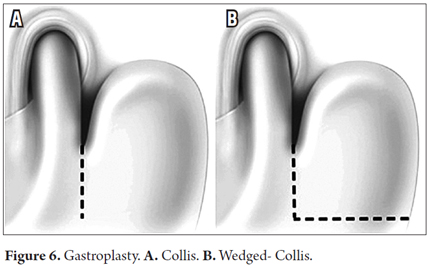
If appropriate dissection is not achieved, a Collis gastroplasty or stapled-wedge Collis gastroplasty will become necessary to achieve an elongation of the esophagus and reduce the stress and strain on the mediastinum (Figure 6).
Withdrawal of synthetics. To the extent possible, the meshes placed in previous procedures must be removed while avoiding further damage. These old meshes do not fulfill any function, but their presence can cause complications such as migration through planes of least resistance and perforations.
Hiatal closure. The tension-free closure of the esophageal hiatus is the first priority of the procedure. The authors prefer initial closure with separated sutures, using a sliding knot to reduce tension. Completion of the closure is then accomplished with many individual separated sutures. Care must be taken to avoid creating angulation or obstruction.
The use of meshes is controversial given the evidence that there is no significant difference in terms of long-term reproduction and the evidence of complications associated with meshes. We believe that if adequate primary closure cannot be achieved, the use of mesh is indicated. It should cover relaxing incisions in the right diaphragm and not on the hiatus.
Anti-reflux procedure. The selection of anti-reflux procedure can protect against the development of future hernias and fix the stomach to the hiatus to limit new migration. The surgeon's decision may be influenced by her or his experience in the use of different techniques.
The authors prefer performance of a Dor partial fundoplication which provides a means of attachment in multiple zones of the hiatus similar to gastropexy and which completely covers the defect (Figure 5).
CONCLUSIONS
Treatment of recurrent hiatal hernias is a challenge for gastroenterologists and surgeons that requires adequate training and extensive knowledge of the anatomy of the gastroesophageal junction and the esophageal hiatus. The multifactorial etiology and broad spectrum of presentation of recurrent hiatal hernias impede diagnosis and study and require extensive diagnostic suspicion and one or more complementary studies depending on the presentation. The authors consider laparoscopic repair to be the standard treatment for patients whether or not they have acute symptoms of obstruction. Laparoscopic repair has proven to be an excellent technique with good to excellent results in most cases.
REFERENCES
1. White BC JL, Morgenthal CB, Zagorski S, Davis SS, Smith CD, et al. Do recurrences after paraesophageal hernia repair matter?: Ten-year follow-up after laparoscopic repair. Surg Endosc. 2008;22(4):1107-11. [ Links ]
2. Coelho JC GC, Claus CM, Andrigueto PC, Ribeiro MN. Late laparoscopic reoperation of failed antireflux procedures. Surg Laparosc Endosc Percutan Tech. 2004;14(3):113-7. [ Links ]
3. Musunuru SGJ. Perioperative outcomes of surgical procedures for symptomatic fundiplication failure: a restrospective case-control study. Surg Endosc. 2012;26(3):838-42. [ Links ]
4. Smith CD, Rajad MA, Lederman AB, Hunter JG. When fundoplication fails: redo? Ann Surg. 2005;241(6):861-9. [ Links ]
5. Oelschlager BK PR, Brunt LM, Soper NJ, Sheppard BC, Mitsumori L, et al. Laparoscopic paraesophageal hernia repair: Defining long-term clinical and anatomic outcomes. J Gastrointest Surg. 2012;16(3):453-9. [ Links ]
6. Landreneau RJ, Santos R Management of paraesophageal hernias. Surg Clin North Am. 2005;85:411-32. [ Links ]
7. Oelschlager BK, Hunter JG, Brunt ML, Soper NJ, Sheppard BC, et al. Biologic prosthesis to prevent recurrence after laparoscopic paraesophageal hernia repair: long-term follow-up from a multicenter, prospective, randomized trial. J Am Coll Surg. 2011;4:461-8. [ Links ]
8. Morino M GC, Pellegrino L, Rebecchi F. Laparoscopic management of giant hiatal hernia: factors influencing long-term outcome. Surg Endosc. 2006;20(7):1011-6. [ Links ]
9. Skinner DB BR. Surgical management of esophageal reflux and hiatus hernia. Long-term results with 1,030 patients. J Thorac Cardiovasc Surg. 1967;53(1):33-54. [ Links ]
10. Treacy PJ. An approach to the management of para-oesopageal hiatus hernias. Aust N Z J Surg. 1987;57:813-7. [ Links ]
11. Brant K. Oelschlager RBYM. Management of Minimally Symptomatic Recurrent Hiatal Hernia. In: Springer, editor. Difficult Decisions in Thoracic Surgery. 2014. p. 511-28. [ Links ]
12. Hutter MM. Paraesophageal and other complex diaphragmatic hernias. In: CJ Y, editor. Shackelford's surgery of the alimentary tract. Philadelphia: Saunders Elsevier; 2007. p. 549-62. [ Links ]
13. Edye MB CEJ, Gattorno F, Salky BA Durability of laparoscopic repair of paraesophageal hernia. Ann Surg. 1998;228:528-35. [ Links ]
14. Papasavas PK, Robke J, Raftopoulos Y, Gagné DJ, et al. Laparoscopic repair of large paraeophageal hernia is associated with a low incidence of recurrence and reoperation. Surg Endosc. 2004;18:444-7. [ Links ]
15. Morcos SK. Review article: Effects of radiographic contrast media on the lung. Br J Radiol. 2003;76(905):290-5. [ Links ]
16. Curci JA ML, Thompson RW, Soper NJ, Matthews BD. Elastic fiber depletion in the supporting ligaments of the astroesophageal junction: a structural basis for the gastroesophageal junction: a structural basis for the development of hiatal hernia. J Am Coll Surg. 2008;207:191-6. [ Links ]
17. Beglaj SM. Paraesophageal hernia in children: familial occurrence and review of the literature. Pediatr Surg Int. 1999;15:85-7. [ Links ]
18. Geoffrey PK RR, Steven RD, Jorg Z, Oliver JM, Zuad A, et al. Guidelines for the management of hiatal hernia. Surg Endosc. 2013;27:4409-28. [ Links ]
19. Mattar SG, Galloway KD, Hunter JG, Smith CD. Long-term outcome of laparoscopic repair of paraesophageal hernia. Surg Endosc. 2002;16(5):745-9. [ Links ]
20. Hashemi M PJ, DeMeester TR, Huprich JE, Quek M, Hagen JA, et al. Laparoscopic repair of large type III hiatal hernia: objective followup reveals high recurrence rate. J Am Coll Surg. 2000;190(5):553-60. [ Links ]
21. Perez AR, Rattner DW Obesity adversely affects the outcome of antireflux operations. Surg Endosc. 2001;15:986-9. [ Links ]
22. Aly A, Jamieson GG, Ludemann R, Devitt PG, Watson DI. Laparoscopic repair of large hiatal hernias. Br J Surg. 2005;92:648-53. [ Links ]
23. Shamiyeh A, Granderath FA, Syre G, Wayand W, Zehetner J. The esophageal hiatus: what is the normal size?. surg Endosc. 2010;24:988-91. [ Links ]
24. Braghetto I, Csendes A, Burdiles P, Valladares H, Brunet L Postoperative results after laparoscopic approach for treatment of large hiatal hernias: is mesh always needed? Is the addition of an antireflux procedure necessary?. Int Surg. 2010;95:80-7. [ Links ]
25. Low DE. Effect of paraesophageal hernia repair on pulmonary function. Ann Thorac Surg. 2002;74:333-7. [ Links ]
26. Awais O. Management of giant paraesophageal hernia. Minerva Chir. 2009;64:159-68. [ Links ]
27. Hunter JG, Branum GD, Waring JP, Trus TL, Cornwell M, et al. Laparoscopic fundoplication failures: patterns of failure and response to fundoplication revision. Ann Surg. 1999;230:595-604. [ Links ]
28. Cardile AP. Gastric volvulus, Borchardt's triad, and endoscopy: a rare twist. Hawaii Med J. 2011;70:80-2. [ Links ]
29. Eren S, Okur A. A rare cause of intestinal obstruction in the adult: Morgagni's hernia. Hernia. 2003;7:97-9. [ Links ]
30. Gourgiotis S, Germanos S, Baratsis S. Acute gastric volvulus: diagnosis and management over 10 years. Dig Surg. 2006;23:169-72. [ Links ]
31. Swanstrom LL, Kinzie LR, Horvath KD. Esophageal motility and outcomes following laparoscopic paraesophageal hernia repair and fundoplication. Am J Surg. 1999;177:359-63. [ Links ]
32. Boushey RP, Burpee S, Schlachta CM, Poulin EC, Haggar F, et al. Laparoscopic repair of paraesophageal hernias: a Canadian experience. Can J Surg. 2008;51:355-60. [ Links ]
33. Shafii AE, Zervos EE. Perforated gastric corpus in a strangulated paraesophageal hernia: a case report. J Med Case Reports. 2009;3:6507. [ Links ]
34. Parker DM, Johanson K, Ibele A, Gabrielsen JD, Petrick AT. Urgent laparoscopic repair of acutely symptomatic PEH is safe and effective. Surg Endosc. 2013;27(11):4081-6. [ Links ]
35. Spaniolas K, Adrales GL, Trus TL. Laparoscopic paraesophageal hernia repair: advanced age is associated with minor but not major morbidity or mortality. J Am Coll Surg. 2014;218(6):1187-92. [ Links ]
36. Che F, Cohen A, Nguyen NT. Prevalence of hiatal hernia in the morbidly obese. Surg Obes Relat Dis. 2013;9(6):920-4. [ Links ]
37. Pandolfino JE, El-Serag HB, Zhang Q, Shah N, Ghosh SK, Kahrilas PJ. Obesity: a challenge to esophagogastric junction integrity. Gastroenterology. 2006;130(3):639-49. [ Links ]
38. Chaudhry UI, Marr BM, Osayi SN, Mikami DJ, Needleman BJ, Melvin WS, et al. Laparoscopic Roux-en-Y gastric bypass for treatment of symptomatic paraesophageal hernia in the morbidly obese: medium-term results. Surg Obes Relat Dis. 2014;10(6):1063-7. [ Links ]
39. Mahawar KK, Jennings N, Balupuri S, Small PK. Simultaneous Sleeve Gastrectomy and Hiatus Hernia Repair: a Systematic Review. Obes Surg. 2014;19(6):761-3. [ Links ]
40. Jobe BA AR, Deveney CW, Domreis JS, Hill LD. Laparoscopic management of giant type III hiatal hernia and short esophagus. Objective follow-up at three years. J Gastrointest Surg. 2002;6(2):181-8. [ Links ]











 text in
text in